Pheochromocytoma is a rare cause of secondary hypertension originating from the chromaffin cells of the adrenal glands or paragangliomas from the sympathetic nervous system or parasympathetic ganglia. Worldwide, the prevalence of this disease is 1to 8 per million cases, but may occur frequently in certain populations.1 In the Philippines, a hospital census done during the 1980's, showed that only four of 101 cases of secondary hypertension were found to have pheochromocytoma.2 In the Philippine General Hospital, only four patients have biopsy proven pheochromocytoma during the past five years.3
Definitive treatment is resection of the mass, either by laparoscopy or open surgery. Preoperative blockade is essentialto improve intraoperative hemodynamic stability and minimize morbidity during resection. Phenoxybenzamine, a non-selective alpha adrenergic blocker, has been widely used as preoperative blockade for this condition, but is unavailable in the Philippines. Selective alpha-1blockers such as prazosin, doxazosin and terazosin have been documented in case reports as suitable preoperative drugsto reduce blood pressure in pheochromocytoma patients.
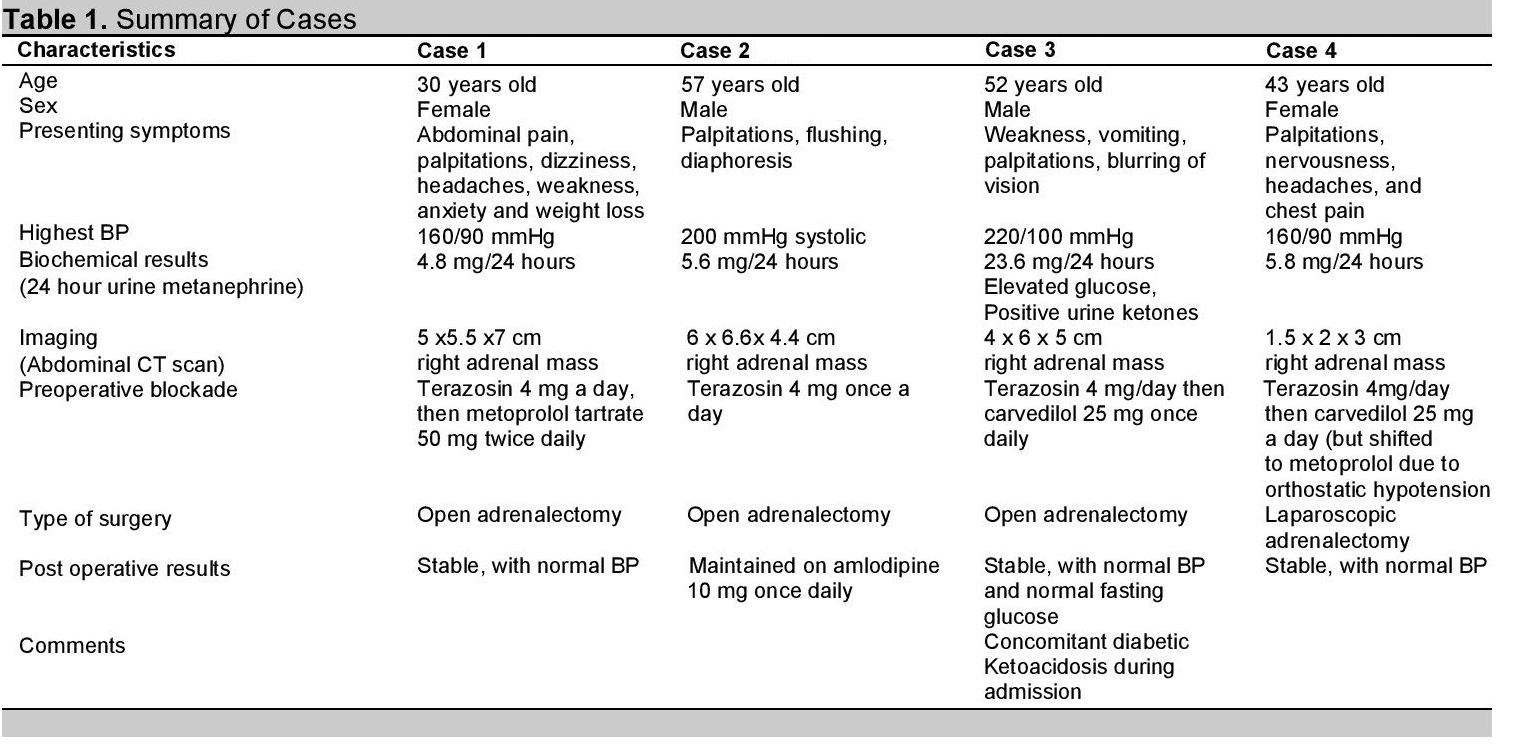
Case 1A 30-year-old Filipino female was complaining of intermittent right flank pain that radiated to the back for four years. She was initially seen at a hospital in Batangas City and was managed for nephrolithiasis. The persistent pain prompted a request for an abdominal CT scan, which revealed a 4 x 4.5 x 5.3 cm right adrenal mass. She was given pain relievers and advised surgery, but due to financial constraints, was lost to consult. During that time, she continued to have the flank pains and, she began to experience episodes of palpitations, dizziness, headaches, weakness, bouts of anxiety and weight loss. She would also have elevated blood pressure, with the highest BP of 160/90 mm Hg. She had normal fundoscopic findings. A repeat abdominal CT scan showed the right adrenal mass had grown to 5 x 5.5 x 7 cm. She was given amlodipine 10 mg/tab for the hypertension and was referred to the Philippine General Hospital. At our institution, a 24-hour urine metanephrine was done and results yield 4.8 mg/24 hours (Normal Value < 1 mg/day).
