In the Philippines, approximately 7.2% of the population is diagnosed to have diabetes and its prevalence continues to increase as the prevalence of obesity escalates.1 Management of type 2 diabetes mellitus requires the adoption and maintenance of self-care behaviors, which include nutrition, aimed at achieving optimal metabolic outcomes and prevention of medical complications.2,3 Physicians often advise diabetic patients to adopt a healthy balanced diet and modify eating habits and patterns.4 However, diabetic patients find adherence to a healthy diet as most difficult component of self-care.5,6 Consequently, they fail to meet current treatment goals for glycemic control.7,8
The overall act of eating not only includes food intake per se, but also eating behavior in relation to preference, selection and consumption of food.4 Aside from behavior, it is also influenced by psychosocial and environmental factors.5-6,11 Savoca et al., in 2001 reported that eating patterns were influenced by participants' knowledge of diabetes management, dietary self-efficacy, social support and time management.5 A similar study from the same authors in 2004 identified food habits like limiting portions and high-sugar foods, meal planning, and carbohydrate/vegetable strategies were all related to lower HbA1c levels.7
In the Treatment Options for type 2 Diabetes in Adolescents and Youth (TODAY) study, young patients with type 2 diabetes who showed clinical (6%) and subclinical (20%) levels of binge eating were found to have higher rates of extreme obesity, global eating disorder, depressive symptoms and impaired quality of life.9 Moreover, a study by Mannucci et al., found that type 2 diabetes mellitus is unlikely to induce eating disturbances among obese patients.10 The study further supports the theory that external factors that influence eating behaviors play a significant role in the development of uncontrolled and emotional eating. Studies on eating behaviors among adults with type 2 diabetes are limited and no similar published studies were found in the Philippines.
The identification and understanding of eating behaviors and its relation to nutrition management could benefit both patients and physicians. Dietary restraint, loss of control over food intake and overeating during emotional distress have been identified as common eating behaviors, especially among obese subjects in foreign studies.12-15 Hence, several questionnaires such as the Restraint scale, Dutch eating behavior questionnaire, and Three-factor eating questionnaire have been developed and validated among obese and non-obese individuals.11,15-23
Research to better understand eating behaviors will help improve lifestyle education by identifying weaknesses in dietary practices. It may fill in the gap between knowledge on appropriate nutrition for patients with type 2 diabetes mellitus.4 The aim of every physician is to come up with nutrition education strategies that are individually tailored. To do this, we first need to be familiar with the general picture of eating behaviors in our local setting, hence, the goal of this study is to develop and validate a Filipino eating behavior questionnaire among adults with type 2 diabetes mellitus.
Based on the literature review, items from three eating behavior questionnaires (Three-factor eating behavior, Dutch eating behavior, and Restraint scale) were pooled to serve as reference for the construct of the new Filipino eating behavior questionnaire.
