Thyroid nodules are commonly encountered in clinical practice. The estimated prevalence, using thyroid palpation for diagnosis is 3-7%.1 In the Philippines, the estimated prevalence of nodular goiter is 4%.2 Thyroid nodules are more common in women, in the elderly, in those with iodine deficiency, and in those with history of radiation exposure.1 They can either be benign or malignant. Thus, it is importance to exclude malignancy in newly diagnosed thyroid nodules.
The evaluation of a thyroid nodule begins with a complete history, physical examination and thyroid sonography focusing on the thyroid gland and cervical lymph nodes. Factors suggestive of an increased risk of malignancy have been enumerated in previous studies. 1,3
Fine-needle aspiration biopsy (FNAB) is the most accurate and cost-effective method for evaluating thyroid nodules.1 The results of FNAB are critical in deciding whether to manage the nodule(s) medically or surgically. FNAB decreases the rate of unnecessary operations in patients with benign nodules and helps to direct patients positive for malignancy to the appropriate definitive surgical procedure. Guidelines have been issued on how to select thyroid nodules for FNAB.1,4
Traditionally, FNAB results are divided into five (5) categories: non-diagnostic, benign, follicular lesions or indeterminate cytology, suspicious for malignancy, and malignant.1 However, classification and reporting systems for thyroid FNAB results are not standardized across institutions.
The classification of “indeterminate” lesions in thyroid cytology has long been a source of confusion for both pathologists and clinicians. There is great variability in the way cytopathologists identify, interpret and report such aspirates, especially when the uncertainty relates to follicular lesions. Clinicians have tended to lump interpretations such as “follicular lesion,” “atypical,” “follicular neoplasm,” “indeterminate for neoplasia,” and “suspicious for malignancy” into a single “indeterminate for malignancy” category for conceptual and even management purposes.5 Follow-up studies, however, have shown significantly different clinical outcomes for distinct subcategories within the generic indeterminate category.5
Thus in 2007, a revised classification system for reporting thyroid FNAB cytology was proposed at the National Cancer Institute State of Science Conference. This led to the Bethesda System for Reporting Thyroid Cytopathology, which provides a revised six-tiered reporting system, with an emphasis on the risk of malignancy associated with each category (Table 1).5
Click here to download Table 1
Table 1. The Bethesda System for Reporting Thyroid Cytopathology: Recommended Diagnostic Categories, Risk of Malignancy and Usual Management 5

The primary purpose of terminology is for clarity of communication. The interpretation should provide clinically relevant information that will assist referring physicians in the management of patients. The indeterminate classification of the traditional system was divided into 1) atypia or follicular lesion of undetermined significance (AUS of FLUS) and 2) follicular neoplasm or suspicious for follicular neoplasm.
The AUS or FLUS subgroup “is a heterogeneous category that includes cases in which the cytologic findings are not convincingly benign, yet the degree of cellular or architectural atypia is not sufficient enough for an interpretation of follicular neoplasm.”6
It is recommended that the patients in the AUS or FLUS category undergo a repeat FNAB at an appropriate interval.4 In most cases, a repeated FNAB results in a more definite interpretation, which may decrease the risk of unnecessary surgery. However, controversy in the management and risk for malignancy varies among institutions.
The risk of malignancy for an AUS or FLUS nodule is difficult to ascertain because only a minority of cases in this category undergo surgery, for which a definite histopathologic diagnosis can be made. The extrapolated estimate for risk for malignancy is estimated at 5% to 15%.4
A cytologic reading of AUS or FLUS is a controversial category in thyroid fine-needle aspiration, not only for its questionable clinical utility, but also for its expression of uncertainty.7
1. To describe the clinical data of patients who underwent FNAB of thyroid nodule with a cytologic diagnosis of AUS or FLUS at St. Luke’s Medical Center from January 2012 to October 2013 in terms of the following:
a. Demographic features (age, sex)
b. Sonographic characteristics of thyroid nodule (size, character, echogenicity, margins, calcification and vascularity)
c. Cytologic characteristics or sub-category (scenarios for which an AUS interpretation is appropriate as stated in the Bethesda System for Reporting Thyroid Cytopathology)
2. To determine the outcomes of these patients in terms of the following:
a. Cytologic sub-category of atypia according to the Bethesda System
b. Management of these patients (follow-up, repeat FNAB or surgery)
c. Repeat cytologic or final histopathologic result
3. To compare the sonographic characteristics and cytologic features of an AUS or FLUS thyroid nodule with malignant histopathology against those with benign results.