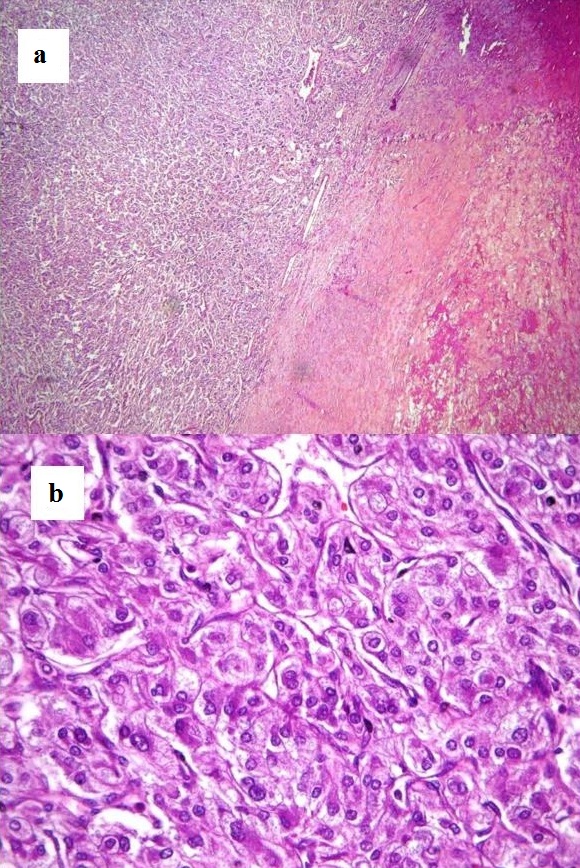
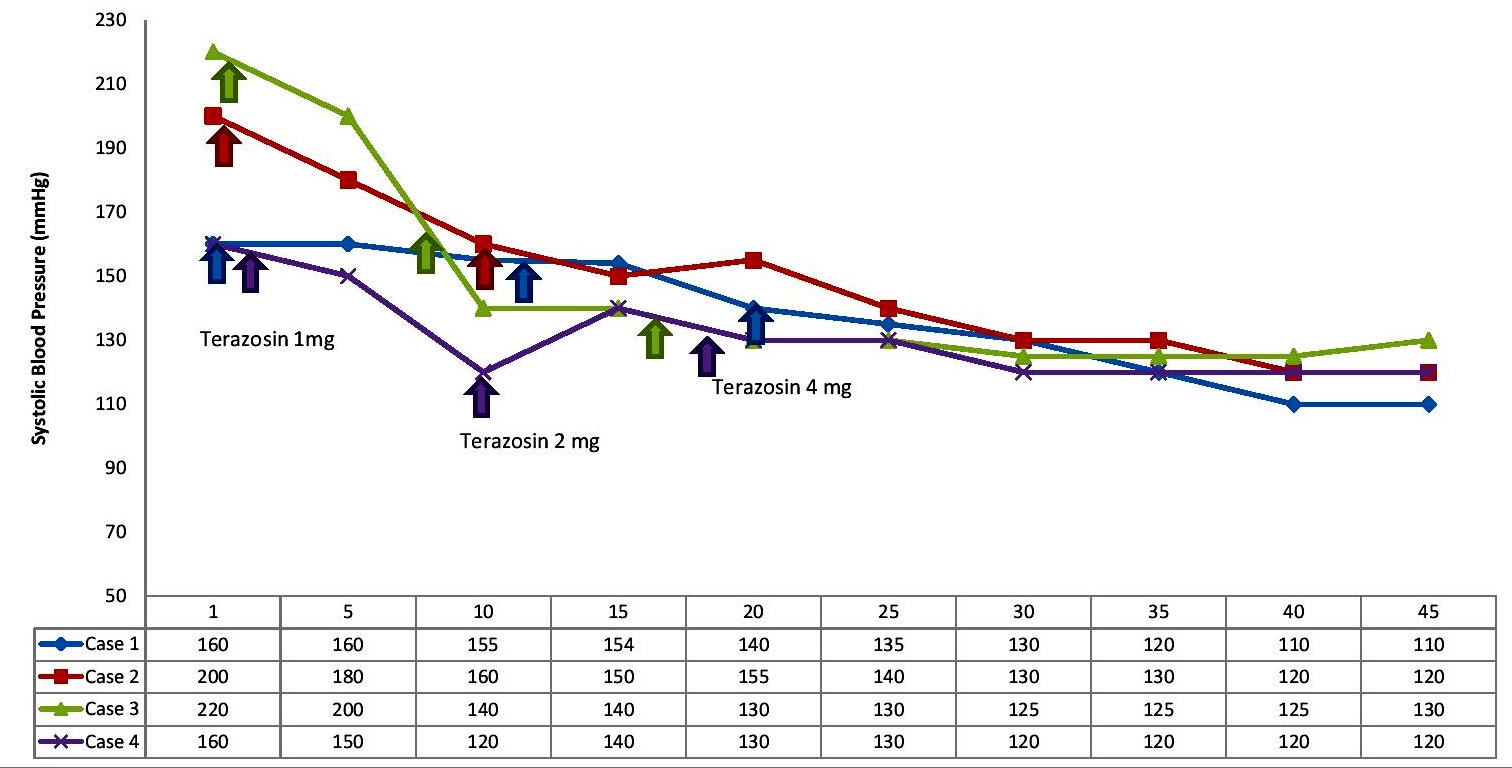
She was started on terazosin, initially dosed at 1 mg/tab ½ tab once a day.After 2 weeks, her blood pressure was still 160/90 mm Hg, the dose of terazosin was increased to 2 mg/tab once a day. With the increase in dose, her BP decreased and reached 140/90 mm Hg.When the dose of terazosin was increased to 4 mg/day on her third follow-up, her blood pressure was sustained at 110-120/70-80 mm Hg. Metoprolol tartrate 50 mg/tab twice a day was subsequently added to her regimen and her heart rate was controlled to 50-60 beats per minute. During this time, her BP still ranged from 110-120/70-80 mm Hg with the use of the alpha and beta blockers. Due to financial constraints, it was a month before she underwent open adrenalectomy which revealed a 10 cm right adrenal mass. Histopathologic findings showed alveolar or trabecular patterns of polygonal or spindle-shaped cells in a rich vascular network (Figure 1). Her blood pressure was stable at 100/60 mm Hg post-operatively. She was discharged after two weeks and is presently asymptomatic.