Upon approval of the University of the Philippines-Manila Research Ethics Board, focus group discussions and expert consultations were carried out to identify eating behaviors among Filipinos that have not been previously described in the available literature.
Participants were patients with type 2 diabetes from the University of the Philippines-Philippine General Hospital (UP-PGH) out-patient clinics who were recommended by their physicians and agreed to engage in the discussions. They were then divided into 5 groups, namely: group 1-male, above 40 years (n=6); group 2-female, above 40 years (n=6); group 3-male, 40 years and below (n=4); group 4-female, 40 years and below (n=7); and group 5-non-diabetic dieticians (n=3) from the UP-PGH dietary department who shared their encounters with type 2 diabetic patients during counselling sessions. The discussions included 24-hour food recalls, sharing of daily eating habits, and eating practices during special occasions and times of emotional distress. A voice recording was taken of every session to accurately document participants' responses, reactions, and even intonations.
Expert consultations were also done with an endocrinologist, nutritionist, psychiatrist and medical anthropologist. Most experts cited that Filipinos are fond of eating together as a family; that this sociocultural behavior results in loss of restraint or uncontrolled over eating; and diabetic patients are under social pressure to impress their hosts with abundance whenever food is offered.
After transcription, the participants responses were reviewed and categorized by the primary investigator and expert panel. Responses that were found to be similar to items from known eating behaviors were assigned to their respective domains. Initially uncategorized responses were reassessed and classified to form the eating behaviors newly identified among Filipinos with type 2 diabetes mellitus.
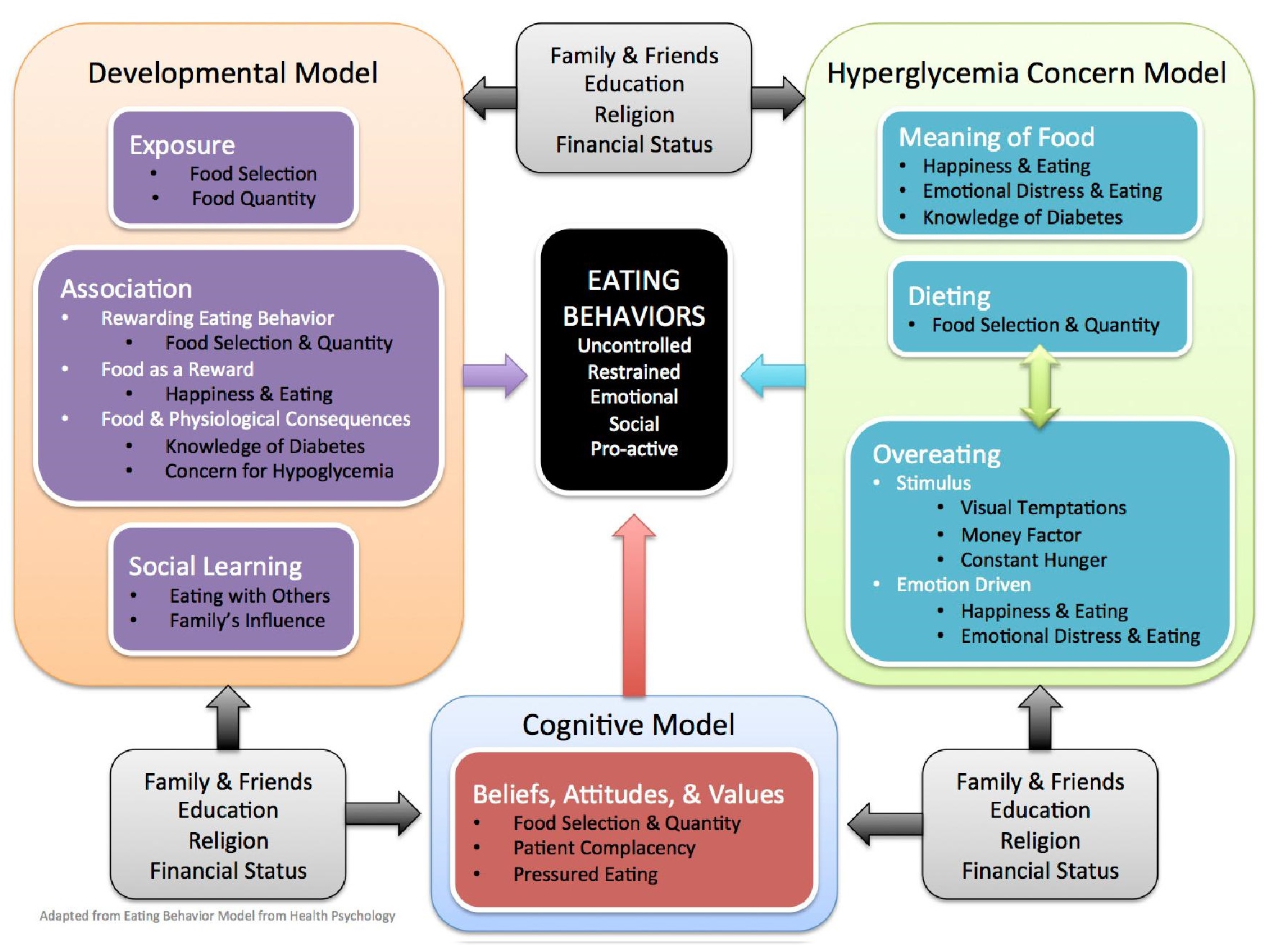
All participant responses were used to construct the conceptual framework and hybrid questionnaire, which was a combination of adapted items from established instruments plus the newly constructed items that were not covered by existing questionnaires.
Click here to download Figure 1Figure 1. The conceptual framework
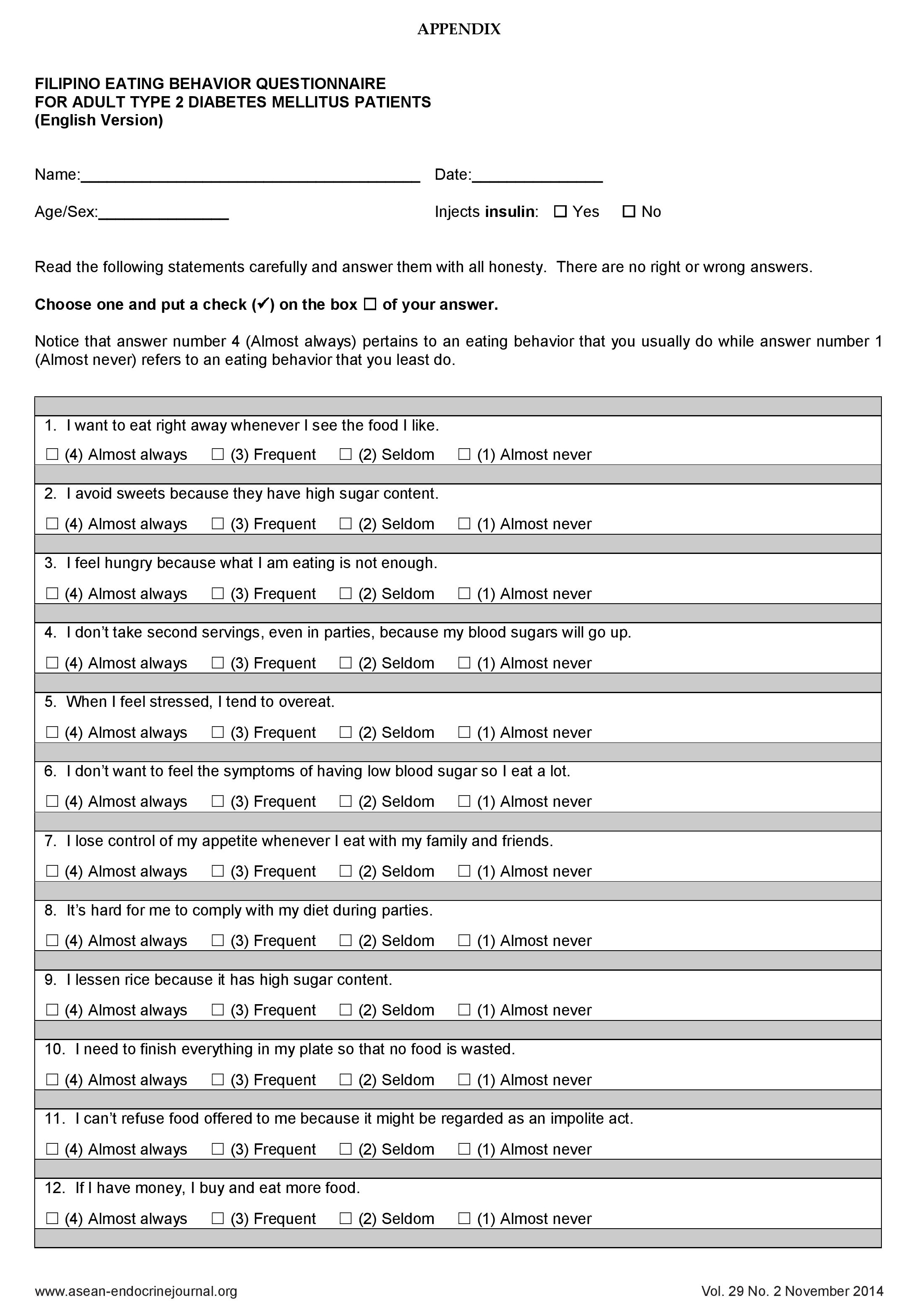
The items of the hybrid questionnaire were translated from English to Filipino by two bilingual translators whose first language is Filipino. The first translator was a medical professional involved in the study while the second translator was a non-medical professional who was unaware of the concepts of the questionnaire. These two forward translations were reviewed and synthesized into a hybrid Filipino version. The hybrid version was then translated back to English by two other bilingual translators who did not have medical backgrounds. Linguistic and cultural quality of the questionnaire were reviewed. The panel consolidated all items and reached a consensus to produce a 29-item Filipino version that was culturally appropriate and conceptually equivalent to the originally constructed questionnaire. The questionnaire was answerable by a 4-point Likert scale with the following responses: almost always, frequently, seldom, and almost never.
