The mission of camps specialized for children and youth with diabetes is to facilitate a traditional camping experience in a medically safe environment. The camp setting is an ideal place for teaching diabetes self-management skills. Examples of educational topics tackled in the camp setting include: blood glucose monitoring, recognition and management of hypo-/hyperglycemia and ketosis, insulin types and administration techniques, carbohydrate counting, insulin dosage adjustment based on nutrition and activity schedules, the importance of diabetes control, healthy lifestyles issues, including integration of healthy eating, physical activity and relaxation, problem-solving skills for caring for diabetes at home versus camp, life skills for independent living, stress management and coping skills, sexual health and preconception issues, diabetes complications and new therapies including technologies.1
Just as important, diabetes camps allow children with diabetes to feel less isolated through interaction with other children afflicted with diabetes. It builds self-confidence and fosters independence. Learning is also facilitated through sharing of experience with their peers.
The aim of this paper is to examine the oral health of children attending a diabetes camp. Studies have shown diabetes to be a risk factor for periodontitis on the one hand and periodontitis has been shown to affect glycemic control and increase the risk for developing complications among diabetic patients.2 In spite of these findings, oral health is only beginning to receive much needed attention as an important aspect of general health in diabetic patients.
Project Oral Health for Juvenile Diabetics was organized in 1998 to provide free/discounted dental treatment to children with diabetes 19 years old and below. The mean number of decayed, missing, and filled teeth (DMFT) of the 11-15 age group in the Project Oral Health for Juvenile Diabetics (POHJD) population was 8.5 while the mean DMFT of the 12-year old age group in the 2006 National Oral Health Survey in the Philippines was 2.9.3,4 The two studies however, used different methods of investigation and therefore, comparisons must be made with caution.
The participants of POHJD have been under the care of a physician for an average of 6 years. In those 6 years, occasions would have arisen to allow the physician a glimpse of the oral problem. However, physicians are also aware of the financial difficulties of type 1 diabetic patients and are not strongly predisposed to recommend preventive or even dental treatment to their patients.5
In addition, a study of the periodontal health of POHJD participants found 34% of patients aged 19 and below have pockets greater than 3.5 mm. The youngest patient found with mild periodontitis (pockets 3.5-5.5 mm) was 13 while the youngest patient with moderate periodontitis (pockets > 5.5 mm) was 17.6
Type 1 diabetic patients are reluctant to seek dental treatment because of cost, fear, and the lack of dentists who are willing to treat diabetic patients.5 Medication is the prime concern of the patient and all other concerns have to wait in line until adequate funds become available. Dental insurance is not available in the Philippines and treatment is offered mostly by private practitioners.3 The development of clinical practice guidelines for the delivery of out-patient dental treatment is also needed in order to relieve the anxiety among dentists when treating diabetic patients.5
Study Design: Cross sectional Survey
Setting and Population: Attendees of the 2013 Camp Cope Summer Camp for Juvenile Diabetics.
Materials and Methods: Data regarding the patient's medical and dental history was obtained prior to dental examination. Dental examination was done inside a room with a plastic chair facing the sunlight. A flashlight was used to help examine the posterior teeth. The patients were examined for the presence dental caries and periodontal disease.
A simple count of the number of decayed, missing and filled teeth was performed and added to come up with the Decayed Missing and Filled Teeth index (DMFT).
Periodontal examination was performed using a Community Periodontal Index of Treatment Needs (CPITN) probe. Pocket probing was performed on six sites (mesiobuccal, mid-buccal, distobuccal, mesiolingual, mid-lingual and distolingual) on each tooth. The teeth were then scored on a scale of 0-4, which is similar to the CPITN method of the World Health Organization. A score of 0 indicated that no bleeding, calculus, or pockets greater than 3.5 mm was detected. A score of 1 indicated that bleeding was observed during pocket probing but not calculus or pockets greater than 3.5 mm. A score of 2 indicated the presence of calculus but not pockets greater than 3.5 mm. A score of 3 indicated the presence of 3.5 to 5.5 mm pockets. A score of 4 indicated pockets greater 5.5 mm.
During pre-camp orientation the families of the participants were informed that an oral examination will be performed as part of a survey to determine the oral health of the participants. The data and photos obtained for documentation will be presented in a study or a journal article. Data Analysis: The data were subjected to descriptive statistical analysis and compared with other factors such as age and number of years with diabetes.