Click here to download Figure 1Figure 1. Histopathologic results of the adrenal mass on low power microscopy (a) with an anastomosing trabecular pattern and high power (b) showing alveolar pattern of cells.
Case 2
A 57-year-old Filipino male was complaining of intermittent nape pains associated with elevation of blood pressure for two years. His blood pressure ranged from 160-180/90-100 mm Hg and was associated with palpitations, diaphoresis and flushing. He was started on metoprolol tartrate 50 mg/tab twice daily, but his condition did not improve. He had multiple admissions at the emergency room for elevations of blood pressure, with BP as high as 200 mm Hg systolic. His primary doctor requested an abdominal CT scan which revealed a 6 x 6.6 x 4.4 cm right adrenal mass. He was referred to the Philippine General Hospital for management. A 24-hour urine collection for urine metanephrine was done and showed a value of 5.6 mg/24 hours.
He was started on terazosin 2 mg/tab once a day for control of his blood pressure and on follow-up after 15 days, his BP decreased to 150/90 mm Hg (Figure 2). The dose of terazosin was increased to 4 mg/day and this further controlled his BP to 130/80 mm Hg by the next follow-up. His BP was maintained prior to surgery with BP readings recorded less than 130/80 mm Hg. After a month, he underwent open adrenalectomy which revealed a 6 cm adrenal mass that was signed out by a pathologist as pheochromocytoma. His symptoms improved after the surgery. He is presently on amlodipine 10 mg/tab once daily for blood pressure.
Case 3A 52-year-old Filipino male was rushed to the emergency room of the Philippine General Hospital for a two day history of vomiting and weakness. He is a diagnosed diabetic for two years and had concomitant hypertension with associated symptoms of weakness, palpitations and blurring of vision. He was on clonidine 75 mcg/tab twice daily and verapamil once daily for the hypertension, and unrecalled oral hypoglycemic agents for the diabetes. One week prior to the admission at the ER, he experienced dysuria, fever and flank pains. At the ER, his blood pressure was 220/100 mm Hg, blood sugar was 500 mg/dl, positive urine ketones, bicarbonate of 8.0, and potassium of 5.3 mg/dl.Fundoscopic findings showed hypertensive retinopathy stage 1. He was initially managed as a case of diabetic ketoacidosis and hypertensive emergency. He was started on intravenous insulin for the DKA and intravenous nicardipine drip for the hypertension. His blood sugars normalized after a few hours but his blood pressure had intermittent elevations despite the nicardipine. Once the patient's blood sugar and blood pressure were stabilized, work up for pheochromocytoma was done. Results showed a 24-hour urine metanephrine of 23.6 mg/day and an abdominal CT scan revealed a 4 x 6 x 5 cm right adrenal mass.
Terazosin was started at 4 mg/tab once a day. After a week, his blood pressure readings ranged between 120-140/70-90 mm Hg. Subsequent follow-up while on terazosin 4 mg/day showed a sustained BP of 130/80 mm Hg, and carvedilol 25 mg/tab once daily was added to control the patient's BP and tachycardia (Figure 2). After a few months, with BP controlled at 130/80 mm Hg, he underwent open adrenalectomy and it revealed a 6 cm adrenal mass that was read as pheochromocytoma on histopathology. He is presently asymptomatic and does not have elevations of blood sugar as well as blood pressure.
Click here to download Figure 2Figure 2. Summary of blood pressures of patients using Terazosin as preoperative blockade.