The pre-testing of the questionnaire was done among 20 type 2 diabetic patients at the UP-PGH out-patient clinics.
Majority of the respondents were elementary undergraduates.Twelve of them did not use insulin. The average time needed to finish answering the Filipino eating behavior questionnaire was 12 minutes. Words like "blood sugar" and "stress" were maintained and not translated to Filipino because these were commonly used by the respondents. An item to identify which respondents did not use insulin was added to guide the interpretation of the pro-active eating domain among insulin naive patients since most have not experienced hypoglycemia.
A total of 197 patients were recruited as questionnaire respondents. The study included patients who were 30-65 years of age; able to read, write and understand the Filipino language; diagnosed with type 2 diabetes based on the American Diabetes Association 2013 criteria; with disease duration of at least 6 months; and voluntarily joined the study after signing the informed consent form. All were referred by their physicians from the out-patient clinics of the UP-PGH through convenience sampling. Excluded from this study were patients diagnosed to have type 1 diabetes mellitus, women who were pregnant, and those on drugs which increase blood sugar levels such as steroids, anti-convulsants, atypical anti-psychotics, anti-fungals, sex hormones, anti-retrovirals, octreotide, lamivudine, and levothyroxine.
The internal consistency of the questionnaire was determined using Cronbach's α. A minimal correlation of 0.60 was set to claim that the instrument and its subscale scores were acceptable.31 Spearman's rank correlation was used to correlate pairs of scores from the same participants given the same questionnaire at least one week apart. All analyses were conducted using the statistical program package Stata 12.
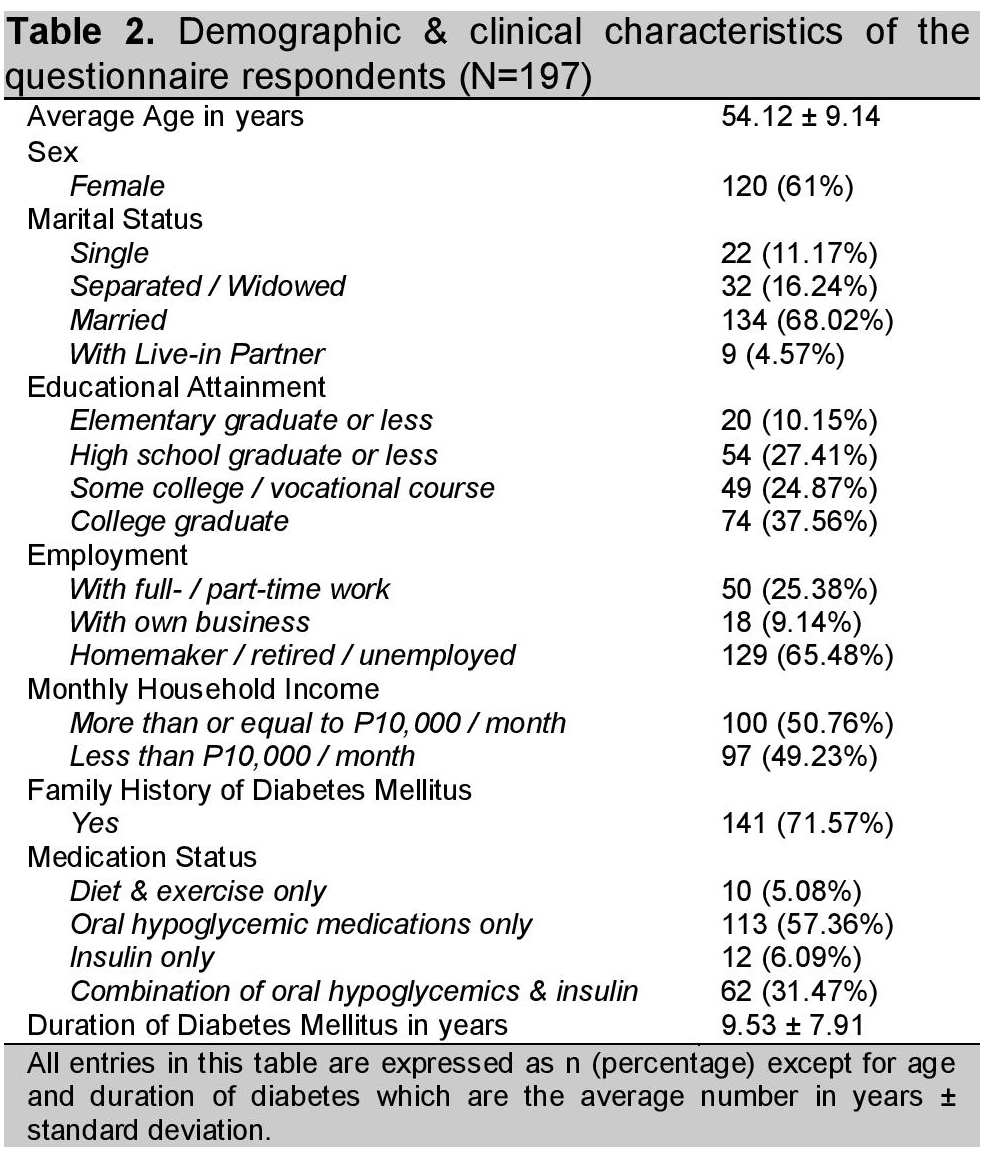
As shown in table 2, more than half of the respondents were females (61%), married (68.02%), able to attend or graduate from college (62.44%), and were either retired or unemployed (65.48%). The average age was 54.12±9.14 years with diabetes duration of 9.53±7.91 years. Around 37% were on insulin therapy.