A descriptive cross sectional study was conducted to determine the clinical characteristics, management and outcome of adult patients who underwent FNAB of thyroid nodule, with a cytologic diagnosis of atypia or follicular lesion of undetermined significance.
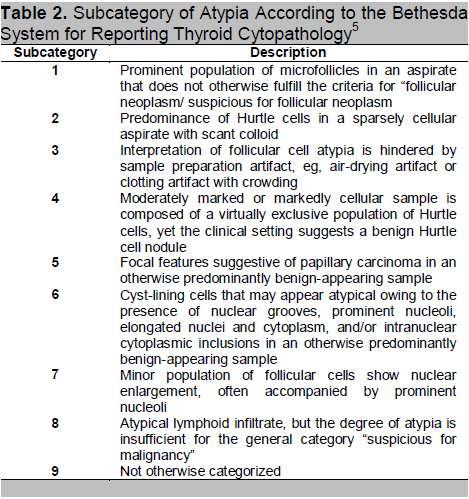
The census of the Pathology Department and Diabetes, Thyroid and Endocrine Center of St. Luke’s Medical Center, Quezon City and Global City, from January 2012 to October 2013 were reviewed. The cytologic diagnosis of those who underwent FNAB of thyroid nodule was determined through the electronic Healthcare-Results Management System of St. Luke’s Medical Center. Based on the microscopic description stated in the report, one cytopathologist subcategorized the form of atypia, using the most common scenarios as mentioned in the Bethesda System for Reporting Thyroid Cytopathology (Table 2). The corresponding ultrasound of the thyroid, initial consultation form and operative techniques were also reviewed. When the sonographic characteristics of the thyroid nodule are not completely reported, one sonologist reviewed the ultrasound images. Patients whose records were incomplete were contacted by telephone to supply the missing data. Those who could not be contacted were considered lost to follow-up.
Click here to download Table2
Table 2. Subcategory of Atypia According to the Bethesda System for Reporting Thyroid Cytopathology5
To be included in the study, the subject must be between 18-85 years old, who underwent fine-needle aspiration biopsy of the thyroid nodule and have a cytologic diagnosis of atypia or follicular lesion of undetermined significance, as defined by the Bethesda System proposed by the National Cancer Institute (NCI). This included FNABs interpreted as “atypical cells,” “atypia of undetermined significance,” “follicular lesion of undetermined significance,” and “cellular follicular lesion.”
A standardized template was used for data collection. The template included the following independent variables: age, gender and sonographic features of the thyroid nodule (size, character, margins, and presence of calcifications and vascularity). Outcome variables were also gathered such as the cytologic diagnosis and subcategory of the biopsied nodule, management of the patient (whether repeat biopsy, surgery or follow-up was done); and the cytologic (for those who underwent repeat biopsy) or histopathologic (for those who underwent surgery) results. On final pathology, only the index nodule was considered as benign or malignant.
Descriptive statistics were used to analyze the demographic and clinical data of the patients. Description of qualitative data was done by the use of percentages. Quantitative data was described using mean and standard deviation.
Multiple logistic regression analysis was used to identify factors or variables predictive of malignancy. The odds ratio of each independent variable was estimated to determine the degree of relationship of the independent variable and malignancy. A p-value of < 0.05 means that the independent variable has a significant contribution in predicting malignancy.
