Hyperglycemia has been known to be a poor marker of outcome in hospitalized patient, for both diabetic and non diabetic patients, particularly critically ill patients.1,2 Newly diagnosed diabetes was associated with longer hospital stay and higher admission rates to intensive care units.1 The increased morbidity and mortality due to hyperglycemia provides strong rationale for intensive control of blood glucose levels in hospitalized patients. An intensive approach using insulin for patients in acute care and surgical settings is considered the most effective regimen for controlling hyperglycemia in the hospital setting.1 Evidence-based rationale for early and aggressive intervention with insulin for glycemic control in the hospital setting as exemplified by Van den Bergh showed significant and huge reductions in mortality, sepsis, incidence of dialysis, use of blood transfusions, and polyneuropathy.5 This target shifted to less strict control at 140-180 mg/dl as the weight of the evidence seen in NICE-SUGAR (Normoglycemia in Intensive Care Evaluation and Survival Using Glucose Algorithm Regulation) data has shown that, intensive insulin therapy increased the risk of hypoglycemia and provided no overall benefit on mortality in the critically ill.6 These results have led to a heightened interest in improving the quality and safety of the management of diabetes and hyperglycemia in the hospital.
The use of intravenous continuous insulin infusion is the preferred route of insulin administration for the management of hyperglycemia in the critical care setting.
Standardization of insulin therapy improves the efficiency and safety of glycemic control in critically ill adults. Several authors have focused on the implementation of a treatment protocol using intravenous insulin infusion over subcutaneous insulin injection in the management of hyperglycemia.3-5,7 Intravenous insulin infusion has shown to reduce the frequency of sternal infections among postoperative coronary bypass graft surgery.3 There was overall reduction in mortality of 29% in patients acute myocardial infarction treated with intravenous insulin for 24 hours,
The importance of using a standard protocol cannot be overemphasized. This will reduce confusion and errors and result in a safer environment for the critically ill patient. Published studies2,10 evaluating the implementation of a standard protocol demonstrated improved glycemic control and less hypoglycemia.11 Implementation of such a protocol in the ICU does not only decrease the variability of care but also improve outcomes.12 According to the review of Wilson on 12 insulin protocols, a systematic comparison of the performance of protocols was not possible due to the lack of prospective, randomized trials.13 His review showed that there was no head-to-head comparison between protocols, thus superiority of one protocol over the other cannot be deduced. The difference he noted was the variability in insulin delivery and the complexity of instructions. Wilson also noted that the majority of protocols are nursing implemented with limited physician oversight. Physicians assist the nursing staff with titration in the Van den Berghe protocol.13
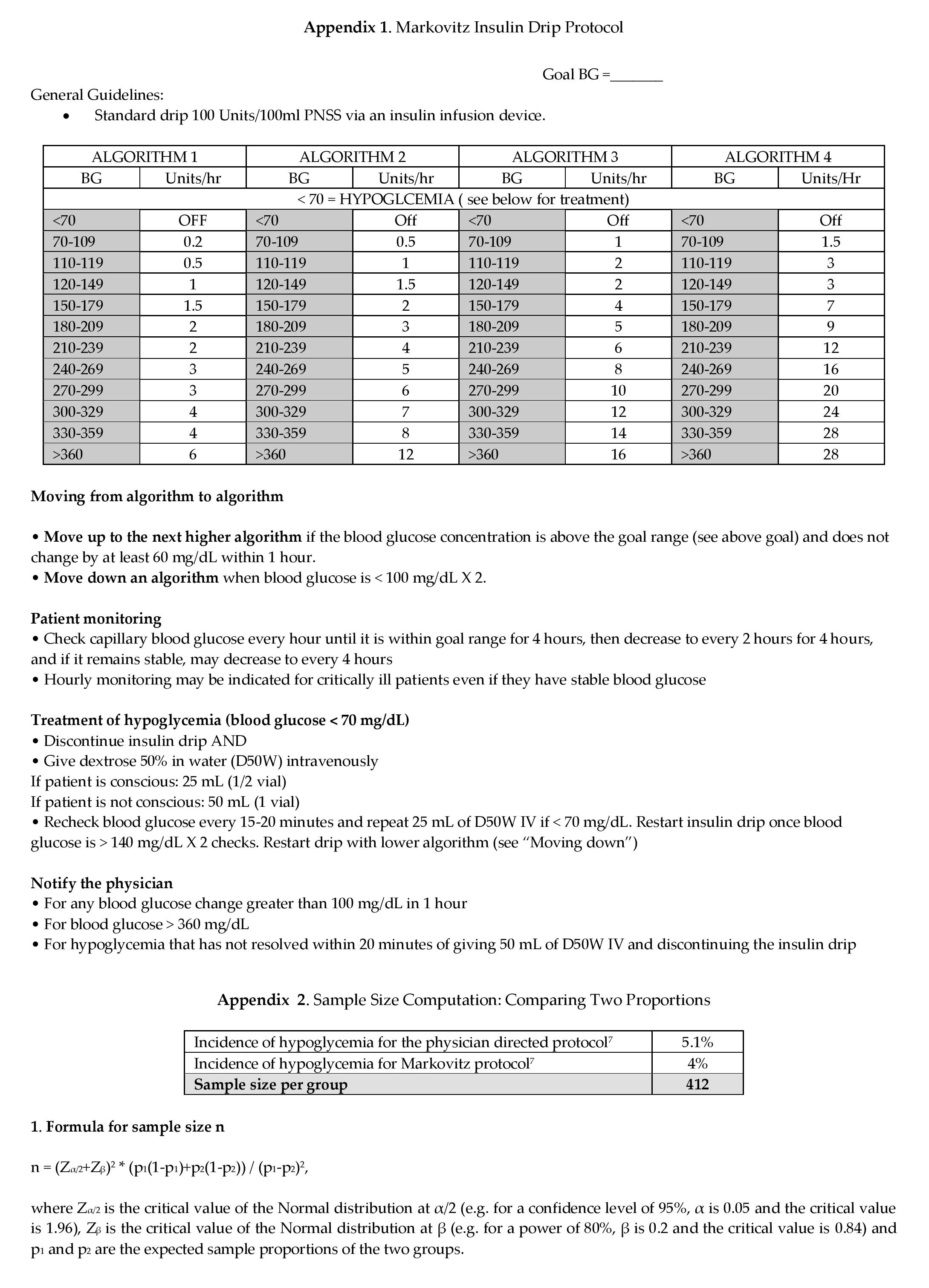