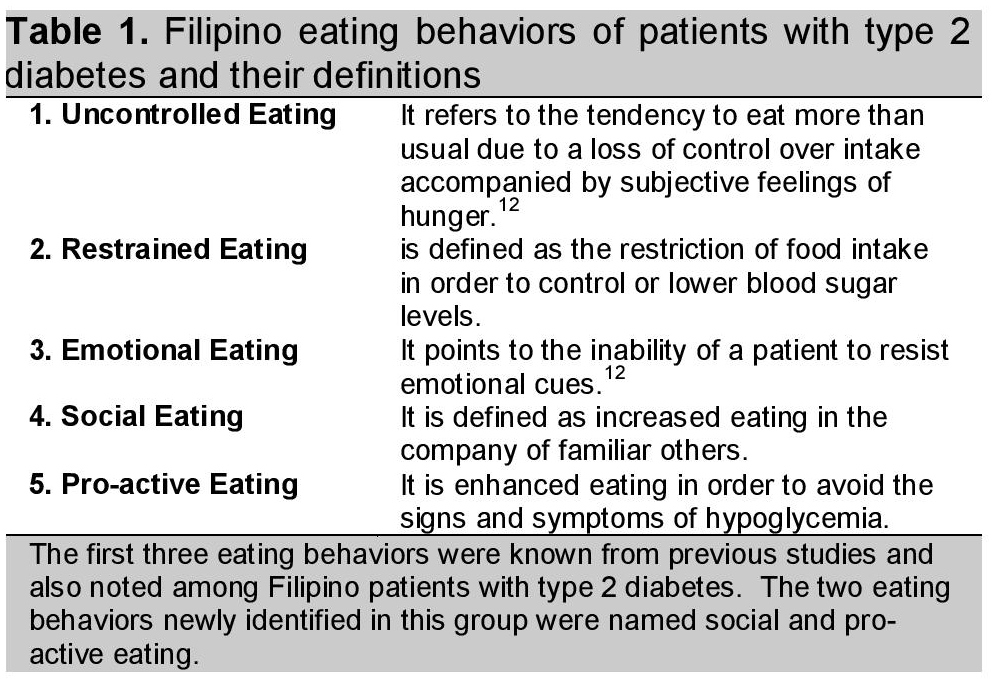
Click here to download Table 1Table 1. Filipino eating behaviors of patients with type 2 diabetes and their definitions
Click here to download Table 2
Table 2. Demographic & clinical characteristics of the questionnaire respondents (N=197)
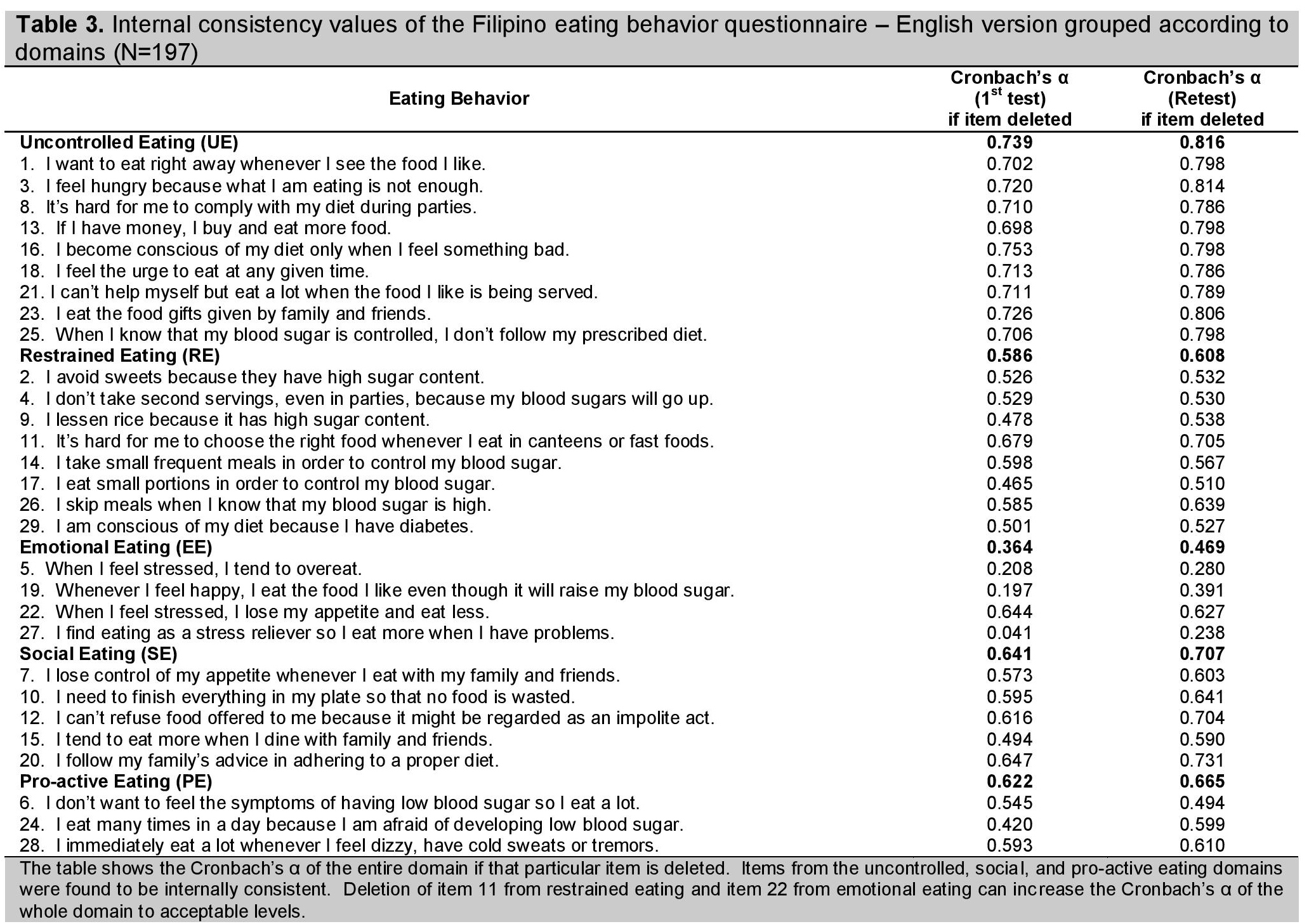
In both first and second testings, only the items in the uncontrolled (Cronbach's α 0.739 & 0.816), social (a 0.641 & 0.707), and pro-active (a 0.622 & 0.665), eating domains were found to be internally consistent.
For the restrained eating domain, deletion of item 11 (It's hard for me to choose the right food whenever I eat in canteens or fast foods) could be done to reach the minimum acceptable value of 0.60 and raise the Cronbach's α from 0.586 and 0.608 to 0.679 and 0.705 for the first and second testings, respectively. The lowered Cronbach's α in this domain might be explained by item 11's statement about being in a situation where difficult food choices are made as opposed to the other items which all describe actions to control blood sugar.