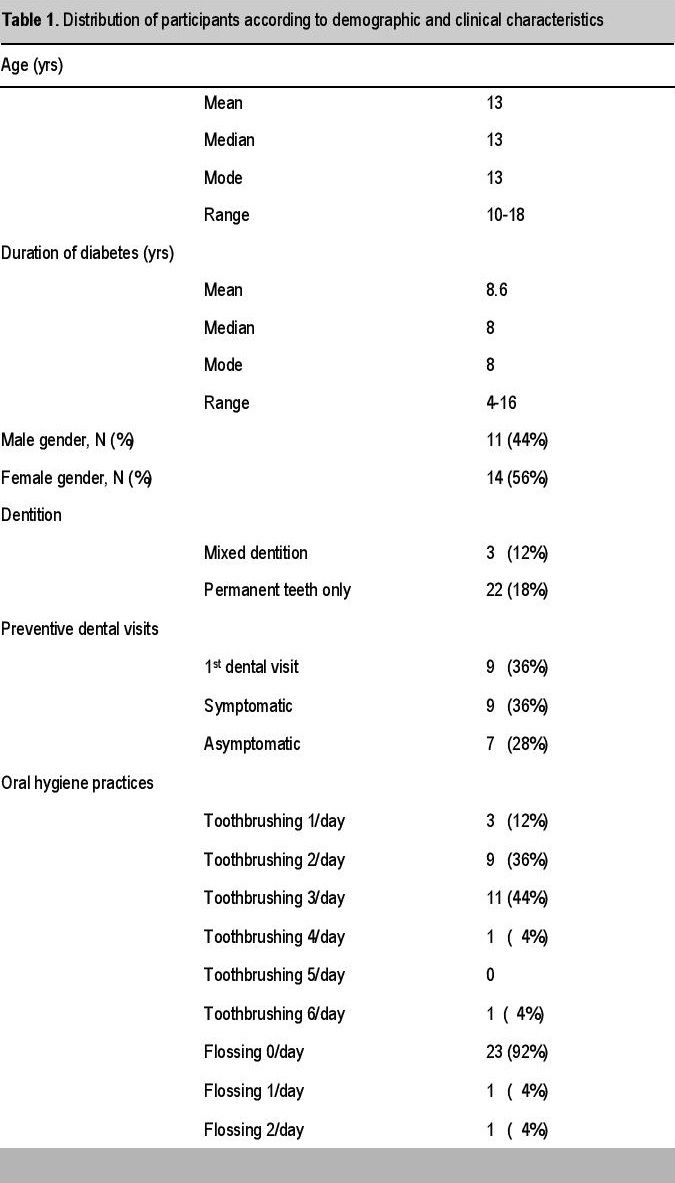
Patient profile. A total of 25 type 1 diabetic patients attended the camp. Of these, 14 (56%) were female while 11 (44%) were male. Mean age of the participants was 13 and a mean number of years with diabetes of 8.6. Three (12%) of the patients still had deciduous teeth. Nine (36%) had their first dental examination during the camp, while another 9 (36%) visited their dentist regularly twice a year. The rest, 7 (28%), went to their dentists only when they felt they had problems. Twenty two patients (88%) brushed their teeth at least twice a day and 23 (92%) did not use the dental floss (Table 1).
Click here to download Table 1Table 1. Distribution of participants according to demographic and clinical characteristics, N=25
Caries and Periodontal Disease Profile. The proportion of participants with dental caries was 72% (18) with a mean number of decayed, missing and filled teeth (DMFT) of 4.6. Five (20%) of the participants had a DMFT score of 0, meaning that they have no decayed missing or filled teeth while 10 (40%) either already had permanent teeth extracted or required tooth extraction for non-restorable, severely decayed permanent teeth. Only 4 (16%) had fillings or pit and fissure sealants, while 14 (56%) had a DMFT score derived mainly from the number of decayed teeth. Two (8%) had a DMFT score equivalent to the sum of the number of decayed and missing teeth. Periodontitis (pockets >3.5 mm; CPITN = 4) was found in only 1 (4%) patient. Twenty one (84%) of the participants either had a CPITN score of 1 or 2, meaning bleeding upon probing or calcular deposits were observed. 3 (12%) had a CPITN score of 0.
The DMFT scores of the participants showed a high of 16 and a low score of 0, indicating the diverse oral health conditions of the participants. Two (8%) participants have DMFT scores composed only of filled teeth, indicating a high level of concern for the preservation of teeth while 14 (56%) had a DMFT score composed only of decayed teeth indicating the opposite.