An ideal insulin infusion protocol is based not only on the current blood glucose level, but also on the rate of change in blood glucose and insulin sensitivity.9 In our institution, control of hyperglycemia was managed by giving insulin using subcutaneous route or using continuous insulin infusion drip titrated according to the discretion of the attending physician. Hourly rate of insulin titration change was directed by the specific orders of the doctors and were carried out daily by the nursing staff and medical residents on duty. In 2005, MIP was adapted to assist non-endocrinologists to manage hyperglycemic episodes in emergency situation where immediate referral cannot be made. The Markovitz Insulin7 protocol was designed by Dr.Lawrence Markovitz, a thoraco-vascular surgeon in consultation with staff endocrinologist and was used in the management of postoperative cardiac patients in a community hospital. This protocol was formulated for post CABG patients and includes parameters for initiating the insulin infusion, blood glucose monitoring and changing the insulin infusion rates. The protocol was published in 2002 with blood glucose goals of 120-199 mg/dL. There were protocols which represents modifications of the Markovitz protocol published by Bode and Ku. It was also adapted by the University of Washington14 as an institutionalized insulin protocol and utilized in all patient populations including diabetes and corticosteroid or stress induced hyperglycemia. The protocol includes changing the insulin infusion rates for a glycemic goal of 80-180 mg/dL. This protocol was also chosen not only because it is easy to follow but its safety and efficacy has been validated.14
From 2007 onwards, the physician directed insulin protocol has been completely replaced by the MIP in the majority of patients admitted in the intensive care unit. This is the oldest published protocol of column method for insulin titration. In our institution, its application was not limited to coronary bypass graft surgery but included the management of diabetic ketoacidosis and critically ill diabetic patients both medical and surgical. Thus led to the review of its efficacy and safety in comparison with the non-protocol physician titration insulin infusion being used in our critical unit.
To compare the efficacy and safety of the Markovitz insulin protocol (MIP) with physician directed insulin titration infusion (PDI) in achieving normoglycemia in the treatment of critically ill diabetic patients admitted in the intensive care unit from 2001-2009.
To compare the rate of change to normal glucose levels between MIP and PDI.
To compare the time to achieve normal glucose levels between MIP to that of PDI.
To compare the number of hypoglycemic episodes between MIP and PDI.
This a cross sectional study examining medical records of critically ill patients admitted in the intensive care unit from 2001-2009. We accessed this information from the Medical information documentation access system (MIDAS). ICD-10 codes were used as keywords to screen for diabetic patients who were hyperglycemic with or without diabetic ketoacidosis (E.11.0 and E.14.0). All records of patients admitted in the ICU from 2001 to 2009 who were on continuous insulin infusion were collected. A total of 108 charts reviewed, 34 charts were managed using PDI were retrieved. No patients were identified using PDI from 2007 to 2009. While 72 patients were started on MIP from 2005 to 2009. The only period where two insulin infusion protocols existed was from 2005 to 2006. From 2007 onwards, the MIP remained the sole insulin infusion protocol used in the intensive care unit. Inclusion criteria included patients with completed insulin infusion from the time of initiation until the time the insulin infusion was discontinued. Excluded were patients who signed waiver for DNR status, and for transfer to hospital of choice.