On the other hand, item 22 (When I feel stressed, I lose my appetite and eat less) of the emotional eating domain could be deleted to increase the internal consistency from 0.364 and 0.469 to 0.644 and 0.627 for the first and second testings, respectively. This item differed from the rest since it pertains to loss of appetite related to emotional distress unlike the other items which showed emotion-driven overeating. However, the expert panel decided to retain this item because it covers an aspect of emotional eating that leads to undereating.
Click here to download Table 3Table 3. Initial consistency values of the Filipino eating behavior questionnaire-English version grouped according to domains(N=197)
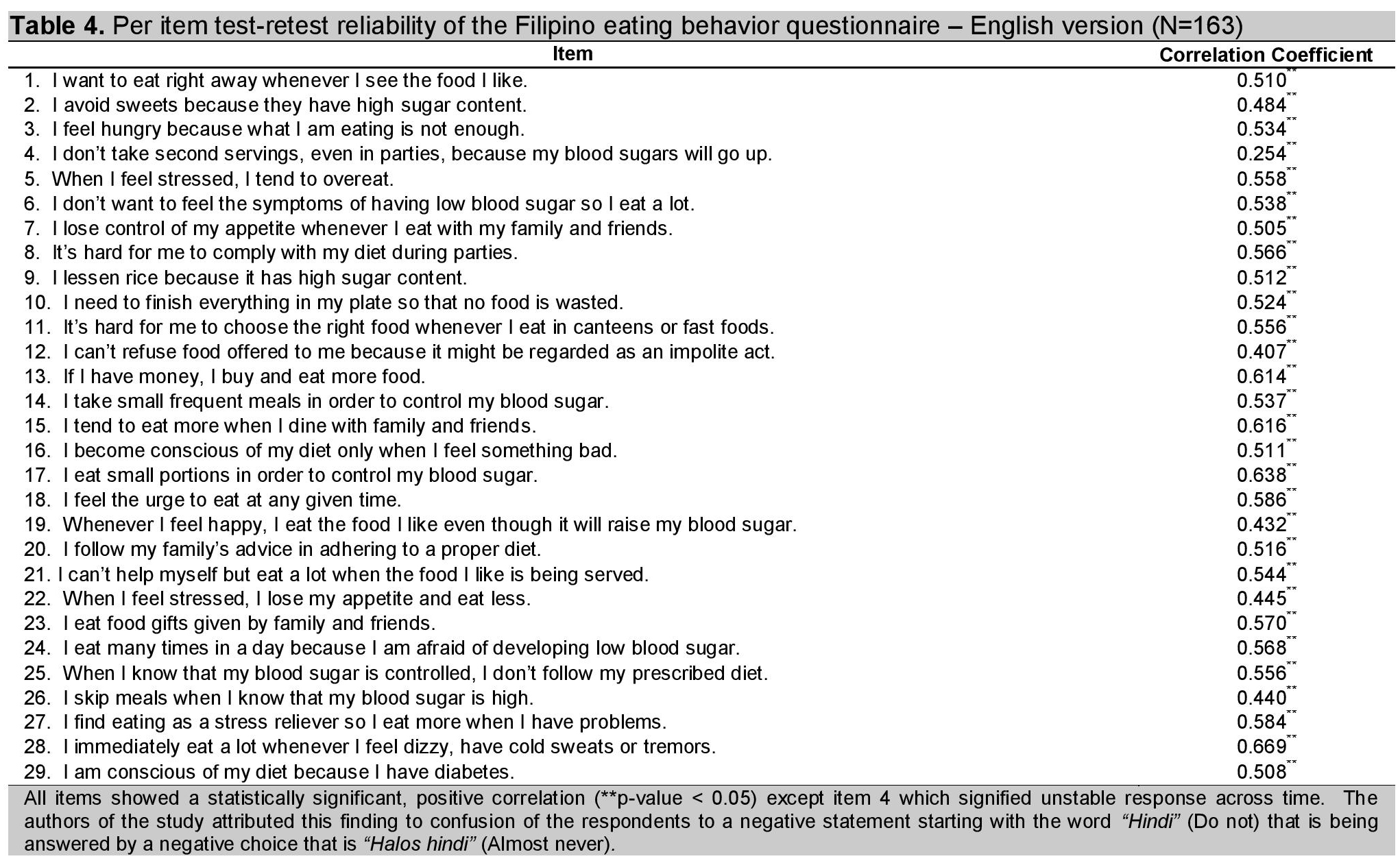
A total of 163 out of 197 respondents were able take the second testing. The mean test-retest interval was 9 days (SD= 4.36 days). As shown in table 4, statistically significant (p-value < 0.05) moderate, positive correlation, ranging from 0.407 to 0.669, indicated fairly stable responses in the two runs of the questionnaire. However, item 4 (I don't take second servings, even in parties, because my blood sugars will go up) demonstrated a relatively low correlation coefficient of 0.254.
Click here to download Table 4Table 4. Per item test-retest reliability of the Filipino eating behavior questionnaire-English version (N=163)
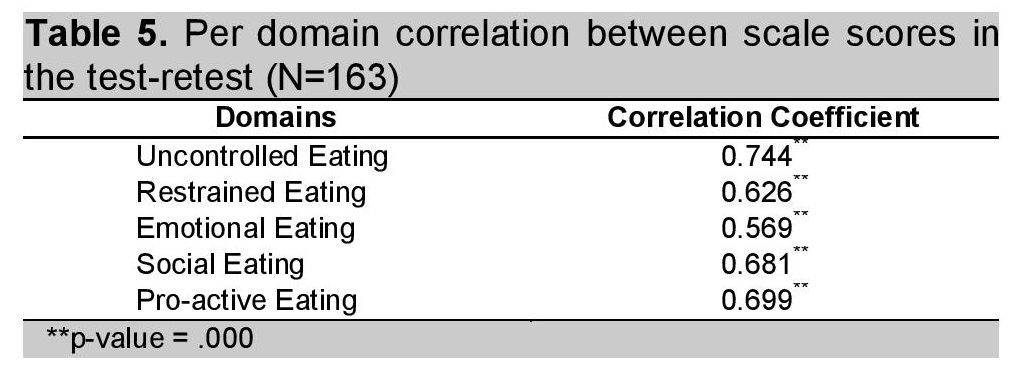
If the items were taken as a group by domains (Table 5), statistically significant (p-value < 0.05) moderate to high positive correlation, ranging from 0.569 to 0.744, between scale scores in the first and second runs were observed and indicated stable responses.