The high number of participants 10 (40%) who required tooth extraction or already had permanent teeth extracted, however, tilts the balance towards a low level of importance attached to oral health among these participants. This is further evidenced by the number of participants 9 (36%) who had their first dental examination during the camp. This subpopulation had a mean age of 12.9 and had received treatment for diabetes for 7.9 years. This shows a lack of concern for oral health among physician managing children with diabetes. Given the number of concepts that patients are encouraged to learn about their diabetes, this is not surprising. However, the possibility that severely decayed teeth can lead to infection that can trigger hyperglycemia or even diabetic keto-acidosis, should oblige the physician to include oral health as a major component of glycemic control.
When oral diseases like tooth decay or periodontal disease affect the anterior teeth, it can result in poor appearance, poor social interaction, unwanted attention, and even ridicule (Figures 1-3). This can further add to the isolation most type 1 diabetic patients encounter during the first few years of the disease. The combination of early onset diabetes and poor oral health can lead to delayed educational development in younger patients and inability to compete for jobs among older patients. High self-esteem was found to relate to good adherence with exercise regimens and adjustment of insulin doses in type 1 diabetics.7 Optimum oral health removes additional obstacles that can further impair a young diabetic from overcoming the challenges of her disease.
Click here to download Figure 1Figure 1.Early loss of anterior teeth secondary to dental caries.

Click here to download Figure 2
Figure 2.Caries on the interproximal areas.

Click here to download Figure 3
Figure 3.Periodontitis with heavy calcular deposits that extends to the subgingival area with Inflamed gingiva that easily bleeds.

Limitations
The lack of adequate lighting, a comfortable chair and radiographs during the dental examination could have underestimated detection of the number of caries and periodontal lesions.
Diabetes camps are a good place to screen oral health problems among type 1 diabetic patients given the different socio-economic factors, levels of concern for oral health and availability of dental care providers among families of with type 1 diabetic children. Physicians managing type 1 diabetics should motivate their patients to see the dentist twice a year for preventive visits and strongly encourage them to have dental treatment when dental diseases are present. An oral exam should be part of the cursory examination performed by physicians handling these patients.
AcknowledgementsI would like to thank Dr. Augusto Litonjua of Camp Cope for inviting me to participate and for showing tremendous concern for the oral health of their campers. Thanks too, to Dr. Jaime Aragon, Dr. Carol Narvacan-Montano and Ms. Louella Therese Babasanta for facilitating the oral examination of the campers and for Mrs. Linda for providing the logistics for the oral health program at camp.
1. American Diabetes Association. Diabetes management at camps for children with diabetes. Diabetes Care. 2012;35(Suppl. 1):S72-S75. http://dx.doi.org/10.2337/dc12-5072.
2. Taylor JJ, Preshaw PM, Lalla E. A review of the evidence for pathogenic mechanisms that may link periodontitis and diabetes. J Clin Periodontol. 2013; 40 (Suppl. 14): S113-S134. http://dx.doi.org/10.1111/jcpe.12059. 3. Ofilada EJL, Oliveros-Villarico M. Caries experience of insulin-dependent diabetic patients in the Philippines. St. Luke's Journal of Medicine. 2012;8 (1):11-16. 4. Monse B and Yanga-Mabunga S. Urgent oral health needs for Filipino children - The results of the National Oral Health 2006. Developing Dentistry. 2007;8:7-9. 5. Ofilada EJL, Jimeno CA. A survey on the barriers to dental care among individuals with type 1 diabetes. PJIM. 2013;51(2):1-6. 6. Ofilada EJL. Periodontal health of type 1 diabetic patients in the Philippines. St. Luke's Journal of Medicine. 2012; 8(2):33-38. 7. Kneckt MC, Keinänen-Kiukaanniemi SM, Knuuttila MLE, Syrjälä AM. Self-esteem as a characteristic of adherence to diabetes and dental self-care regimens. J Clin Periodontol. 2001; 28(2):175-180. http://dx.doi.org/10.1034/j.1600-051x.2001.028002175.x.Authors are required to accomplish, sign and submit scanned copies of the JAFES Declaration that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere.
Consent forms, as appropriate, have been secured for the publication of information about patients; otherwise, authors declared that all means have been exhausted for securing such consent.
The authors have signed disclosures that there are no financial or other relationships that might lead to a conflict of interest. All authors are required to submit Authorship Certifications that the manuscript has been read and approved by all authors, and that the requirements for authorship have been met by each author.