This study was conducted in a tertiary hospital in two hospital location. The old site was located in Mandaluyong City and has 300 bed capacity with 14 intensive care unit bed, mixed medical/surgical cases. The hospital transferred to its new site in Pasig City, Philippines in 2004. It has a 500 bed capacity with 18 ICU beds. Common causes of ICU admissions in the old site were acute respiratory failure, primary cardiac event, septic shock, severe pneumonia, acute renal failure, diabetic ketoacidosis, massive GI bleeding, cerebrovascular accident and coronary artery bypass graft patients. Management of ICU patients was limited to 1 resident with a 24 hour shift. The hospital in the new site was manned by 4 medical residents on duty, 2 medical residents every 12 hours with supervision from consultants. In 2007, additional supervision was provided by two critical care specialists to oversee all patients. The patient to nurse ratio was the same in both settings, and ranges from 1:1 to 2:1.
Prior to 2005, management of hyperglycemia among critically ill patient was based on insulin infusion titrated according to target blood glucose ranges based on the attending physician's discretion. It is a non-protocol insulin infusion, in which the target range, frequency of blood glucose measurement, threshold for hypoglycemic rescue with dextrose and insulin infusion titration scale were prescribed at the discretion of the primary physician. For this study, it is referred to as physician directed insulin infusion. The insulin infusion prescribed in this cohort was not standardized. This varies among physicians which led to diverse patterns of continuous insulin infusion with respect to insulin dose titration scale; such that in 2005, the MIP protocol has been employed in our intensive care unit to standardized infusion titration of all patients who presented with hyperglycemic crisis for both medical and surgical cases. The algorithm is divided into four columns based on empirically determined insulin sensitivity. The first algorithm column was for the most insulin-sensitive patients, and the fourth algorithm column was for the most insulin resistant patients. The majority of patients started in the algorithm 1 column. Insulin resistant patients, such as those receiving glucocorticoids or receiving >80 units of insulin per day as outpatients, started in the algorithm 2 column. The insulin infusion rate was determined by the patient's blood glucose level and was measured hourly until the patient was stable and within the target range. If blood glucose targets were not achieved and the blood glucose had not decreased by at least 60 mg/dL in the preceding hour, the patient was moved to the next column. The protocol was approved by the Systems quality improvement office of our hospital. After approval, copies of protocol have been disseminated in the ICU and the emergency room for use. Medical residents were responsible for interpreting trends in blood glucose and titrating the insulin infusion according to the titration scale in the protocol. Nurses were supervised by the medical residents. No standardized orientation was performed. Efficacy was measured by comparing the rate of change of capillary blood sugar, time to achieve target blood sugar, and the number of times the blood sugar was within target range. Safety was assessed by comparing the incidence of severe hypoglycemia.
The study was conducted to determine the glycemic control among intensive care patients over a 10-year period from 2001-2009. Patients admitted prior to the implementation of MIP until the time it was adapted were evaluated. Adult patients admitted to the ICU with new hyperglycemia or with a known history of diabetes treated with insulin therapy or with any combination of oral antidiabetic agents were selected. Patients on insulin infusion based on discretion of the physician termed as PDI were identified. Patients on MIP were prescribed according to the preference of the physician. We collected baseline information, patient's characteristics and clinical conditions.
The computed sample size in comparing physician directed and Markovitz with 95% level of significance and 80% power is 412 per group. This is based on the following assumptions: incidence of hypoglycemia for the physician directed protocol is 5.1% and the incidence of hypoglycemia for Markovitz protocol is 1.4%.7
The computed sample size in comparing physician directed and Markovitz with 95% level of significance and 80% power is 412 per group. This is based on the following assumptions: incidence of hypoglycemia for the physician directed protocol is 5.1% and the incidence of hypoglycemia for Markovitz protocol is 1.4%.,sup>7
Baseline characteristics were summarized using descriptive statistics such as mean and percentage. Efficacy and safety outcomes measures were compared using blood glucose levels and percent difference between Markovitz vs Physician directed insulin control. Independent t-test was used to compare continuous variables and chi-square for the categorical variables.
The study protocol was reviewed and approved by the Institutional Review Board (IRB) of Medical City. Patients' confidentiality remained protected. The study was funded by the primary investigator.