Click here to download Table 5Table 5. Per domain correlation between scale scores in the test-retest (N=163)
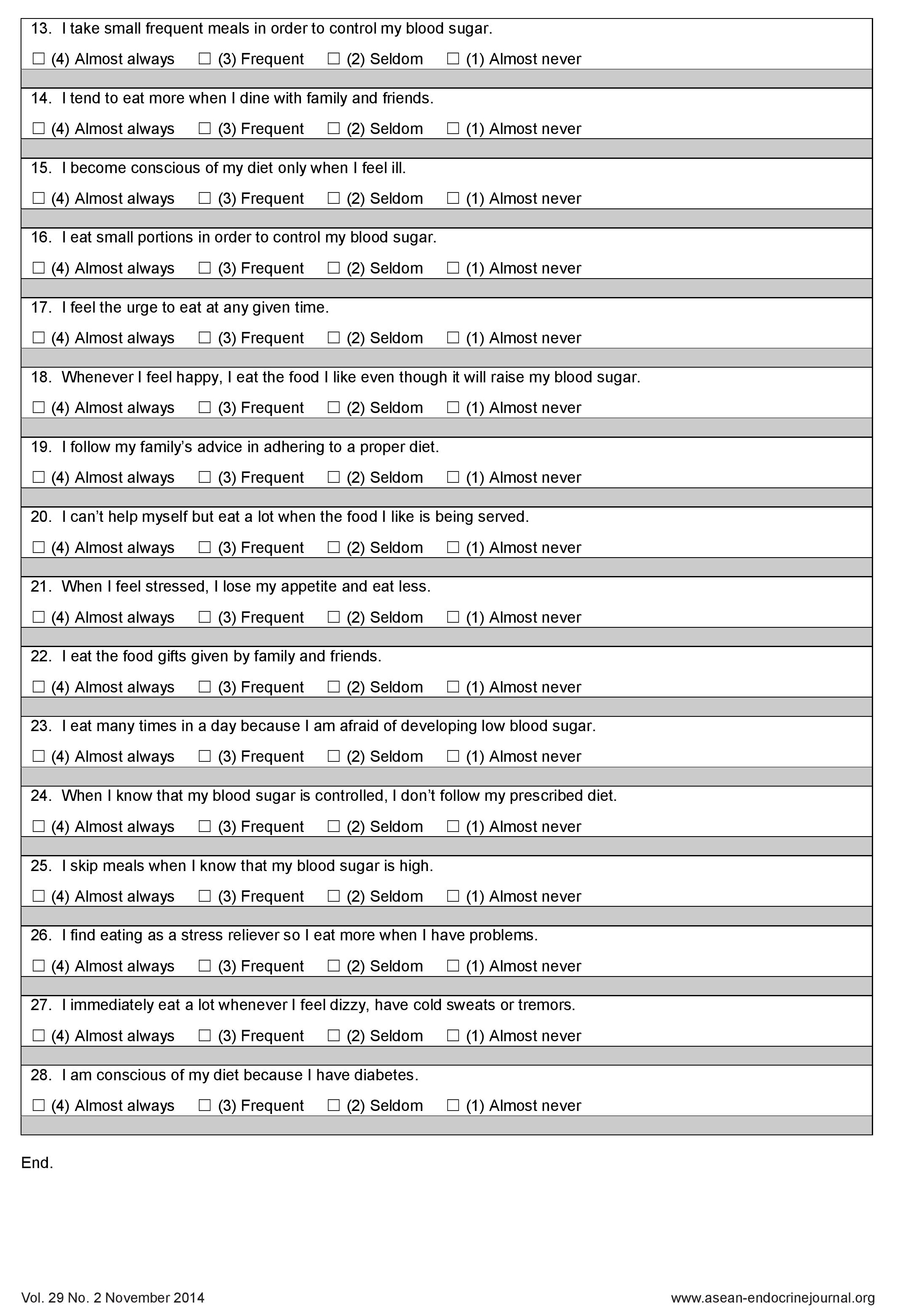
The final questionnaire is a 28-item, Filipino eating behavior questionnaire for adults with type 2 diabetes mellitus.
The questionnaire featured three known eating behavior domains which include uncontrolled, restrained and emotional eating plus two new domains that were named social and pro-active eating. The known eating behaviors were adapted from questionnaires for obese patients and these three behaviors were also observed in this population. This finding was somewhat expected since uncontrolled, restrained and emotional eating had been identified as common eating behaviors based on previous studies.8-11 Furthermore, type 2 diabetic patients are usually overweight or obese patients, hence, the probability of similar eating behaviors.
Uncontrolled eating was a frequent topic during the expert consultations and patient discussions. Different situations like the presence of tempting foods, having extra money and knowing one has a controlled blood sugar could lead to complacency and loss of control over eating. Studies report the prevalence of binge eating disorders among type 2 diabetics to range from 2.5 to 25.6%.27-30 They support binge eating as a cause of increase in body weight and ultimately, a risk for type 2 diabetes mellitus development.4 Moreover, both binge eating and obesity may independently contribute to diabetes onset.28
Restrained eating was likewise identified in this study. Findings of Manucci et al., showed higher scores on the restraint scale among diabetic patients compared to obese non-diabetic controls. The explanation is that the diagnosis of diabetes intensified the drive for weight loss resulting in a more controlled diet.27 Similarly, participants of the group discussions expressed knowledge of having diabetes was a big factor in shifting to healthier food selections and portions.
For the emotional eating domain, happiness and distress were mostly described by this group. The four items under this domain illustrated two possible links of emotions to eating. Negative emotions, as exemplified by items 5 (When I feel stressed, I tend to overeat) and 27 (I find eating as a stress reliever so I eat more when I have problems), promote eating in order to regulate emotions.37 Some individuals use eating as a coping mechanism to alleviate negative moods and mask their stress.39-40 In addition, the processing of emotions requires attention and can lead to the loss of focus on the control of eating.37 Emotions can modulate eating in congruence with emotional features as well.37 Sadness or emotional distress was observed to decrease and happiness to increase food pleasantness and motivation to eat more.41 Based on discussions, patients associated happiness to celebrations and achievements that lead to the tendency to overeat and give in to prohibited foods, while some revealed that stress makes them lose their appetite. These behaviors were reflected in items 19 (Whenever I feel happy, I eat the food I like even though it will raise my blood sugar) and 22 (When I feel stressed, I lose my appetite and eat less).
