Pancreatic calcification is a well recognized cause of diabetes but development of primary hyperparathyroidism in the background of pancreatic and renal calcification and diabetes is uncommon. Solitary parathyroid adenomas are the commonest cause of primary hyperparathyroidism. Primary hyperparathyroidism classically presents with fractures, kidney stones, depression, hypertension and peptic ulcer disease, predominantly in females. The clinical presentation of primary hyperparathyroidism is changing and most cases are now picked up during evaluation of other conditions. We report a case of primary hyperparathyroidism who presented with gastrointestinal symptoms followed by multiorgan calcification, and then diabetes and finally, life threatening hypercalcaemia.
A 51-year-old female had recurrent episodes of vomiting with dehydration necessitating multiple (2 to 3 times every year) episodes of hospitalisation since 1988. She often became slightly symptomatic in between these episodes and was managed with oral antiemetics & proton pump inhibitors at home. No surgical cause could be identified. Initial investigations in 1988 revealed plasma glucose, calcium, phosphorus, liver function tests including serum albumin, serum amylase, lipase all within normal limits. Ultrasonography of pancreas, upper GI endoscopy and CT scan of abdomen were normal.
The patient developed diabetes in 1991, during the course of a hospital admission. Her serum amylase level was normal at 47 iu/l; sonography of the abdomen showed pancreatic calcification and a CT scan showed pancreatic calcification with dilated pancreatic duct, intraductal calculi and atrophic pancreas suggestive of chronic pancreatitis. From 1993 the intensity and frequency of episodic vomiting and pain abdomen increased, occurring every 3-4 months and relieved gradually over 3-4 days with intravenous fluids and conservative management.
In 2003 she was hospitalized with a urinary tract infection and was found to have hypertension and bilateral nephrolithiasis. At that time, her diabetes was poorly controlled (FPG: 230 mg/dl, PPPG: 245 mg / dl), normal renal profile (urea: 25 mg/dl, creatinine: 0.86 mg/dl) and normal serum calcium (9.12 mg /dl) and normal serum albumin. She was discharged with insulin.
In December 2004, she was admitted to hospital with similar symptoms along with severe hyperglycaemia (365 mg/dl). She was 156 cm in height, weighed 46 kg and her BMI was 18.9. She had no history of diabetes in both paternal and maternal sides of the family. She had two children and denied diabetes during her pregnancies. She delivered healthy babies and neither of them was more than 3.5kg (the boy was 2.8 kg and the girl was 3.3 kg) at the time of birth. Investigations revealed no ketone bodies in the urine, normal amylase (29 iu/l) and lipase 14 iu/l). There were multiple areas of calcification in the pancreas, spleen and kidneys on sonography. Her renal profile was normal (urea: 44 mg/dl, creatinine: 1.2 mg/dl) with severe hypercalcaemia (serum calcium: > 15 mg/dl ) and normal serum phosphorus (4.7 mg/dl) and albumin (4.0 gm/dl).
Hypercalcaemia was initially treated with intravenous saline and oral alendronate. Her calcium reduced to 9.4 mg/dl and phosphorus lowered to 0.6 mg/dl in the next 24 hours and stabilized at 10 mg/dl and 3.44 mg/dl respectively in 72 hours
Click here to download Table 1Table 1. Laboratory results.
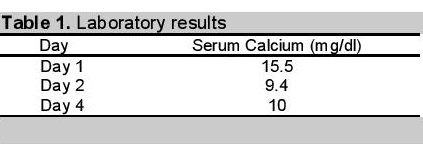
Her serum PTH level was high at 221.7 pg/ml (normal range: 11-79.5 pg/ml), obtained when serum calcium had normalized at 10.0 mg/dl. She underwent a parathyroid sestamibi scan which showed a right inferior parathyroid adenoma.
The patient underwent right inferior parathyroidectomy and histology confirmed a parathyroid adenoma. Following the surgery, her gastrointestinal symptoms disappeared but diabetes persisted and required insulin. Her serum calcium and phosphate levels were normal (Ca: 8.58 mg/dl & PO4: 3.54 mg/dl ) with oral calcium 1.5 gm daily and calcitriol 0.5 ug daily.
She was further evaluated for MEN 1, but no pituitary pathology was seen on CT scan. She has regularly followed up until March 2012 and required insulin treatment for control of the persistent hyperglycemic state.
Primary hyperparathyroidism (PHPT) has a variable clinical expression. The clinical profile of the disease in the Western hemisphere has changed from that described in the past but symptomatic PHPT is still the predominant form of the disease in many parts of the world, especially developing countries.1 In Indians, PHPT is a severe, symptomatic disorder with skeletal, muscular and renal manifestations at a younger age.2
Our patient first presented with gastrointestinal symptoms (1988), followed by pancreatic calcifications & diabetes (1991), nephrolithiasis (2003) and finally, life threatening hypercalcaemia (2004). Repeated serum calcium with albumin measurements were done and hypercalcaemia was never detected except on the last occasion. Prominent gastrointestinal symptoms along with progressive organ calcification are an uncommon presentation in an overwhelmingly classical PHPT.
Intermittent hypercalcaemia is a recognized biochemical finding of PHPT,3 a condition that requires sophisticated diagnostic tools (parathyroid venous sampling and bone densitometry) to identify the cause4 early in the disease. Intermittent hypercalcaemia may produce multiorgan calcification including the kidney5 before the development of symptomatic hypercalcaemia. Parathyroid adenomas may lead to pancreatic calcifications6 and PHPT leading to pancreatic calcifications that can give rise to diabetes.7
The increased prevalence of diabetes mellitus (DM) and glucose intolerance in primary hyperparathyroidism (PHPT) is established by many studies.8,9 The prevalence of diabetes mellitus in PHPT is approximately 8% and that of PHPT in diabetic patients is approximately 1%. Both values are about three-fold higher than the respective expected prevalences in general populations.10 In our case, diabetes and pancreatic calcification developed early (in 1991) and hypocalcaemia with PHPT discovered 13 years later (in 2004).
