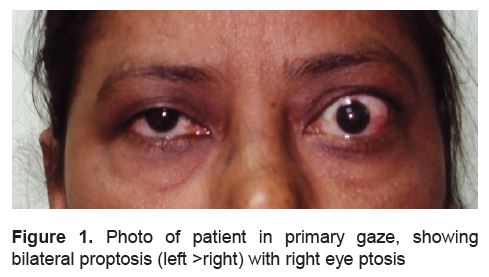
A 62-year-female presented with bilateral proptosis and 1 year episodic eye pain, grittiness, redness, watering and intermittent diplopia for 6 months, and drooping of right eye lid for 2 months (Figure 1). She had a firm WHO grade-1b goiter, exopthalmos (26 mm and 23 mm in left and right eye respectively, Hertel exopthalmometer), clinical activity score of 1/6, without any evidence of bulbar, neck muscles and limb weakness.
Click here to download Figure 1
Figure 1. Photo of patient in primary gaze, showing bilateral proptosis (left >right) with right eye ptosis
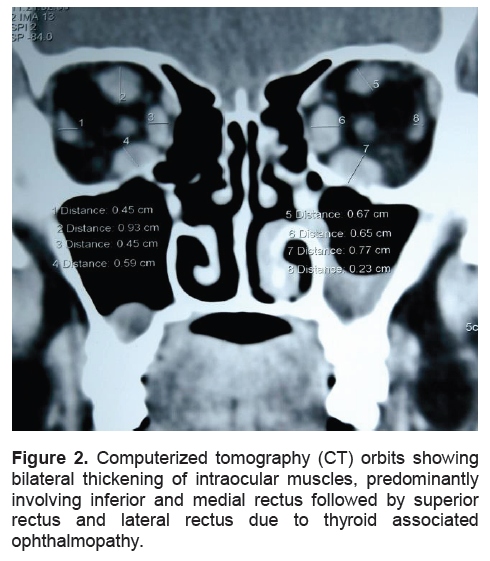
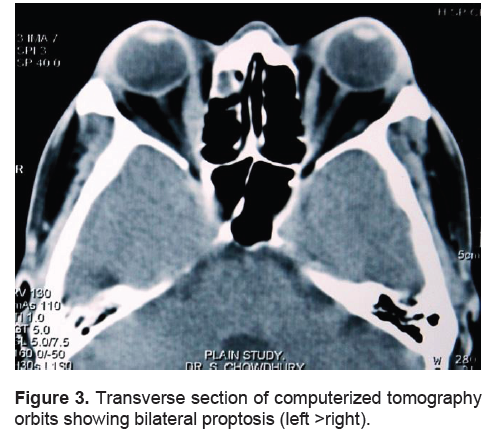
Computerized tomography (CT) of orbits revealed extraocular muscles thickening and expansion of retro-orbital fibro-fatty tissue confirming the diagnosis of thyroid associated ophthalmopathy (TAO) (Figures 2, 3). Investigations revealed low free T 4 (0.8 ng/dl; normal: 0.9-1.8 ng/dl), elevated TSH (38 µU/ml; normal: 0.4-4.2 µU/ml), elevated anti-thyroid peroxidase antibody (189 IU/ml; normal <35 IU/ml), anti-acetylcholine receptor antibody (2.32 nmol/L; normal <0.5 nmol/L); a repetitive nerve stimulation test of bilateral nasalis muscle was suggestive of ocular myasthenia with normal electrodiagnostic studies of limbs and normal CT thorax. Anti-TSH receptor antibody testing was not done, and is a limitation of this report. When she was last evaluated 3 months after diagnosis; ptosis had improved with pyridostigmine (60 mg 4 times daily) and levothyroxine (75 µg/d) initiated at dose of 1.25 µg/kg/day, which resulted in normalization of TSH (3.4 µU/ml).
Click here to download Figure 2
Figure 2. Computerized tomography (CT) orbits showing bilateral thickening of intraocular muscles, predominantly involving inferior and medial rectus followed by superior rectus and lateral rectus due to thyroid associated ophthalmopathy.
Click here to download Figure 3
Figure 3. Transverse section of computerized tomography orbits showing bilateral proptosis (left >right).
Primary hypothyroidism in TAO is rare, observed in only 5% cases, and is associated with milder and more asymmetrical ophthalmopathy.1 Hypothyroidism is extremely rare with myasthenia and is more associated with hyperthyroidism, occurring in 3-8% patients of patients.2 However, the occurrence of isolated ocular myasthenia with TAO is extremely uncommon with isolated reports in Graves’ disease, but never with primary hypothyroidism.3 Any patient with TAO and ptosis should be evaluated for ocular myasthenia. This case intends to highlight that TAO and ocular myasthenia can co-exist, even in primary hypothyroidism, is a diagnostic challenge with important consequences, as inability to achieve euthyroid status can worsen both TAO and myasthenia.
1. Eckstein AK, Lösch C, Glowacka D, Schott M, Mann K, Esser J, Morgenthaler NG. Euthyroid and primarily hypothyroid patients develop milder and significantly more asymmetrical Graves’ ophthalmopathy. Br J Ophthalmol.2009;93:1052-6.
2. Drachman D. Myasthenia gravis and other diseases of neuromuscular junction. In: Fauci A, Braunwald E, Kasper D, Hauser L. Harrison’s Principles of Internal Medicine. 17th Edition Volume-2, McGraw Hill. 2008; 2675.
3. Zouvelou V, Potagas C, Karandreas N, Rentzos M, Papadopoulou M, Zis VP, Vassilopoulos D. Concurrent presentation of ocular myasthenia and euthyroid Graves ophthalmopathy: A diagnostic challenge. J Clin Neurosci. 2008;15:719-20.
Articles and any other material published in the JAFES represent the work of the author(s) and should not be construed to reflect the opinions of the Editors or the Publisher.
Authors are required to accomplish, sign and submit scanned copies of the JAFES Declaration that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere.
Consent forms, as appropriate, have been secured for the publication of information about patients; otherwise, authors declared that all means have been exhausted for securing such consent.
The authors have signed disclosures that there are no financial or other relationships that might lead to a conflict of interest. All authors are required to submit Authorship Certifications that the manuscript has been read and approved by all authors, and that the requirements for authorship have been met by each author.