Given that the odds that a nodule with an AUS or FLUS cytologic category will be benign is 11.96, and with an R2 of 0.38, a sample size of 68 has a calculated power of 94%.8
Among the 2247 patients who underwent fine-needle aspiration biopsy of the thyroid nodule at the St. Luke’s Medical Center from January 2012 to October 2013, a total of 200 (8.9%) had a cytologic diagnosis of atypia or follicular lesion of undetermined significance.
One hundred eighty-two (91%) are females while only 18 (9%) are males. The average age of the patients is 47.7 ± 14.31 years.
Of the 200 patients, 25 (12.5%) underwent repeat fine needle-aspiration biopsy, while a total of 68 (34%) underwent surgery. Fifty-two patients were reassessed with a clinical examination and an ultrasound (Figure 1).
Click here to download Figure 1
Figure 1. Management of Fine-Needle Aspiration Biopsy at St. Luke’s Medical Center form January 2012 to October 2013.

Table 3 shows that among those who underwent repeat fine-needle-aspiration biopsy (n=25), 10 (40%) had benign results, 12 (48%) were AUS or FLUS and 3 (12%) were consistent with malignancy (papillary carcinoma). Surgery was performed in 3 of the 25 patients, after a repeat biopsy.
Click here to download Table 3
Table 3. Result of Repeated Fine Needle Aspiration Following an Initial Result of AUS/AFUS

The average age of those patients who underwent surgery after an FNAB result of AUS or FLUS is 47.7 ± 13.6 years. Fifty-six (82.4%) of the subjects are female. Of which, 37 nodules are benign while 19 are malignant. In terms of sonographic characteristics, majority (64.4%) of the nodules are solid and the remainder are complex. The size of the nodules ranges from 0.6 cm to 6.8 cm. A third (33.9%) of the nodules biopsied are greater than 3 cm. Only 6.5% of the nodules are sub-centimeter in size. Half of the nodules are hyperechoic, 40% have mixed echogenicity while only 10% are hypoechoic. The majority (83.3%) of the nodules have well-defined margins. Seventy-nine percent of the nodules have no microcalcifications, while 65.9% of them are avascular (Table 4).
Under the cytologic subcategory of atypia, 55 % of the nodules fall under category 5, due to focal features suggestive of papillary carcinoma; while 44.8% of them are under category 1, due to prominent microfollicles.
Among the 68 patients who underwent surgery, forty-four (64.7%) had benign results on final histopathology. Most are females (84.1%) with an average age of 46 years old ± 12.8 years.
By sonology, most nodules were more than 3cm in size (41%), solid (57.9%), hyperechoic (48.5%), with well-defined margins (80.6%), with no micro calcifications (93.5%) or intra-lesional vascularity (70.4%). The majority of the nodules fall under the 5th subcategory of atypia (51.2%) (Table 4).
