Osteoporosis is a systemic skeletal disease characterized by low bone mass and microarchitectural deterioration of bone tissue, with a consequence increase in bone fragility and susceptibility to fracture. In 2001, the National Institute of Health (NIH) proposed anew definition for osteoporosis as a systemic skeletal disease characterized by compromised bone strength result in increase susceptibility to fracture.1
The problem of osteoporosis will increase in developing countries, including Indonesia, with increased life expectancies and increased proportion of aged population. Data from survey in 1990 showed that proportion of population with age of 55 or more was 9.2%, which is increased 50% compared to data from the survey of 1971.2The Indonesian Guideline of Osteoporosis was developed to increase awareness of specialists, general practitioners and patients, about the detection and management of osteoporosis in Indonesia. Both the healthcare professionals and the patients can choose the optimal investigation and treatment options for the disease.
The Guidelines was developed by Indonesian Osteoporosis Association (Perhimpunan Osteoporosis Indonesia, PEROSI) and was officially launched during The 6th Annual National Scientific Meeting of PEROSI in Malang, Indonesia at October 15, 2010.
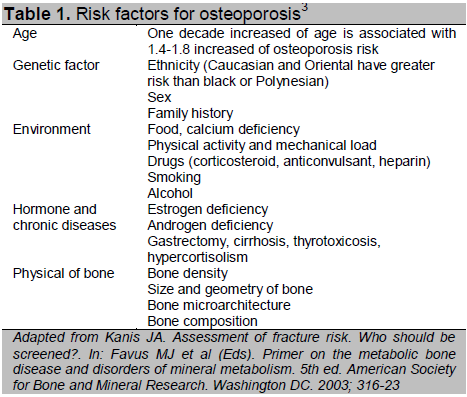
Several conditions will increase the risk for osteoporosis. Risk factor evaluation is an important step in identifying patient with osteoporosis. (Table 1)
Risks for osteoporotic fracture are mainly determined by age and bone density. Other risk factors for osteoporotic fractures vary in different ages including risk of fall, vision problems, immobilization, sedative drugs and calcium intake.3,4
Click here to download Table 1
Table 1. Risk factors for osteoporosis3
Clinical evaluation for patient with osteoporosis is aimed to identify risk factors, including life styles. History taking should include these points :
1. History of minimally traumatic fracture, decreased body height, increased kyphosis of the spine.
2. Chronic diseases that may increase risk for osteoporosis including endocrine disorders, renal diseases, liver diseases, vitamin D deficiency, hematologic diseases, gastrointestinal disease, neurologic diseases and rheumatic diseases.
3. History of drugs consumption (corticosteroid, anti-epileptic drug, cyclosporine, lithium, etc.).
4. Menstrual period (menarche, menopause, pregnancy).
5. Nutrition, including calcium intake.
6. Lifestyles (smoking, alcoholism, physical exercise).
7. Risk of fall.
8. History of breast tumor, malignancy, and vascular diseases that may be important in considering treatment option.
Physical examinations for patient with osteoporosis include height and weight. Other examinations include gait, bone deformities, leg-length inequality, spinal tenderness, and thyroid glands. Blue sclera are found in patients with osteogenesis imperfect, associated with deafness, ligament hyperlaxity, joint hypermobility, and teeth abnormalities. In rickets, physical examination shows short stature, bone pain, craniotabes, costo-chondral joint prominence, and bowing deformity of long-bone. Patients with hypocalcemia may present with tetany. Band keratopathy, which results from calcium phosphate deposition in the cornea, may be found in patients with primary hyperparathyroidism.5
Indication for bone biochemical markers measurement is to identify patient with osteoporosis risk, rapid bone loss, predict femoral fracture risk, to monitor patient with long-term steroid treatment, to evaluate treatment responses and study the pathogenesis of osteoporosis. Treatment with anti-resorptive agents will rapidly decrease bone remodeling, thus it can be detected using bone marker tests.
Bone formation markers include serum alkaline phosphatase, osteocalcin, procollagen-1-peptides, p1-carboxyterminal propeptide, and p1-N-terminal propeptide. Bone resorption markers include urinary hydroxyproline, pyridinoline, deoxypyridinoline, and collagen-1-N-terminal telopeptide. Several conditions should be considered in interpreting results of bone markers, such as renal function, circadian rhythm, age and other diseases.6,7
Patients with osteoporosis should have a radiographic examination of the thoraco-lumbar spine to identify the present of spinal fracture. However, plain radiographic examinations cannot detect early osteoporosis. Radiographic examinations have an important role in excluding other conditions such as bone metastasis, spondylitis, degenerative process, or primary malignancy on bone.2
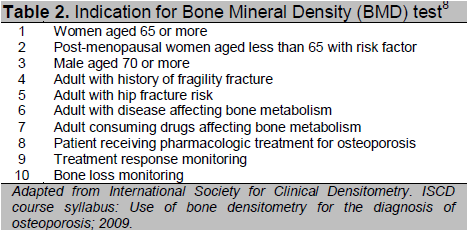
Bone density test using dual energy x-ray absorptiometry (DXA) method is the standard test and widely used to measure the bone mineral density (BMD). This technique can be used to measure axial, peripheral and total body bone density. Indications for bone density test are to confirm diagnosis of osteoporosis, to calculate fracture risk and monitor treatment8 (Table 2).