The admission characteristics and clinical variables of interest are shown in Table 1. Data were analyzed from a total of 108 patients: 36 patients were managed using PDI while 72 patients applied MIP. 101 patients met the inclusion criteria. There were 7 patients excluded. Six patients did not complete the insulin infusion, 5 patients were excluded under PDI, and 1 from MIP. These patients died due to severe septic shock and cardiogenic shock thus the infusion was terminated prematurely. One pediatric Type 1 DM patient was excluded. There were no differences in the mean age, gender, history of diabetes, or primary admitting diagnosis between treatment groups except for patients with acute respiratory failure were significantly higher among patients in PDI. Most common reasons for admission were primary cardiovascular event (30%), severe pneumonia (27.72%) and other infections such as UTI, cellulitis and infected wounds (18.8%).
Click here to download Table 1Table 1. Baseline characteristics of patients 2001-2009
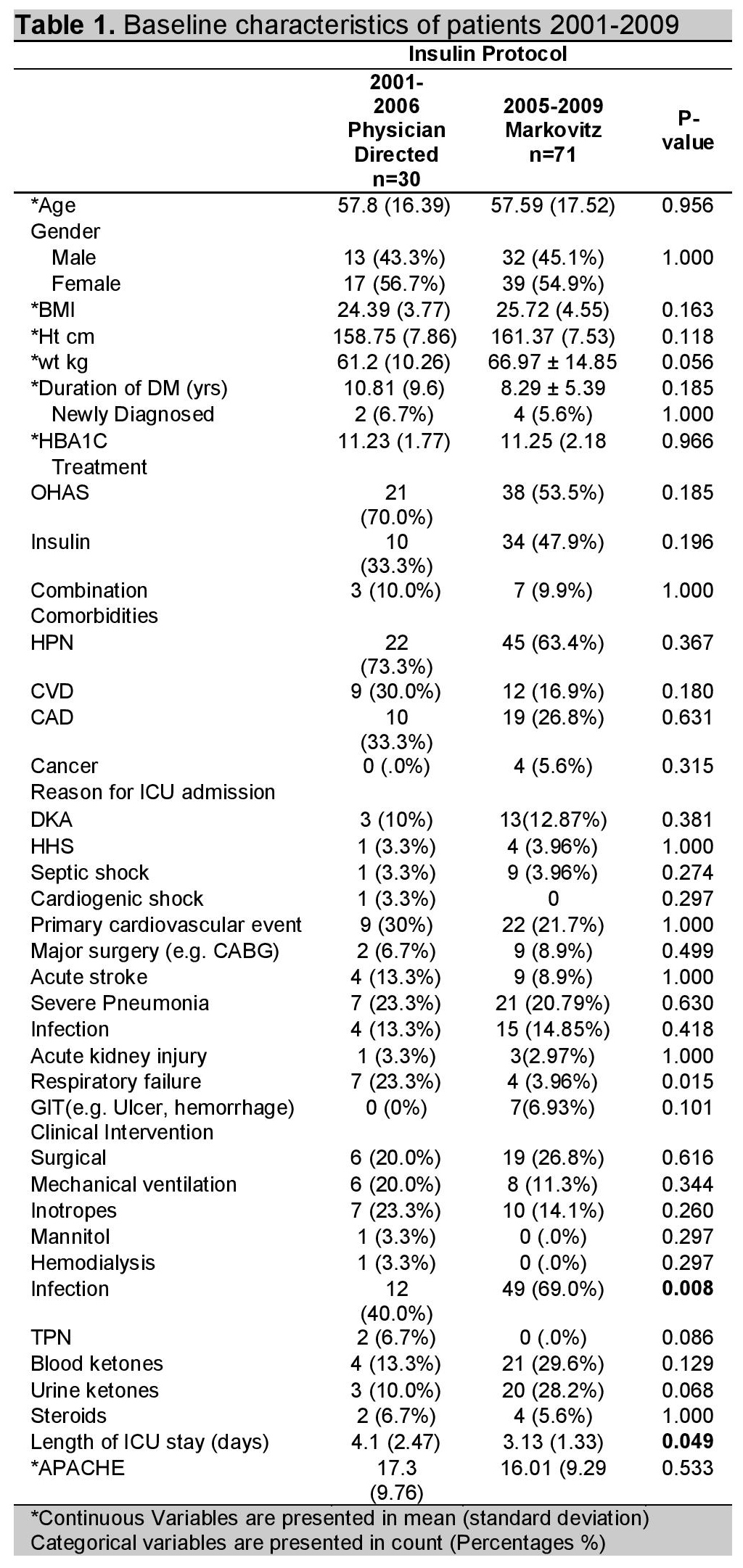
Seventy-one or 70% applied MIP protocol from the time of its implementation, while 30 or 29.7% used the physician titrated insulin drip. From 2007 to 2009, 44 patients were managed using Markovitz protocol. There were no patients managed under the PDI protocol from 2007 to 2009.
