Diabetes mellitus (DM) is classified into 4 major categories (Type 1 Diabetes Mellitus (T1D), Type 2 Diabetes Mellitus (T2D), Gestational Diabetes Mellitus (GDM), other types due to other specific causes that reflect its underlying pathophysiology.1 Immunologic markers and assessment of β-cell function are useful tools when clinical parameters alone are inadequate to differentiate between T1D and T2D.
There are five antibodies [Islet Cell Antibody (ICA), Insulin Autoantibody (IAA), Glutamic Acid Decarboxylase 65 Antibody (GAD65Ab), antibodies to Tyrosine Phosphatase like IA-2 (IA-2Ab) and Zinc Transporter 8 (ZnT8)] used to test for autoimmunity in DM. GAD65Ab is detected in 70-80% of cases during the evolution of a patient with T1D. It is likewise the most sensitive marker (91%) for detecting multiple antibody positivity compared with ICA (82%).2
β-cell functional reserve can be assessed with a Mixed-Meal Tolerance Test (MMTT) or Glucagon Stimulation Test (GST) by measuring fasting and post stimulus C-peptide levels. In a recent study, basal C-peptide of less than 0.6 ng/ml indicates absolute insulin deficiency; more than 0.6 ng/ml suggests T2D or maturity onset diabetes in the young (MODY) in a patient with presumed T1D, and more than 3 ng/ml suggests MODY or T2D in young onset DM at diagnosis.3
The classification of DM is often difficult based on clinical parameters alone. The face of diabetes has evolved over the years with the increasing prevalence of obesity. Younger patients are frequently diagnosed with T2D and obesity in T1D is becoming more common. In these equivocal circumstances, immunologic markers and assessment of β-cell function are important tools to differentiate between T1D and T2D but is underutilized in routine clinical practice.4 This gray area between the types of DM is discussed and how accurate diagnosis leads to proper management.
The patient is a 22-year-old Filipino male who was admitted due to diabetic ketoacidosis (DKA). He did not have a prior history of DM but experienced polydipsia, polyuria and 8 kg weight loss one month prior to admission. He eventually developed generalized weakness and fatigue.
The patient has an unremarkable past medical history. Family history includes a diabetic mother on metformin, and a hypertensive grandmother. There was no autoimmune disease in the family.
On examination, patient's blood pressure was 140/90 mm Hg, RR 20 breaths per minute, heart rate of 79 per minute, and temperature of 37C. He is morbidly obese (BM 41.1; W:H 1.29) with acanthosis nigricans. Initial work-up showed blood glucose of 462 mg/dl, arterial blood gas was uncompensated metabolic acidosis and +3 urinary ketones. There were no infections noted. He was admitted as a case of DKA and was managed accordingly with fluid and an insulin drip. Other work-ups showed absence of microvascular complications.
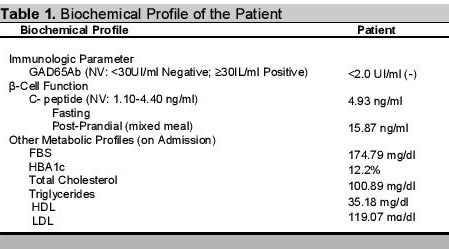
Patient was discharged with NPH insulin 40 u SC in AM and 20 u SC in PM, metformin 500 mg/tab BID and amlodipine 5mg/tab QD. One month after discharge, patient was noncompliant with insulin but noted to have good glycemic control with metformin alone (preprandial CBGs 103-133 mg/dl). He was also noncompliant with his antihypertensive medication but BP monitoring at home was stable at 120/80 mm Hg. We requested for C-peptide and GAD65Ab two weeks after discharge to determine whether the patient has T1D or T2D. GAD65Ab was negative and C-peptide was detectable at fasting state and increased after a mixed-meal diet. Patient has no pancreatic islet antibodies and has adequate β-cell functional reserve, and was diagnosed as unprovoked A-β+ Ketosis Prone Type 2 DM. Metformin was eventually discontinued after 6 months. One year after the diagnosis, he was able to achieve good glucose control with HbA1c of 6.2%, FBS 4.3 mmol/L with diet alone.
Click here to download Table 1Table 1. Biochemical profile of the patient.
The increasing incidence of ketoacidosis without precipitating cause has been reported among pediatric and adult patients with T2D, primarily among Africans, African Americans and other minority ethnic groups.5-8,14 These patients are usually obese and have a strong family history of DM. They are able to regain sufficient β-cell function and insulin sensitivity within months of treatment allowing the discontinuation of insulin therapy. The overlapping features of both types of diabetes have been previously referred to as 'atypical diabetes', 'diabetes type 1 ½', and has been recently called 'ketosis prone DM (KPD)'.