The newly identified eating behavior termed "social eating" was defined as increased eating in the company of familiar persons. It was a prominent idea during the interviews and group discussions since Filipinos recognize the importance of eating as a social function. Accordingly, eating with family and friends can be enhanced by around 40-50% compared to eating alone.32-33 This is possibly explained by time extension, which states that when meals are eaten with others, meals tend to take longer, thereby increasing exposure to food cues and the opportunity to eat.34 Another explanation for this behavior considers eating with others as a distraction that diverts attention away from finishing the meal and this causes the individual to eat more.35-36 Also, Filipinos with diabetes value the advice of loved ones about dieting (item 20) and the need to show courtesy to those who provided the food (items 10 and 12).
The other newly identified eating behavior is "pro-active eating." The three items (item 6, 24, and 28) under this domain refer to increased eating by patients with type 2 diabetes in order to avoid the signs and symptoms of hypoglycemia. The concern about hypoglycemia, particularly by insulin users, was identified as a possible factor that pushes patients to overeat because they fear experiencing hypoglycemia. Unlike uncontrolled eating, this behavior is distinguished by the presence of a motivation from a perceived danger. Studies show that hypoglycemia provokes loss of personal control, embarrassment and anxiety to the patient and the family members as well.37
Nutrition education is a key approach for effective diabetes management.5 The recognition of these eating behaviors, through the use of the Filipino eating behavior questionnaire, may assist in creating a focused and structured nutritional management plan. Uncontrolled eaters may benefit from behavioral approaches for food stimulus control and even appetite-suppression therapy; restrained eaters may be more receptive to complicated strategies such as calorie counting; emotional eaters may need support groups to address personal issues; social eaters may be offered ways on how to be more attentive to food intake when eating with others; and lastly, pro-active eaters may require a strictly scheduled diet to avoid hypoglycemia.
The study showed that a culturally appropriate eating behavior questionnaire for type 2 diabetic patients is a generally reliable, reproducible and valid instrument to assess eating behaviors. Aside from the known eating behaviors such as uncontrolled, restrained, and emotional eating, social and pro-active eating are newly described behaviors seen in this group of Filipinos with type 2 diabetes. The application of this questionnaire can potentially assist physicians and nutritionists in coming up with individualized nutrition plans. It might possibly be used in countries with a similar cultural milieu as the Philippines, where social eating is prevalent but at the same time there is great fear of hypoglycemia, hence, pro-active eating is likewise observed.
My heartfelt gratitude goes to Dr. Mary Ann Ladia from the Department of Clinical Epidemiology, University of the Philippines-Manila; Dr. Belle Erika Nubla-Gestuvo & Dr. Louie Rebuccal from the UP-PGH Department of Psychiatry; Ms. Elizabeth Limos from the UP-PGH Dietary department; Mr. Sumsabalip Alatiit, Ms. Renee Rose Cantos & Mr. Leonard David Espiritu for the translations. Thank you also to the Philippine Society of Endocrinology, Diabetes & Metabolism who provided funding for this research.
1. Sy RG, Morales DD, Dans AL, et al. Prevalence of atherosclerosis-related risk factors and diseases in the Philippines. J Epidemiol. 2012; 22(5): 440-447. http://dx.doi.org/10.2188/jea.JE20110095.
2. Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Eng J Med. 1993; 329: 977-1036. http://dx.doi.org/10.1056/NEJM199309303291401.
3. UK Prospective Diabetes Study Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (33). Lancet 1998; 352: 837-53. http://dx.doi.org/10.1016/S0140-6736(98)07019-6.
4. Yannakoulia M. Eating behavior among type 2 diabetic patients: A poorly recognized aspect in a poorly controlled disease. Rev Diabetic Stud. 2006; 3: 11-16. http://dx.doi.org/10.1900/RDS.2006.3.11.
5. Savoca M, Miller C. Food selection and eating patterns: Themes found among people with type 2 diabetes mellitus. J Nutri Educ. 2001; 33: 224-233. http://dx.doi.org/10.1016/S1499-4046(06)60035-3.
6. Sullivan ED, Joseph DH. Struggling with behavior changes: A special case for clients with diabetes. Diabetes Educ 1998; 24: 72-77. http://dx.doi.org/10.1177/014572179802400110.
7. Savoca M, Miller C, Ludwig D. Food habits are related to glycemic control among people with type 2 diabetes mellitus. J Am Diet Assoc. 2004; 104: 560-566. http://dx.doi.org/10.1016/j.jada.2004.01.013.
8. Harris MI. Racial and ethnic differences in health care access and health outcomes of adults with type 2 diabetes. Diabetes Care. 2001; 24: 454-459. http://dx.doi.org/10.2337/diacare.24.3.454.
9. Treatment options for type 2 diabetes in adolescents and youth (today) study group. A clinical trial to maintain glycemic control in youth with type 2 diabetes. N Engl J Med. 2012; 366: 2247-2256.
10. Nestle M, Wing R, Birch, et al. Behavioral and social influences on food choice. Nutr Rev. 1998; 56: S50-74.
11. De Lauzon B, Romon M, Deschamps V, et al. The three-factor eating questionnaire-R18 is able to distinguish among different eating patterns in a general population. J Nutri. 2004; 2372-2380.
12. Tuschl RJ. From dietary restraint to binge eating: Some theoretical considerations. Appetite. 1990; 14: 105-109. http://dx.doi.org/10.1016/0195-6663(90)90004-R.
13. Blundell JE & Gillett A. Control of food intake in the obese. Obese Res. 2001; 9 (Suppl. 4): 263S-270S.
14. Allison DB & Heshka S. Emotion and eating in obesity? A critical analysis. Int J Eat Disord. 1993; 13: 289-295. http://dx.doi.org/ 10.1002/1098-108X(199304)13:3<289::AID-EAT2260130307>3.0.CO;2-X.
15. Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985; 29: 71-83. http://dx.doi.org/10.1016/0022-3999(85)90010-8.