Case 4
A 43-year-old Filipino female was complaining of intermittent episodes of elevated blood pressure, palpitations, nervousness, headaches and chest pains. She had consulted different doctors and was maintained on metoprolol tartrate 100 mg/tab once daily, amlodipine 10 mg/tab once daily, and clonidine 75 mcg/tab taken orally only when BP >160/90 mm Hg. She was also on an anxiolytic for the palpitations. She had frequent consults at the emergency room, but would be sent home once her BP becomes normal.
She consulted the Philippine General Hospital for management of blood pressure. Work up revealed an elevated 24-hour urine metanephrine at 5.8 mg/day and an abdominal CT scan showed a 1.5 x 2 x 3 cm right adrenal mass. She was started on terazosin 1 mg/tab once daily and the dose was escalated weekly. On the second week, when carvedilol 25 mg/tab ½ tab twice daily was added to the regimen, patient experienced dizziness and weakness when standing with BP at120/70 mm Hg. Carvedilol was then shifted to metoprolol succinate 50mg/tab once daily with improvement of symptoms. Her blood pressure increased to 140/90 mm Hg on the third week, so the dose of terazosin was increased to 4 mg/tab. This stabilized her BP to 130/80 mm Hg on subsequent weeks (Figure 2). She was scheduled for laparoscopic adrenalectomy after one month and surgery revealed a 2 x 3 cm adrenal mass, which was, a pheochromocytoma on final histopathology. Presently, her BP is maintained at 110-120/70-80 mm Hg with no maintenance anti-hypertensive medications.
Click here to download Table 1Table 1. Summary of cases.
Pheochromocytomas and paragangliomas are neuroendocrine tumors derived respectively from adrenal chromaffin cells and extra-adrenal paraganglia, and these tumors can cause secondary hypertension. The sympathetic nervous system activity is enhanced and this over-activity is integral to the maintenance of elevated blood pressure. The excess release and high levels of catecholamines; norepinephrine, epinephrine, and to a lesser extent dopamine, account for the typical presentation of pheochromocytoma4 . Many adrenal tumors can produce both norepinephrine and epinephrine, or are predominantly epinephrine-secreting tumors, while most extra-adrenal tumors produce predominantly norepinephrine. Epinephrine-secreting pheochromocytomas produce episodic signs and symptoms such as palpitations, light-headedness or syncope, anxiety and hyperglycemia more frequently, while norepinephrine-producing tumors are more often associated with continuous symptoms and signs including hypertension, sweating and headaches.4-6
The definitive treatment for pheochromocytomais surgical removal of the mass. Prior to surgery, appropriate anti-hypertensive medications are used to manage hypertension, control of symptoms and prepare patients for surgery. In most centers, an alpha blocking agent followed by the use of a beta blocker is one approach for treatment. Phenoxybenzamine, a non-selective alpha receptor blocker, has been widely used since the 1950s as the mainstay of pre- and perioperative control of blood pressure in patients with pheochromocytoma.7,8 It has the advantage of having a long duration of action, allowing twice daily oral ingestion, and produces a non-competitive blockade as a result of covalent binding of the drug to the receptor. The non-selectivity of phenoxybenzamine prevents the effects of surges of catecholamine release during the preoperative preparatory period. However, because of its non-selectivity, it also blocks the alpha-2 receptors, especially those on the pre-synaptic membrane of adrenergic neuron terminals particularly at cardiac sympathetic nerve endings, leading to undesirable chronotropic and inotropic effects.7 The non-competitive covalent binding in the alpha receptors results in alkylation of the alpha receptor by a highly reactive carbonium ion formed by the cleavage of the tertiary amine of phenoxybenzamine. This leads to marked, prolonged blockade in the postoperative period, despite stopping the drug in the first 48 hours after surgery, and this may result inpersistent central alpha-2 blockade. Patients are often very somnolent, would experience headaches, stuffy nose and consistent and marked postural hypotension.7,9