Click here to download Table 4
Table 4. Clinical Characteristics, Ultrasonographic Features of the Thyroid Nodule, and Cytologic Subcategory of Atypia of those Patients who Underwent Surgery
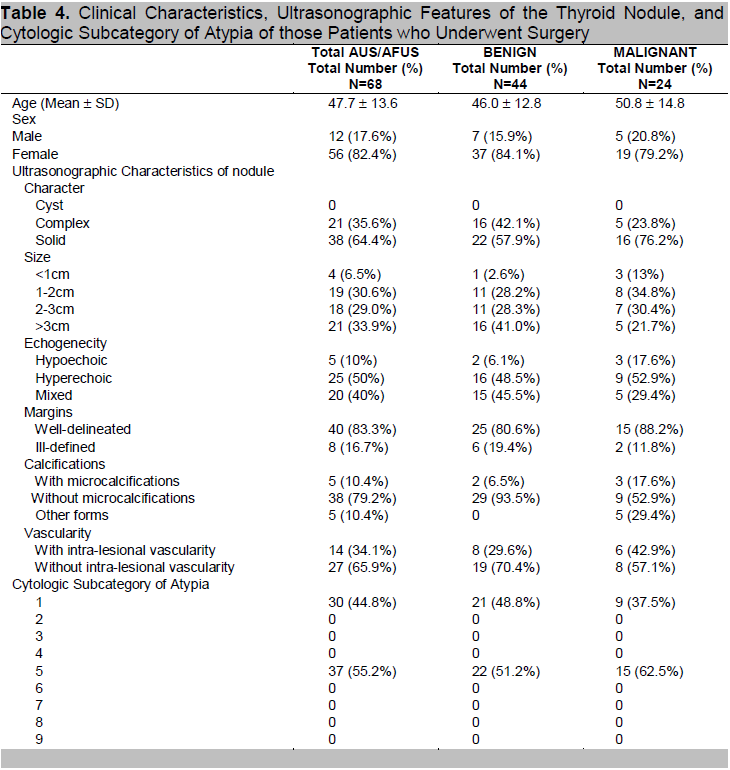
Among those who underwent surgery, twenty-four (35.3%) had malignant results on final histopathology. Nineteen (79.2%) are females with an average age of 50.8 years old ± 14.8 years.
The majority of the nodules are solid (76.2%) by sonology measuring 1-2cm in its widest diameter (34.8%), hyperechoic (52.9%), with well-defined margins (88.2%), without microcalcifications (52.9%) or intra-lesional vascularity (57.1%). Fifteen (62.5%) were categorized under the 5th category of atypia, while the remaining 9 (37.5%) fall under the 1st category (Table 4).
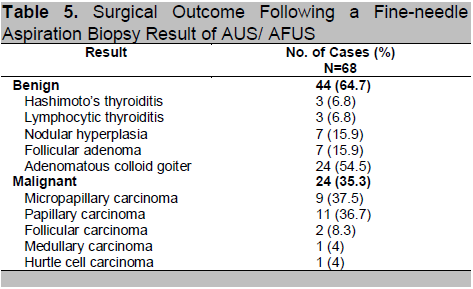
Table 5 shows the histopathology results of those who underwent surgery. Forty-four (64.7%) of the nodules were benign, with the majority classified as adenomatous colloid goiter (54.5%). The rest of the findings are as follows: Hashimoto’s thyroiditis (6.8%), lymphocytic thyroiditis (6.8%), nodular hyperplasia (15.9%) and follicular adenoma (15.9%). There were 24 cases of histologically documented malignancies: 9 (37.5%) micropapillary carcinomas (size < 1cm), 11 (36.7%) papillary carcinomas, 2 (8.3%) follicular carcinomas, 1 (4%) medullary carcinoma and 1 (4%) Hurtle cell carcinoma. The overall malignancy rate is 35.3%.
Click here to download Table 5
Table 5. Surgical Outcome Following a Fine-needle Aspiration Biopsy Result of AUS/ AFUS
As seen in Table 6, in the presence of other variables in the model, only size and vascularity were significant predictors of malignancy. The odds ratio for size is 0.19. This means that as the size increases (from < 1cm to 1-2 cm, or 1-2 cm to 2-3 cm, or 2-3 cm to more than 3cm), the odds that the nodule with an AUS or FLUS cytologic result is malignant decreases by 0.19 times. Smaller size is associated with malignancy.
On the other hand, the odds that an AUS or FLUS nodule with no intra-lesional vascularity will be classified as malignant is 19.1 times that of a nodule with intra-lesional vascularity. However, the corresponding confidence interval for the absence of intra-lesional vascularity is very wide, indicating that this result may not be conclusive.