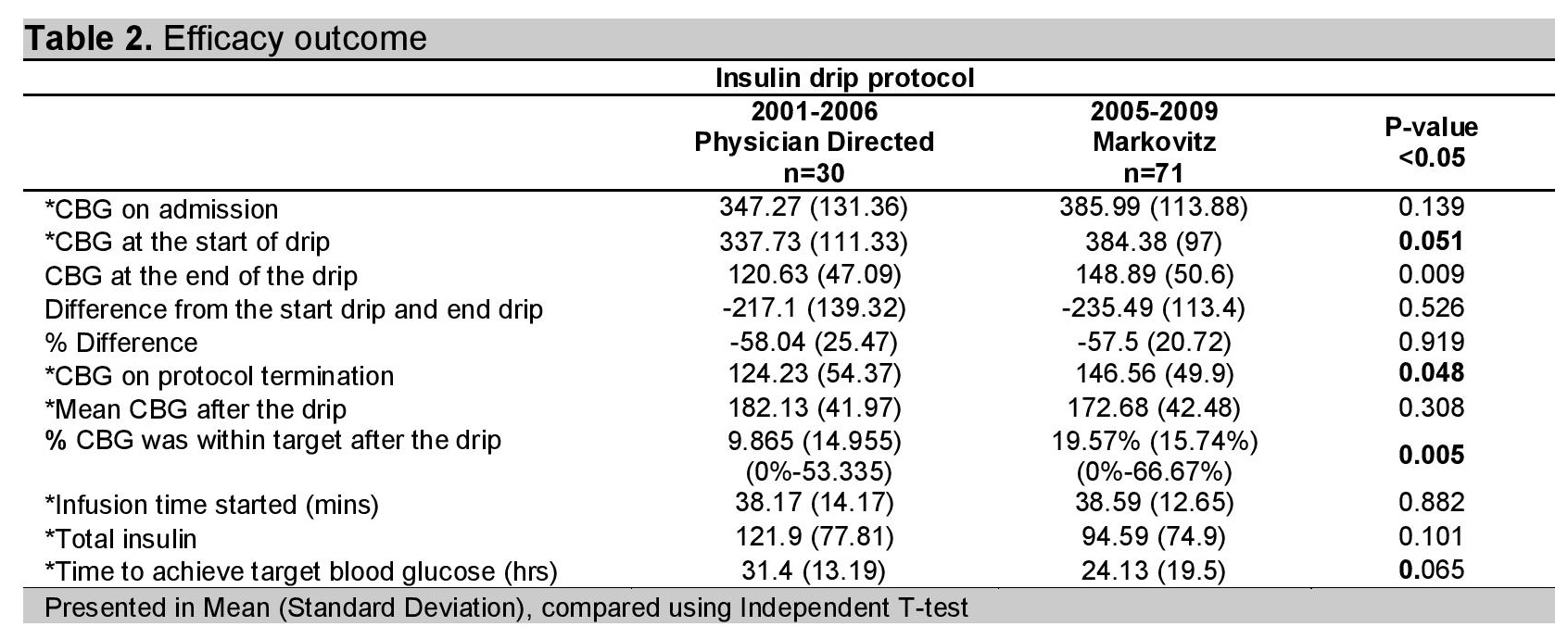
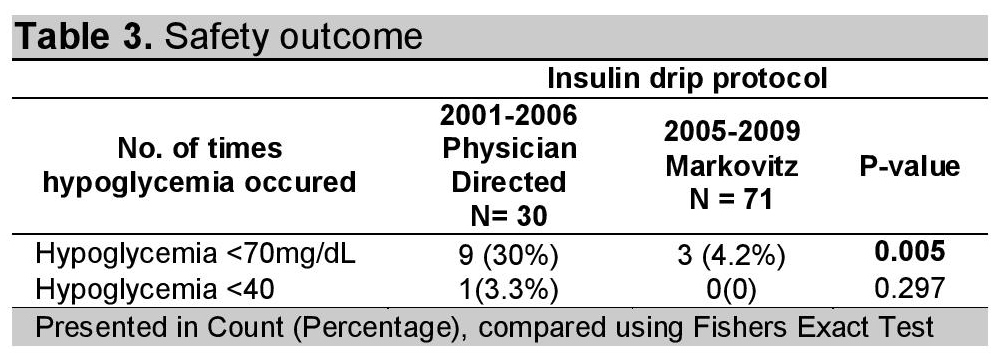
Glycemic control parameters achieved with the insulin infusion protocols are listed in Table 2. At the start of infusion, the mean blood glucose value was significantly higher for MIP compared to PDI (348.15 vs 337.73, p-value = 0.051). Patients managed using MIP reached their target more rapidly (24.13 vs 31.4 hrs), but was not statistically significant (p-value = 0.065). Blood glucose levels in MIP fell below -235.49 (SD=113.4) mg/dl with -57.5% (SD=20.72) percent difference (p-value = 0.919). Insulin requirement was minimal on the Markovitz group, requiring 94.59 (SD=74.9 units) to achieve target glycemic control compared to physician directed protocol which showed higher insulin requirement of 121.9 (SD=77.81) units (p-value =0.101). Patients on MIP achieved statistically significant control after the insulin drip with 19.57% (SD=15.74) (95% CI: 0% - 66.7%) (p = 0.005) within the target range, with a mean blood glucose of 172.68 (SD=42.48) mg/dl. Compared to patients on PID with 9.86% (SD=14.95%) (95% CI: 0% - 53.3%), with a mean glucose of 182.13 (SD=41.97)mg/dl (p-value 0.308). In addition, the MIP was associated with a significantly lower rate of hypoglycemia at 4.2% ,compared to PID at 30% (p-value =0.001). Both groups were not significant in terms of severe hypoglycemic episodes. In all cases, hypoglycemia was rapidly corrected using intravenous dextrose, per protocol. No patient in either group experienced any clinically significant adverse events due to hypoglycemia (i.e., seizures, hemodynamic compromise). From 2007 onwards, the Markovitz insulin protocol became the only insulin protocol employed in the management of hyperglycemia. The MIP was applied in a mixed population of medical and surgical patients, while the original Markovitz was used among postoperative coronary artery bypass graft patients. Supervision was provided by thoracovascular surgeons and referral to endocrinologists was made once patients were transitioned to subcutaneous insulin. While the implementation of MIP in TMC was initiated and supervised by the endocrinologists, its application in diabetic emergencies was evaluated for the first time in this study. The TMC Markovitz experience showed a mean blood glucose reduction of -235.49 (SD=113.4) with a mean percent difference of -57.5 (SD=60.3) as shown in Table 2.