Unfortunately, phenoxybenzamine is unavailable in the Philippines. Selective alpha-1 blockers have been used in lieu of phenoxybenzamine and to prevent the usual side effects of the non-selectivity of the drug. A retrospective study showing different preoperative medical management for laparoscopic treatment of pheochromocytoma was demonstrated at the Mayo Clinic and Cleveland Clinic in the United States. Patients from the former received predominantly phenoxybenzamine, while patients from the Cleveland Clinic were predominantly treated with selective alpha-blockers (either prazosin, doxazosin and terazosin). The intraoperative systolic and mean BP trends were lower, and the trend of having a shorter duration of hypertension is seen in the phenoxybenzamine group. However, there is less use of beta blockers and a relatively shorter time of hypotension post-operatively with selective alpha-1 blockers. There were no differences in the postoperative surgical outcome in both groups and the hospital stay was comparable in both groups.10
Prazosin, a drug with high first-pass metabolism, was used with the highest dose of 12 mg daily. Several case series showed good control of blood pressure with prazosin as their pre-operative drug of choice.11-13 However, a study by Russell et al claimed that phenoxybenzamine treatment provided better intraoperative stability to prazosin. The hypotensive effect of prazosin was due to the immediate effects of arteriolar dilation in a patient who has been in a state of venoconstriction and arteriolar vasoconstriction with low circulating blood volume.14 Doxazosin has a high bioavailability, does not readily cross the blood-brain barrier and has a long duration of action allowing a once-a-day dosing. A case series showed that 20 patients with pheochromocytoma were treated successfully with doxazosin with doses from 2 to 8 mg/day. Only one patient in the series developed postural hypotension. Preoperative control of arterial pressure was at least good as that achieved with phenoxybenzamine.9
Terazosin is an alternative selective alpha-1 receptor blocker with pharmacokinetic characteristics similar to those of doxazosin but with a shorter half-life. The initial dose is 1 mg with a maximum dose of 20 mg at night. There is a paucity of cases where terazosin was used as a preoperative drug for BP control in pheochromocytoma. All our patients received terazosin as first line for pre-operative blockade. The choice of terazosin was based on the availability and low cost of the drug in the Philippines. The initial dose in our patients was 1 mg/day and the maximum dose was 4 mg/day which controlled the patients' blood pressures. Selective alpha blockers do not block the presynaptic alpha-2 receptors, thus norepinephrine release is not enhanced, preventing reflex tachycardia. They also have a shorter duration of action permitting a more rapid adjustment of dosage and reduced duration of postoperative hypotension.15 However, the use of these agents may lead to supersaturation of the alpha receptors, and these drugs can be displaced by high levels of endogenous catecholamines.7 This may lead to elevations in blood pressures. Despite that, the patients given terazosin did not suffer from blood pressure elevations while on the drug, which may be safely given as a pre-operative blockade for pheochromocytoma patients in the absence of phenoxybenzamine. Since terazosin is readily available in the Philippines, this could be an alternative treatment for the preoperative management of pheochromocytoma in the country.
One of our patients had diabetic ketoacidosis during admission. The elevation of glucose is due to the profound effect of elevated catecholamines on glucose tolerance. It also induces lipolysis, hepatic gluconeogenesis and inhibits peripheral glucose utilization. Elevated norepinephrine stimulates glycogenolysis, suppresses insulin secretion, and increases ketone production. Diabetic ketoacidosis is a rare complication of pheochromocytoma and has been reported in a few patients.16
Terazosin, a selective alpha-1 antagonist, at a maximum dose of 4 mg per day, may be safely given to Filipino patients diagnosed with pheochromocytoma as first line preoperative blockade. This may influence local guidelines in the country to consider terazosin as first line agent in the pre-operative management of pheochromocytoma.
1. Walther MM, Keiser HR, Linehan WM. Pheochromocytoma: Evaluation, diagnosis, and treatment. World J Urol. 1999;17(1):35-39. http://dx.doi.org/10.1007/s003450050102.