Click here to download Table 6
Table 6. Multivariate Analysis for Malignancy

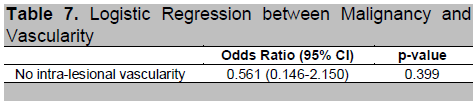
Logistic regression was done between malignancy and vascularity as seen in Table 7. Based on the p-value, the absence of intra-lesional vascularity is not statistically significant if it is the sole independent variable for malignancy. This is different from the multiple regression discussed earlier. Nevertheless, with an estimated odds ratio < 1, a thyroid nodule without intra-lesional vascularity is associated with benign histopathology. Vascularity, on the other hand, is associated with malignancy.
Click here to download Table 7
Table 7. Logistic Regression between Malignancy and Vascularity
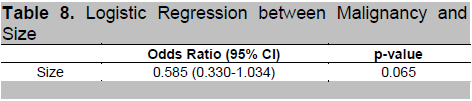
When size is the only independent variable regressed to malignancy, its p-value is > 0.05 suggesting that it is not statistically significant (Table 8). This also contradicts the results of multiple logistic regression. However, the direction of the association of size and malignancy is still the same (whether in the presence of other independent variables or not). There is a trend that bigger nodules are associated with benign histopathology, but it is not statistically significant.
Click here to download Table 8
Table 8. Logistic Regression between Malignancy and Size
Also, although not statistically significant, malignancy is more associated with males than with females. For ultrasonographic characteristics, a solid nodule is more associated with malignancy than a complex nodule. Nodules that are hypoechoic or with mixed echogenecity are more associated with malignancy than hyperechoic nodules. Those with well-defined margins are more correlated with benign histopathologic results. Moreover, the presence of microfollicles (subcategory 1) is more associated with malignancy than focal features of papillary carcinoma (subcategory 5). On the other hand, the odds ratio for age is near 1, which implies that age is not predictive of whether a nodule is benign or malignant.
This report presents the clinical data of 200 patients who underwent fine-needle aspiration biopsy of thyroid nodule with a cytologic diagnosis of atypia or follicular cells of undetermined significance at St. Luke’s Medical Center from January 2012 to October 2013. The institutional experience in the management of patients with FNABs reported as AUS or FLUS was described.
Although the Bethesda System advocates the creation of a category termed AUS or FLUS, it also recommends that this category be used sparingly, limiting its use to approximately 7% of all thyroid FNA interpretations. The recommended management for an initial AUS interpretation is clinical correlation and, for most cases, a repeat FNAB at an interval of about 3-6 months.5
In this study, the prevalence of AUS or FLUS is 8.9%. This is consistent with some reports, although data on the incidence of AUS or FLUS have been variable ranging from 3%-27% of aspirates. Rabaglia, et al. reported a 12% incidence of AUS or FLUS and postulated that its overuse may be a reflection of lack of confidence with the new diagnostic criteria in the early adoption period.9
A number of studies have described the management of AUS or FLUS nodules since the NCI recommendations were published. Chen et. al., reviewed the medical records of those who underwent FNAB10 and, of the 393 patients, 61 (16%) had AUS or FLUS. Only 56 had complete follow-up, of which 19 underwent surgery, 26 underwent repeat FNAB and 9 were observed by clinical follow-up without repeat FNAB. In a study by Nagarkatii, et. al., a total of 203 patients of the 5391 FNABs performed met the diagnostic criteria for AUS or FLUS, 62% were sent directly to surgery, 25% had a repeat FNAB, and 13% were observed. 11
Contrary to the suggested management of these patients, the majority of patients in this study were sent to surgery after an FNAB result of AUS or FLUS. One possible explanation for this preference for surgery maybe the unfamiliarity with NCI recommendations to repeat the FNAB. During the pre-Bethesda system, a cytologic diagnosis of indeterminate lesion warrants surgical excision. The new Bethesda category with terms “atypia” and “follicular lesion” may have been considered by the clinician as the “indeterminate lesion” of the more familiar pre-Bethesda category.