A patient with KPD has severe hyperglycemia with associated ketosis that can be managed without insulin after a few months; and can maintain acceptable glycemic control with diet or oral agents. Ketoacidosis is not rare in T2D but occurs in settings of acute illness and infections. Our patient had a phenotype compatible with T2D but was diagnosed with DM after an episode of DKA which is a presentation more commonly seen among those with T1D.. Our patient had no precipitating cause for DKA and was later noted to have near-normoglycemic remission from insulin and oral hypoglycemic agents (OHA).
Assessment of autoimmunity and β-cell secretory reserve of newly diagnosed DM patients after 1-3 weeks of resolution of the index DKA episode was reported to predict the ability of the newly diagnosed KPD patient to discontinue insulin and remain in near-normoglycemic remission. They are divided into four groups based on autoimmunity and β-cell function (Aβ) classification scheme: those patients with autoimmune disease with absent (A+β-) or preserved (A+β+) β-cell function and those without autoimmune diabetes with absent (A-β-) or preserved (A-β+) β-cell function.5
Patients with negative β-cell function, with or without autoimmune markers, have clinical and biochemical characteristics of T1D implying lifelong insulin dependency. These groups are comparable to the American Diabetes Association (ADA) classification of autoimmune and idiopathic T1D respectively.9
Adequate β-cell function after an episode of DKA, regardless of autoimmunity is compatible with T2D. Types A+β+, and A-β+ are termed as 'ketosis prone type 2 DM.'5 β-cell reserve determines the definitive management of diabetes and is the best predictor of remission in KPD. Insulinopenia will require lifelong insulin (T1D), while those with adequate β-cell function benefit from lifestyle modification and OHA.
Autoimmunity, on the other hand, is a determinant of future β-cell function. Presence of autoantibodies (GAD65Ab) at diagnosis is highly predictive for future insulin use at a rate of 1-2% per year after 1-5 years of therapy with diet, exercise, OHA.5,10,11 Fifty percent of DKA patients classified as A+β+ (represents 7%) have progressive decline of β-cell function eventually becoming insulin requiring following a clinical course that resembles T1D within the first two years of diagnosis. Serial C-peptide determination is recommended every 6 months to trackβ-cell deterioration.5,12,14
The majority of KPD is represented by A-β+ (74%), whose clinical course mimics that of T2D after resolution of DKA. They are able to achieve near-normoglycemic remission within 10 weeks (~70%) and 40% remain insulin independent a decade after diagnosis. The cause of the sudden, severe but reversible β-cell dysfunction is unknown in 50% of cases (unprovoked), whereas the other half is precipitated by an acute illness or noncompliance with medications (provoked). The unprovoked ketosis among β-cell adequate groups is postulated to be secondary to impaired ketone oxidation and fatty acid utilization. The provoked A-β+ KPD group has better glycemic control (twice the frequency of attaining Hba1c <7%), 2-fold greater improvement in β-cell function (after 12 months of treatment), and a higher rate of insulin independence.5,12-14
All newly diagnosed KPD patients should be discharged with basal insulin regimen after resolution of DKA. Any attempt to discontinue insulin should be based on the Aβ classification scheme. If blood glucose monitoring of β+ patients after 2 weeks is within ADA target goals (preprandial 90-130mg/dl; postprandial <180mg/dl), the insulin dose can be decreased by 50% and is reassessed after another week. If the patient achieves ADA target by the second visit, insulin regimen can be discontinued but close monitoring is warranted.5 If blood glucose is uncontrolled, insulin regimen is intensified.5
Our patient (unprovoked A-β+ KPD) has sufficient insulin secretion that enables him to sustain good glycemic control through diet alone. Absence of autoimmunity makes him less susceptible to future β-cell failure and recurrence of DKA. However, we need to be vigilant since the patient's DKA is unprovoked and an underlying β-cell dysfunction may be present. Close follow-up is prudent to avoid recurrence of life-threatening ketosis, to anticipate complications and to monitor eventual shifts in the therapy of patients with KPD.
Diabetes can present in various ways. Phenotypical characteristics are not enough to classify them into either T1D or T2D. Tests for autoantibodies and β-cell function are recommended for patients with overlapping features of both types of DM, and may be considered for patients on insulin who want to be shifted to oral agents, and patients who are uncontrolled with oral agents and are suspected to have inadequate β-cell function. These tests will guide clinicians regarding diagnosis, response to treatment and anticipation of complications.
1. American Diabetes Association. Standards of Medical Care in Diabetes - 2014. Diabetes Care. January 2014;37(Suppl 1):S14-80. http://dx.doi.org/10.2337/dc14-S014.
2. Pihoker C, Gilliam L, Hampe C, et al. Autoantibodies in diabetes. Diabetes. December 2005;54(Suppl 2):S52-61. http://dx.doi.org/ 10.2337/diabetes.54.suppl_2.S52.