Click here to download Table 2Table 2. Efficacy outcome
Click here to download Table 3
Table 3. Safety outcome
While the need for tighter glycemic control in critically ill patients is increasingly being recognized, no universal tool has been identified to facilitate intensive insulin therapy efficiently without compromising patient safety. Due to the nature of the intervention, institutional protocols that standardize prescribing and monitoring are the most appropriate strategy to ensure that the maximum benefit of the therapy is realized while ensuring patient safety. In our institution, there was a need for a protocol to guide attending physicians in prescribing and monitoring of insulin infusions to standardize the care for critically ill patients. Such that in 2005, MIP was adapted in the management of medical and surgical patients admitted in the ICU. This study is the first to compare the safety and efficacy of a Markovitz insulin protocol to a historical cohort of patients managed using our previous practice of physician directed insulin infusion. The MIP was employed in 71 patients admitted in 2005 to 2009, compared to 30 patients managed using PDI admitted in 2001 to 2006.
This study showed that Markovitz insulin protocol was comparable to physician directed insulin protocol in terms of efficacy outcome. Both methods achieved a mean blood glucose difference of -235.49 (SD=113.4) mg/dl for Markovitz insulin protocol and -217.1 (SD=139.32) for physician directed insulin protocol. The MIP achieved glycemic control within 24 hrs (SD=19.5) compared to PID. The Markovitz insulin protocol has a more constant procedural application than physician directed protocol. While the efficacy of insulin infusion protocol plays a large role in directing physician on which protocol to apply, the driving force for our institution in undertaking this study was to improve the safety of insulin infusions in the ICU. The Markovitz insulin protocol proved to be safe during its implementation and was associated with a significantly lower rate of hypoglycemia at 4.2%, compared to PID at 30% (p<0.001). Even if there was a wide spectrum of severity of illness as shown by the APACHE score, the Markovitz protocol was shown to be safe in terms of preventing over treatment.