The malignancy rate in this study is 35.3%, comparable to the study done by Shi in New York, where they reported the risk of malignancy of 35%.7 But in Texas and Ohio, they reported a malignancy rate of 13 and 19% respectively.9,10 A study in South Korea reported a malignancy rate of 47%, while an academic institution in the US reported a malignancy rate of 48%.12, 15
These reported rates are higher than the implied risk of malignancy (5-15%) adopted by the Bethesda System. These rates were extrapolated from 3 referral centers who were using a similar 6-tiered classification system long before the new system was introduced. The reported malignancy rates from the centers range from 19%-24%.16,17
The higher risk of malignancy in this study may be biased by the fact that only those patients who underwent surgery were studied. The patients who underwent repeat FNAB, who followed-up clinically and those who were lost to follow-up were excluded. Surgery was only performed in patients considered to be at high risk for malignancy. Thus, the calculated malignancy rate provides only an estimation of the true rate of malignancy, because not all of the patients with AUS/FLUS nodules underwent thyroidectomy for definitive diagnosis.
It is well-established that certain ultrasound characteristics of thyroid nodules, such as large size, hypoechogenicity, ill-defined margins, intra-lesional vascularity and presence of micro calcifications, have been associated with malignancy.2 A study in South Korea showed that in thyroid nodules with indeterminate cytology, ill-defined margins, microcalcifications and taller-than wide shape were features showing correlation with malignancy.13
In contrast, this study shows that ultrasound features such as echogenecity, margins and the presence of microcalcifications did not appear to differ between benign and malignant nodules. Only size and vascularity seems to be the significant predictors of malignancy in the presence of other variables in the model. However, if they are the sole independent variable for malignancy, the absence of vascularity and nodule size are not statistically significant.
For nodules with the subcategory of atypia, the presence of microfollicles (category 1) is more associated with malignancy than features of papillary carcinoma (category 5). The difference, however, is not statistically significant. This differs from previous studies showing a higher risk of malignancy in nuclear or cytologic features of papillary carcinoma.14 It is important to acknowledge that this study was based on retrospective review of primary pathology reports, without performing a slide review. The sub-classification of atypia was done by a cytopathologist based on the reported microscopic description of the original cytopathologist, reflecting a “real-world” working experience with this diagnostic category. As such, the varying reporting practices of individual cytopathologists may have adversely affected the power of the study to detect the importance of various qualifiers in AUS or FLUS.
Essentially, there were no sonographic characteristics or cytologic features that would statistically associate a thyroid nodule with a cytologic diagnosis of AUS or FLUS with malignancy.
This report presents the clinical data of 200 patients who underwent fine-needle aspiration biopsy of thyroid nodule with a cytologic diagnosis of atypia or follicular cells of undetermined significance and comprises 8.9% of all FNABs done from January 2012 to October 2013.
One-third of patients with AUS or FLUS underwent surgery and only 12.5% underwent repeat FNAB as recommended by the new Bethesda system. Of the 68 patients who underwent surgery, 44 were benign and 24 were malignant with a malignancy rate of 35.3%. Statistically, there were no ultrasound characteristics or microscopic findings that are significantly associated with malignancy. The recommendation of the Bethesda System of doing a repeat FNAB in these patients should, therefore, be reconsidered.
Since most patients did not undergo surgery, some patients may have had thyroid malignancy but were not histologically diagnosed. Due to the relatively limited number of patients who underwent surgery and the limited time frame, the calculated malignancy rate provides only an estimation of the true rate of malignancy.
We recommend that those patients who opted for a more conservative management and those who underwent repeat FNAB be reevaluated to obtain a better estimate of the malignancy rate of thyroid nodules with a cytologic diagnosis of AUS or FLUS.
By comparing the data gathered by this study to those of the pre-Bethesda System period, the effect of the Bethesda System of classification in terms of management and histologic outcome can be determined.
1. Gharib H, Papini E, Paschke R, et al. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and European Thyroid Association medical guidelines for clinical practice for the diagnosis and management of thyroid nodules. Endocrine Practice. 2011;16 (Suppl 1):1-43.