3. Jones AG, Hattersley AT. The clinical utility of C-peptide measurement in the care of patients with diabetes. Diabet Med. July 2013;30(7):803-817. http://dx.doi.org/ 10.1111/dme.12159.
4. Bingley PJ. Clinical applications of diabetes antibody testing. J Clin Endocrinol Metab. Jan 2010;95(1):25-33. http://dx.doi.org/ 10.1210/jc.2009-1365.
5. Balasubramayam, A, Nalini R, Harpe CS, Maldonado M. Syndromes of ketosis-prone diabetes mellitus. Endocr Rev. 2008;29(3):292-302. http://dx.doi.org/10.1210/er.2007-0026.
6. Sobngwi E, Vexiau P, Levy V, et al. Metabolic and immunogenetic prediction of long-term insulin remission in African patients with atypical diabetes. Diabet Med. 2002;19:832-835.
7. Balasubramanyam A, Zern JW, et al. New profiles of diabetic ketoacidosis: Type 1 vs type 2 diabetes and the effect of ethnicity. Arch Intern Med. October 1999. 159(19):2317-2322. http://dx.doi.org/10.1001/archinte.159.19.2317.
8. Yamada K, Nonaka K: Diabetic ketoacidosis in young obese Japanese men. Diabetes Care. June 1996.19(6):671. http://dx.doi.org/10.2337/diacare.19.6.671a.
9. American Diabetes Association. Diagnosis and classification of diabetes. Diabetes Care. January 2013; 36(Suppl 1):S67-74. http://dx.doi.org/ 10.2337/dc13-S067.
10. Tuomi T, Groop LC, Zimmet PZ, et al. Antibodies to glutamic acid decarboxylase reveal latent autoimmune diabetes mellitus in adults with a non-insulin-dependent onset of disease. Diabetes. February 1993; 42(2): 359-362. http://dx.doi.org/10.2337/diab.42.2.359.
11. Jameson JL, De Groot LJ, et al. Endocrinology: Adult and pediatric, 6th Ed. Philadelphia: Saunders Elsevier, 2010.
12. Maldonado M, Hampe CS, et al. Ketosis-prone diabetes: Dissection of a heterogeneous syndrome using an immunogenetic and beta-cell functional classification, prospective analysis, and clinical outcomes. J Clin Endocrinol Metab. November 2003; 88(11):5090-5098. http://dx.doi.org/10.1210/jc.2003-030180
13. Patel SG, Hsu JW, Jahoor F, et al. Pathogenesis of A-β+ ketosis-prone diabetes. Diabetes. March 2013; 62(3):912-922. http://dx.doi.org/10.2337/db12-0624. 14. Umpierrez GE. Ketosis-prone type 2 diabetes: Time to revise the classification of diabetes. Diabetes Care. December 2006; 29(12):2755-2757. http;//dx.doi.org/ 10.2337/dc06-1870.
This patient exemplifies the increasing difficulty in differentiating between Type 1 and Type 2 DM among young patients, based on clinical grounds alone. This is especially true in the presence of obesity. The category to which the patient in the case was classified would correspond to Type 1 DM or monogenic diabetes (maturity onset diabetes of the young, MODY). Both will have A-β+* designation with C-peptide between 0.6 and 2 ng/mL. A young patient eventually diagnosed to have Type 2 DM is a cause for alarm. A comparison of the outcomes among diabetic individuals showed a two- fold increase in case fatality in young-onset T2DM compared with T1DM of a similar age of onset and disease duration.1 This is accounted for by the greater number of cardiovascular deaths,1 which has thus created the notion that young-onset T2DM is a more aggressive disease compared to T1DM. Thus, the prevention of obesity among children cannot be over-emphasized, as this is the single most important factor for the rising trend in the occurrence of Type 2 DM in this age group.
Lorna R. Abad, MD, FPPS, FPSPMEPediatric Endocrinologist,
University of the Philippines-Philippine General Hospital
________
*A- means negative antibody while β+ means reserved beta cell function
References
1. Constantino MI, Molyneaux L, Limacher-Gisler F, et al. Long-term complications and mortality in young-onset diabetes. Diabetes Care. 2013;36(12):3863-3869. http://dx.doi.org/10.2337/dc12-2455.
Authors are required to accomplish, sign and submit scanned copies of the JAFES Declaration that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere.
Consent forms, as appropriate, have been secured for the publication of information about patients; otherwise, authors declared that all means have been exhausted for securing such consent.
The authors have signed disclosures that there are no financial or other relationships that might lead to a conflict of interest. All authors are required to submit Authorship Certifications that the manuscript has been read and approved by all authors, and that the requirements for authorship have been met by each author.