Early randomized trials in ICU patients reported that intensified insulin treatment to achieve a target glucose between 80 mg/dL to 110 mg/dL reported a reduction in short-term and long term mortality and rates of multiorgan failure and systemic infections compared with conventionally treated patients.5 This intensive glycemic goal has been difficult to achieve without increasing the risk for severe hypoglycemia among patients in PID, with blood glucose of 120.63 (SD=47.09) mg/dl at the end of the drip. Recent multicenter trials have failed to show significant improvement in clinical outcomes or have even shown increased mortality risk with intensive glycemic control.6 Based on these reports, the American Diabetes Association (ADA) guideline8 recommended a less stringent blood glucose target between 140 mg/dL and 180 mg/dL. The MIP achieved target blood glucose of 148.89 (SD=50.6) mg/dl at the end of the infusion, more patients obtained normoglycemia after the drip and shorter ICU stay. However both infusion had similar blood glucose reduction.
The variability in insulin delivery and differences in insulin dosing in the physician directed insulin titration, resorted to implement standardized protocol. The Markovitz insulin drip was adapted by our institution to address the need for standardized management of hyperglycemia. In our study, 70% preferred to use the Markovitz protocol for glycemic control because it was easy to follow, medical residents were not hesitant to titrate insulin drip, it lessened the delays in the management as there was less time to call the attending physician for titration instruction, and nurses were guided in regulating the infusion. Though there was a greater demand for infusion pumps, and increased need for nursing staff to monitor.
By 2007 onwards, most physicians adhered to this protocol for the management of hyperglycemia and have abandoned the physician titrated insulin infusion. Our observational study design was markedly different from that of the original Markovitz insulin protocol in 2002. The Markovitz protocol has been widely applied not only for coronary artery bypass patients but also to almost all patients presenting with hyperglycemia crisis, surgical and non surgical cases. Standard management for DKA in terms of fluid resuscitation and correction of electrolytes were applied. However, the initial experience using this insulin protocol was suboptimal dose titration since critical nurse would only escalate the algorithm upon the order of the medical residents or the attending physicians. This was resolved by close supervision for every new staff hired.
The effectiveness of the Markovitz insulin protocol was assessed with regards to the presence or absence of relevant clinical variables. Blood glucose levels on the MIP were also not significantly affected by age, sex, severity of illness, or the use of corticosteroids, vasopressors or parenteral nutrition.
The TMC insulin drip protocol applied Markovitz to a wide spectrum of critically ill patients and showed it can be safely performed beyond its use as a standardized insulin protocol improved glycemic control in postoperative cardiac patients. The use of the TMC insulin drip protocol has become a standard of care among critically ill patient in our institution. The efficacy of glycemic control between the physician directed and the MIP did not indicate a significant difference (p-value=0.919) as both were managed and supervised by endocrinologists.
Several limitations of our study are identified including the small sample size, non-randomized, retrospective study design that used historical cohorts in the target population, Secondly, the before-after cohort study requires that a number of assumptions be made, specifically that the patient populations are similar and that no significant changes in practice other than the insulin protocol are made that would confound the results. We did not identify any differences other than the fact that MIP, a pre-printed algorithm form made it much easier to prescribe and follow, particularly for non-endocrinologist, leading to more frequent prescribing. There was no significant difference between the two cohorts in terms of severity of illness on admission, or interventional treatment modalities required. However, there were significantly more patients in the MIP admitted with infection. There were no significant changes in practice or studies that would influence the efficiency or approach to glycemic control other than the need for more infusion pumps, and nursing staff in the new site. These needs were appropriately provided.
Secondly, clinical outcome was not evaluated in this study. Thirdly, the need to modify Markovitz protocol from blood glucose goal of 120-199 mg/dL to 140-180mg/dl based on the ADA guideline should be undertaken.
This study evaluated the successful implementation of a safe and effective insulin protocol. The MIP provides better glycemic control in critically ill patients than PDI infusion with a greater percentage of glucose measurements maintained within target range, without an increased risk of severe hypoglycemia. Future studies should determine whether MIP will result in improved patient outcomes for patients admitted in the ICU.
The Markovitz insulin protocol was preferred over physician directed insulin protocol which led to its eventual disuse.
1. Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE: Hyperglycemia: An independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002; 87:978-982. http://dx.doi.org/10.1210/jcem.87.3.8341.
2. Krinsley JS. Effect of intensive glucose management protocol on the mortality of critically ill adult patients. Mayo Clin Proc. 2004; 79:992-1000 [erratum in Mayo Clin Proc 2005; 80:1101].
3. Furnary AP, Zerr KJ, Grunkemeier GL, Starr A. Continuous intravenous insulin infusion reduces the incidence of deep sternal wound infection in diabetic patients after cardiac surgical procedures [with discussion]. Ann Thorac Surg. 1999;67:352-362. http://dx.doi.org/10.1016/S0003-4975(99)00014-4.