2. Hernandez FC, Sánchez M, Alvarez A, et al. A five-year report on experience in the detection of pheochromocytoma. Clin Biochem. 2000;33(8):649-655. http://dx.doi.org/10.1016/S0009-9120(00)00172-7.
3. Philippine General Hospital Census 2013. Unpublished data.
4. Eisenhofer G, Goldstein DS, Walther MM, et al. Biochemical diagnosis of pheochromocytoma: How to distinguish true- from false-positive test results. J Clin Endocrinol Metab. 2003;88(6):2656-2666. http://dx.doi.org/10.1210/jc.2002-030005.
5. Zelinka T, Štrauch B, Petrák O, et al. Increased blood pressure variability in pheochromocytoma compared to essential hypertension patients. J Hypertens. 2005;23(11):2033-2039.
6. Zapanti E, Ilias I. Pheochromocytoma: Physiopathologic implications and diagnostic evaluation. Ann N Y Acad Sci. 2006;1088:346-360. http://dx.doi.org/10.1196/annals.1366.022.
7. Prys-Roberts C. Phaeochromocytoma-recent progress in its management. Br J Anaesth. 2000;85(1):44-57. http://dx.doi.org/10.1093/bja/85.1.44.
8. Loh KC, Shlossberg AH, Abbott EC, Salisbury SR, Tan MH. Phaeochromocytoma: A ten-year survey. QJM. 1997;90(1):51-60. http://dx.doi.org/10.1093/qjmed/90.1.51.
9. Prys-Roberts C, Farndon JR. Efficacy and safety of doxazosin for perioperative management of patients with pheochromocytoma. World J Surg. 2002;26(8):1037-1042. http://dx.doi.org/ 10.1007/s00268-002-6667-z.
10. Weingarten TN, Cata JP, O'Hara JF, et al. Comparison of two preoperative medical management strategies for laparoscopic resection of pheochromocytoma. Urology. 2010;76(2):508-511.
11. Feit A, Cohen M, Dimino L, et al. The effects of labetalol and prazosin on exercise haemodynamics in hypertensive patients. J Hum Hypertens. 1991;5(1):39-43.
12. Kocak S, Aydintug S, Canakci N. Alpha blockade in preoperative preparation of patients with pheochromocytomas. Int Surg. 2002;87(3):191-194.
13. Agrawal R, Mishra SK, Bhatia E, et al. Prospective study to compare peri-operative hemodynamic alterations following preparation for pheochromocytoma surgery by phenoxybenzamine or prazosin. World J Surg. 2014;38(3):716-723. http://dx.doi.org/10.1007/s00268-013-2325-x.
14. Russell WJ, Metcalfe IR, Tonkin AL, Frewin DB. The preoperative management of phaeochromocytoma. Anaesth Intensive Care. 1998;26(2):196-200.
15. Tauzin-Fin P, Sesay M, Gosse P, Ballanger P. Effects of perioperative a1 block on haemodynamic control during laparoscopic surgery for phaeochromocytoma. Br J Anaesth. 2004;92(4):512-517. http://dx/doi.org/10.1093/bja/aeh083.
16. Douma S, Petidis K, Kartali N, Mahera K, Sabanis C, Zamboulis C. Pheochromocytoma presenting as diabetic ketoacidosis. J Diabetes Complications. 2008;22(4):295-296. http://dx.doi.org/10.1016/j.jdiacomp.2007.02.006.
Authors are required to accomplish, sign and submit scanned copies of the JAFES Declaration that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere.
Consent forms, as appropriate, have been secured for the publication of information about patients; otherwise, authors declared that all means have been exhausted for securing such consent.
The authors have signed disclosures that there are no financial or other relationships that might lead to a conflict of interest. All authors are required to submit Authorship Certifications that the manuscript has been read and approved by all authors, and that the requirements for authorship have been met by each author.