16. Karlsson J, Perssom L-O, Sjostrom L, et al. Psychometric properties and factor structure of the three-factor eating questionnaire (TFEQ) in obese men and women. results from the swedish obese subjects (SOS) study. Int J Obes. 2000; 24:1715-1725. http://dx.doi.org/10.1038/sj.ijo.0801442.
17. Angle S, Engblom J, Eriksson T, et al. Three factor eating questionnaire-R18 as a measure of cognitive restraint, uncontrolled eating and emotional eating in a sample of young finnish females. Int J Behavi Nutri & Phys Act. 2009; 6:41 (1-7).
18. Cappelleri JC, Bushmakin AG, Gerber RA, et.al. Psychometric analysis of the three-factor eating questionnaire-R21: results from a large diverse sample of obese and non-obese participants. Int J Obes. 2009; 33:611-620. http://dx.doi.org/10.1038/ijo.2009.74.
19. Heatherton TF, Herman CP, Polivy J, et.al. The (mis)measurement of restraint: An analysis of conceptual and psychometric issues. J Abnorm Psychol. 1988; 97:19-28. http://dx.doi.org/10.1037/0021-843X.97.1.19.
20. Williamson DA, Martin CK, York-Crowe E, et al. Measurement of dietary restraint: Validity tests of four questionnaires. Appetite. 2007; 48:183-192. http://dx.doi.org/10.1016/j.appet.2006.08.066.
21. Allison DB, Gorman BS, Kalinsky LB. A comparison of the psychometric properties of three measures of dietary restraint. Psychol Asses. 1992; 4:391-398. http://dx.doi.org/10.1037/1040-3590.4.3.391.
22. Laessle RG, Tuschl RJ, Kotthaus BC, Pirke KM. A comparison of the validity of three scales for the assessment of dietary restraint. J Abnorm Psychol. 1989; 4:504-507. http://dx.doi.org/10.1037/0021-843X.98.4.504.
23. Chearskul S, Pummoung S, Vongsaiyat S, et.al. Thai version of three-factor eating questionnaire. Appetite. 2010; 54:410-413. http://dx.doi.org/10.1016/j.appet.2010.01.005.
24. Oltersdorf U, Schlettweing-Gsell D, Winkler G. Assessing eating patterns-an emerging research topic in nutritional sciences: Introduction to the symposium. Appetite. 1999; 32:1-7. http://dx.doi.org/10.1006/appe.1998.0189.
25. Ogden J. "Eating behaviour." Health Psychology, 5th ed. McGraw-Hill, 2012. 133-165.
26. Manucci E, Tesi F, Ricca F, et al. Eating behavior in obese patients with and without type 2 diabetes mellitus. Int J Obes Relat Metab Disord. 2002. 26(6):848-853.
27. Kenardy J, Mensch M, Bowen K, et al. Disordered eating behaviors in women with type 2 diabetes mellitus. Eat Behav. 2001. 2(2):183-192.
28. Herpetz S, Albus C, Wagener R, et al. Comorbidity of diabetes and eating disorders. Does diabetes control reflect disturbed eating behavior? Diabetes Care. 1998. 21(7):1110-1116.
29. Crow S, Kendall D, Praus B, Thuras P. Binge eating and other psychopathology in patients with type II diabetes mellitus. Int J Eat Disord. 2001. 30(2):222-226.
30. Abhaya, I. "Quality considerations." Medical Biostatistics, 2nd ed. Chapman & Hall / CRC Biostatistics Series, 2008. 545-571.
31. De Castro JM. Family & friends produce greater facilitation of food intake than other companions. Physiol Behav. 1994; 56:445-55. http://dx.doi.org/10.1016/0031-9384(94)90286-0.
32. Shide DJ, Rolls BJ. Social facilitation of caloric intake in humans by friends but not strangers. Int J Obes. 1991; 15:8.
33. De Castro JM. Social facilitation of duration & size but not rate of the spontaneous meal intake of humans. Physiol Behav. 1990; 47:1129-35. http://dx.doi.org/10.1016/0031-9384(90)90363-9.
34. Bellisle F, Dalix AM. Cognitive restraint can be offset by distraction, leading to increased meal intake in women. Am J Clin Nutr. 2001; 74:197-200.
35. Mitchell GI, Brunstrom JM. Everyday dietary behavior & the relationship between attention & meal size. Appetite. 2005; 45:344-45. http://dx.doi.org/10.1016/j.appet.2005.06.001.
36. Frier BM. How hypoglycemia can affect the life of a person with diabetes. Diabetes Metab Res Rev. 2008; 24:87-92. http://dx.doi.org/10.1002/dmrr.796.
37. Macht M. How emotions affect eating: A five-way model. Appetite. 2007; 50:1-11. http://dx.doi.org/10.1016/j.appet.2007.07.002.
38.Marx RG, Menezes A, Horovitz L, et al. A comparison of two time intervals for test-retest reliability of health status instruments. J Clin Epidemiol. 2003; 56:730-735. http://dx.doi.org/10.1016/S0895-4356(03)00084-2.
39. Thayer RE. Calm Energy-How people regulate mood with food and exercise. Oxford: Oxford University Press.
40. Polivy J & Herman, CP. Distress and eating: Why dieters overeat? Int J of Eat Disord. 1999; 26: 153-164.
41. Macht M, Roth S, & Ellgring H. Chocolate eating in healthy men during experimentally induced sadness and joy. Appetite. 2002; 39:147-158. http://dx.doi.org/10.1006/appe.2002.0499.
Click here to download Appendix page 1Appendix page 1. FILIPINO EATING BEHAVIOR QUESTIONNAIRE FOR ADULT TYPE 2 DIABETES MELLITUS PATIENTS
Click here to download Appendix page 2
Appendix page 2. FILIPINO EATING BEHAVIOR QUESTIONNAIRE FOR ADULT TYPE 2 DIABETES MELLITUS PATIENTS
Authors are required to accomplish, sign and submit scanned copies of the JAFES Declaration that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere.
Consent forms, as appropriate, have been secured for the publication of information about patients; otherwise, authors declared that all means have been exhausted for securing such consent.
The authors have signed disclosures that there are no financial or other relationships that might lead to a conflict of interest. All authors are required to submit Authorship Certifications that the manuscript has been read and approved by all authors, and that the requirements for authorship have been met by each author.