The response of parathyroid surgery on diabetes is variable: in some patients the diabetic condition improves or resolves;10 remains unaltered, or deteriorates.11 The diabetic state of our patient did not change following parathyroid surgery. The type of diabetes associated with PHPT is also variable: Type 1 or Type 2,10,13 or may be a secondary diabetes from pancreatic calcification.7 A diagnosis of chronic calcific pancreatitis (CCP) was established in this patient by evidence of characteristic abdominal pain; presence of diabetes mellitus and radiological evidence of pancreatic calculi.12
MEN 1 is characterized by the combined occurrence of tumors of the parathyroid, pancreatic islet cells and anterior pituitary. Parathyroid tumors occur in 95% of MEN 1 patients and the resulting hypercalcaemia is the first manifestation in about 90% of patients. Though no neoplastic changes were identified in the patient's pituitary or pancreas, close follow up is necessary to detect any future changes.
MEN 2 describes the association of medullary thyroid carcinoma, pheochromocytomas and parathyroid tumors. Medullary thyroid carcinoma is the most common component in MEN 2. The patient had no goitre and serum calcitonin level could not be measured because of the unavailability of this test in our institution
The prevalence of diabetes mellitus (DM) or glucose intolerance in PHPT and prevalence of primary hyperparathyroidism in diabetic patients are about three-fold higher than their respective expected prevalences in the general population. This middle-aged female, diabetic, developed multi-organ calcification and primary hyperparathyroidism and had parathyroidectomy. The cause of progressive multi-organ calcification before detection of hypercalcaemia is difficult to explain. However, intermittent hypercalcaemia may explain the progressive multiorgan calcification in primary hyperparathyroidism which repeatedly escaped detection before the development of symptomatic hypercalcaemia.
1. Bhansali A, Masoodi SR, Reddy KS et al. Primary hyperparathyroidism in North India: A description of 52 cases. Ann Saudi Med. 2005 ;25(1):29-35.
2. Mishra SK, Agarwal G, Kar DK, et al. Unique clinical characteristics of primary hyperparathyroidism in India. Br J Surg. 2001;88(5):708-14. http://dx.doi.org./10.1046/j.0007-1323.2001.01775.x
3. Broadus AE, Horst RL, Littledike ET et al. Primary hyperparathyroidism with intermittent hypercalcaemia: Serial observations and simple diagnosis by means of an oral calcium tolerance tests. Clin Endocrinol (Oxf). 1980;12(3):225-35. http://dx.doi.org/10.1111/j.1365-2265.1980.tb02704.x.
4. Barilla DE, Pak CY. Pitfalls in parathyroid evaluation in patients with calcium urolithiasis. Urol Res. 1979;7(3):177-82. http://dx.doi.org/10.1007/BF00257203.
5. Ljunghall S, Kallsen R, Backman U et al. Clinical effects of parathyroid surgery in normocalcaemic patients with recurrent renal stones. Acta Chir Scand. 1980;146(3):161-9.
6. Stone GR. Pancreas and parathyroid. Parathyroid adenoma in association with pancreatic calcification. J Kans Med Soc. 1962 Dec;63:519-21.
7. Kubota S, Yamada Y, Wakasugi H et al. An autopsy case of renal failure as its cause of death in a patient with primary hyperparathyroidism associated with chronic pancreatitis.Fukuoka Igaku Zasshi. 1996;87(10):226-8.
8. Taylor WH. The prevalence of diabetes mellitus in patients with hyperparathyroidism and among their relatives. Diabet Med 1991; 8(7): 683-687. http://dx.doi.org/ 10.1111/j.1464-5491.1991.tb01678.x.
9. Khaleeli AA, Johnson JN, Taylor WH. Prevalence of glucose intolerance in primary hyperparathyroidism and the benefit of parathyroidectomy. Diabetes Metab Res Rev. 2007;23(1):43-8. http://dx.doi.org/10.1002/dmrr.637.
10. Taylor WH, Khaleeli AA. Coincident diabetes mellitus and primary hyperparathyroidism. Diabetes Metab Res Rev. 2001 ;17(3):175-80. http://dx.doi.org/10.1002/dmrr.199.
11. Ljunghall S, Palmer M, Akerstrom G et al. Diabetes mellitus, glucose tolerance and insulin response to glucose in patients with primary hyperparathyroidism before and after parathyroidectomy. Eur J Clin Invest. 1983 ;13(5):373-7. http://dx.doi.org/ 10.1111/j.1365-2362.1983.tb00116.x.
12. Balaji LN, Tandon RK, Tandon BN, et al. Prevalence and clinical features of chronic pancreatitis in southern India. Int J Pancreatol. 1994 ;15(1):29-34.
Authors are required to accomplish, sign and submit scanned copies of the JAFES Declaration that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere.
Consent forms, as appropriate, have been secured for the publication of information about patients; otherwise, authors declared that all means have been exhausted for securing such consent.
The authors have signed disclosures that there are no financial or other relationships that might lead to a conflict of interest. All authors are required to submit Authorship Certifications that the manuscript has been read and approved by all authors, and that the requirements for authorship have been met by each author.