4. Malmberg K, Ryden L, Efendic S, et al. Randomized trial of insulin-glucose infusion followed by subcutaneous insulin treatment in diabetic patients with acute myocardial infarction (DIGAMI study): Effects on mortality at 1 year. J Am Coll Cardiol. 1995;26:57-65. http://dx.doi.org/10.1016/0735-1097(95)00126-K.
5. Van den Berghe G, Wilmer A, Hermans G, Meersseman W, Wouters PJ, Milants I, et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006; 354:449-461. http://dx.doi.org/10.1056/ NEJMoa052521.
6. Finfer S, Chittock DR, Su SY, et al. NICE-SUGAR Study Investigators. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360:1283-1297. http://dx.doi.org/ 10.1056/NEJMoa0810625.
7. Markovitz LJ, Wiechmann RJ, Harris N, Hayden V, Cooper J, Johnson G, et al: Description and evaluation of a glycemic management protocol for patients with diabetes undergoing heart surgery. Endocr Pract. 2002 Jan-Feb;8(1):10-8.
8. American Diabetes Association. Standards of Medical Care in Diabetes-2013. Diabetes Care. 2013; 36 (Suppl. 1):S11-66.
9. Bode BW, Braithwaite SS, Steed RD, Davidson PC: Intravenous insulin infusion therapy: Indications, methods, and transition to subcutaneous insulin therapy. Endocr Pract. 2004; 10 (Suppl. 2):71-80.
10. Kanji S, Singh A, Tierney M, Meggison H, McIntyre L, Hebert PC. Standardization of intravenous insulin therapy improves the efficiency and safety of blood glucose control in critically ill adults. Intensive Care Med. 2004 May; 30(5):804-10.
11. Reynolds R. Insulin use in the hospital: An evolving therapeutic paradigm. Lab Medicine. August 2008; 39: 491-495. http://dx.doi.org/10.1309/87FW3DAAQFCEUU9. 12. Balfe D. Implementation of a safe glycemic control protocol in hospitalized intensive care unit patients. ICU Director. 2010; 1(5):271-276. http://dx.doi.org/10.1177/1944451610384357. 13. Wilson M, Weinreb J, Soo Hoo G. Intensive insulin therapy in critical care: A review of 12 protocols. Diabetes Care. 2007; 30:1005-1011. doi: 10.2337/dc06-1964. http://dx.doi.org/10.2337/dc06-1964. 14. Ku SY, Sayre CA, Hirsch IB, Kelly JL. New insulin infusion protocol improves blood glucose control in hospitalized patients without increasing hypoglycemia. Jt Comm J Qual Patient Saf. March 2005; 31-141-147. 15. Trence D, Kelly J, et al. The rationale and management of hyperglycemia for in patients with cardiovascular disease: Time for change. JCEM. June 2003; 88 (6): 2430-2437. 16. Finney SJ, Zekveld C, Elia A, Evans TW: Glucose control and mortality in critically ill patients. JAMA. 2003; 290:2041-2047. http://dx.doi.org/10.1001/jama.290.15.2041. 17. Goldberg PA, Siegel MD, Sherwin RS, et al. Implementation of a safe and effective insulin infusion protocol in a medical intensive care unit. Diabetes Care. 2007;27: 461-467. http://dx.doi.org/ 10.2337/diacare.27.2.461. 18. Goldberg PA, Siegel MD, Sherwin RS, Halickman JI, Lee M, Bailey VA, Lee SL, Dziura JD, Inzucchi SE. Implementation of a safe and effective insulin infusion protocol in a medical intensive care unit. Diabetes Care. 2004;27:461-467. http://dx.doi.org/10.2337/ diacare.27.2.461. 19. Malesker MA, Foral PA, McPhillips AC, Christensen KJ, Chang JA, Hilleman DE. An efficiency evaluation of protocols for tight glycemic control in intensive care units. Am J Crit Care. 2007;16:589-598. 20. Newton CA, Smiley D, Bode BW, et al. A comparison study of continuous insulin infusion protocols in the medical intensive care unit: computer-guided vs. standard column-based algorithms. J Hosp Med. 2010 October; 5(8):432-437. http://dx.doi.org/10.1002/jhm.816. 21. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985 Oct;13(10):818-29. Click here to download Appendix 1.Appendix 1.Markovitz Insulin Drip Protocol
Authors are required to accomplish, sign and submit scanned copies of the JAFES Declaration that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere.
Consent forms, as appropriate, have been secured for the publication of information about patients; otherwise, authors declared that all means have been exhausted for securing such consent.
The authors have signed disclosures that there are no financial or other relationships that might lead to a conflict of interest. All authors are required to submit Authorship Certifications that the manuscript has been read and approved by all authors, and that the requirements for authorship have been met by each author.