2. Carlos-Raboca J, Jimeno C, Kho S, et al. The Philippine Society of Endocrinology and Metabolism PhilTidDes Working Group, The Philippine Thyroid Disease Study (PhilTiDes 1): Prevalence of thyroid disorders among adults in the Philippines. Journal of the ASEAN Federation of Endocrine Societies. 2012;27(2):27-33.
3. Melmed S, Polonsky K, Larsen P, Kronenberg H. Williams Textbook of Endocrinology 12th ed. Elsevier Saunders, Philadelphia, PA.; 2011:445.
4. Cooper D, Doherty G, Haugen B, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009; 19(11):1167-1214.
5. Cibas E, Ali S. The Bethesda system for reporting thyroid cytopathology. Am J Clin Pathol. 2009;132:658-665.
6. Teixeira G, Chikota H, et al. Incidence of malignancy in thyroid nodules determined to be follicular lesions of undetermined significance on fine-needle aspiration. World J Surg. 2012;36:69-74.
7. Shi Y, Ding X, Klein M, et al. Thyroid fine-needle aspiration with atypia of undetermined significance: A necessary or optional category? Cancer Cytopathology. 2009;299-304.
8. Bonzaninm M, Amadori P, et al. Subclassification of the “Grey Zone” of thyroid cytology, a retrospective descriptive study with clinical cytological and histological corrrelation. Journal of Thyroid Research. 2011:1-8.
9. Rabaglia J, Kabbani W, et al. Effect of the Bethesda system for reporting thyroid cytopathology on thyroidectomy rates and malignancy risk in cytologically indeterminate lesions. Surgery. 2010;148:1267-73.
10. Chen J, Pace C, et al. Yield of repeat fine-needle aspiration biopsy and rate of malignancy in patients with atypia or follicular lesion of undetermined significance: The impact of the Bethesda system for reporting thyroid cytopathology. Surgery. 2012;152:1037-44.
11. Nagarkatii S, Faquin W, Lubitz C, et al. Management of thyroid nodules with atypical cytology on fine-needle aspiration biopsy. Ann Surg Oncol. 2013;20:60-65.
12. Theoharis C, Schofield K, et al. The Bethesda thyroid fine-needle aspiration classification system: Year 1 at an academic institution. Thyroid. 2009;1(11):1215-1223.
13. Yoon J, Kwak J, Kim E, et at. How to approach thyroid nodules with indeterminate cytology. Ann Surg Oncol. 2010;17:2147-2155.
14. VanderLaan P, Marqusee E, Krane J. Usefulness of diagnostic qualifiers for thyroid fine-needle aspirations with atypia of undetermined signifiance. Am J Clin Pathol. 2011;136:572-577.
15. Kim D, Lee E, et.al. Role of sonographic diagnosis in managing Bethesda class III nodules. Am J Neuroradiol. 2011;32:2136-2141.
16. Yang J, Schnadig V, Logrono R, Wasserman P. Fine-needle aspiration of thyroid nodules: A study of 4703 patients with histologic and clinical correlations. Cancer Cythopathol. 2007;111:306-315.
17. Yassa L, Cibas E, Benson C, et.al. Long-term assessment of a multidisciplinary approach to thyroid nodule diagnostic evaluation. Cancer Cytopathol. 2007;111:508-516.
Articles and any other material published in the JAFES represent the work of the author(s) and should not be construed to reflect the opinions of the Editors or the Publisher.
Authors are required to accomplish, sign and submit scanned copies of the JAFES Declaration that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere.
Consent forms, as appropriate, have been secured for the publication of information about patients; otherwise, authors declared that all means have been exhausted for securing such consent.
The authors have signed disclosures that there are no financial or other relationships that might lead to a conflict of interest. All authors are required to submit Authorship Certifications that the manuscript has been read and approved by all authors, and that the requirements for authorship have been met by each author.