Click here to download Table2
Table 2. Indication for Bone Minderal Density (BMD) test8
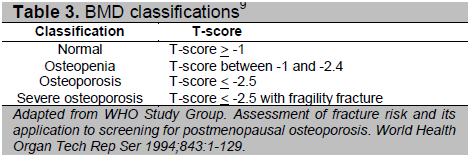
Results from BMD test using DXA technique are area bone density (gram/cm2), T-score, and Z-score. T-score is the number of standard deviations by which the patient’s BMD differs from the mean peak BMD for young normal subjects of the same gender. Z-score is the number of standard deviations by which the patient’s BMD differs from the mean BMD for subjects of the same age. The World Health Organization (WHO) classifies the BMD based on the T-scores8 (Table 3).
Click here to download Table 3
Table 3. BMD classifications9
Fracture risk can be calculated using formula WHO FRAX Tool from the website www.shef.ac.uk/FRAX.
Regular physical exercise to maintain strength, flexibility and coordination of neuromuscular system may prevent falling.. Adequate calcium and vitamin D intake, smoking and alcohol cessation should be advised for all patients with osteoporosis. Patient also should be informed regarding other diseases and drugs that may increase risk of osteoporosis. Patients who need long-term corticosteroid therapy should be treated with the lowest acceptable dose and should be discontinued as soon as possible. Patient with chronic inflammatory disease such as rheumatoid arthritis should be adequately treated to control the disease process.2
1. Antiresorptive agentBisphosphonate
Bisphosphonates inhibit the action of osteoclasts. These drugs should be administered on an empty stomach, with 2 glasses of plain water, and patient should keep upright for at least 30 minutes to improve absorption and prevent reflux esophagitis. Bisphosphonate agents for osteoporosis treatment are risedronate (orally 5 mg/day or 35 mg/week or 150 mg/month), alendronate (orally 10 mg/day or 70 mg/week), ibandronate (orally 2.5 mg/day or 150 mg/month or intravenously 3 mg/3 months), and zoledronate (intravenously 5 mg/year).2,10
2. Raloxifene
Raloxifene inhibits osteoclast differentiation through selective estrogen receptor modulator (SERM) action. It does not stimulate estrogen receptors in the endometrium and breast. Recommended dose for osteoporosis treatment is 60 mg/day.2
3. Hormonal replacement therapy
a. Post-menopausal women: conjugated estrogen 0.3125 – 1.25 mg/day in combination with
medroxyprogesterone acetate 2.5 – 10 mg/day continuously. Mammography should be done
before the treatment is started then re-ordered every year. Physicians should be aware of the findings of The Women’s Health Initiative study of 2002, which reported potential side-effects of hormonal treatments.
b. Pre-menopausal women: conjugated estrogen is given on day 1 to 25 of the menstrual cycle, andmedroxyprogesterone on day 15 to 25, then both drugs stopped from day 26 to 28.
c. Male: testosterone treatment is considered in male with testosterone deficiency.
4. Calcitonin
Calcitonin is indicated for conditions with increased bone resorption and hypercalcemia such as Paget’s disease, osteoporosis and hypercalcemia of malignancy. Calcitonin decreases vertebral fracture risk, but not non-verebral fracture. Subcutaneous calcitonin effectively decreases pain in spinal fracture. Recommended dose is 200 IU/day intranasal.
5. Strontium ranelate
Strontium ranelate is an anti-osteporosis drug with dual effects by increasing osteoblast action and inhibiting osteoclast action. Recommended dose of strontium ranelate is 2 gram/day dissolved in water and taken at night 2 hours before or after meal.
6. Vitamin D
Vitamin D plays an important role in calcium absorption in gastrointestinal tract. More than 90% of vitamin D is synthesized within the body from its precursor in the skin by ultraviolet light. In the elderly, activation of vitamin D in the skin is decreased, and results in increased frequency of vitamin D deficiency in elderly.
7. Calcium
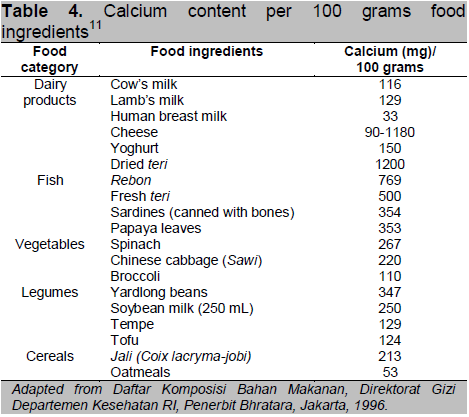
Recommended daily calcium intake is 1200 mg. Calcium carbonate containing elemental calcium 400 mg/gram is preferred. Other calciums such as calcium phosphate, calcium citrate, calcium lactate and calcium gluconate contain lower elemental calcium i.e., 230 mg/gram, 211 mg/gram, 130 mg/gram and 90 mg/gram, respectively. (Table 4)
8. Phytoestrogens
Phytoestreogens are derived from plants with similar chemical structure to 17β-estradiol and showing estrogenic effect. There are four groups of phytoestrogens including flavonoids, lignans, coumestans, and stilben.Isoflavon (mainly genistein and daidzein) is a subgroup of flavonoid, already investigated for treatment of osteoporosis. Effective dose of isoflavon is 20-80 mg/day.12
Click here to download Table 4
Table 4. Calcium content per 100 grams food ingredients11
Surgical treatment is indicated in patient with fracture, mainly hip fracture. In elderly with hip fracture, surgical treatment should be planned immediately in order to prevent long-term immobilization and further complications. Patient should also be treated with calcium and anti-osteoporosis agent after the operation.2
BMD re-examination at1 to 2 year intervals can be done to evaluate treatment responses in patient with osteoporosis. If the BMD can be maintained or remains stable in one yea, the treatment is successful and the bone resorption activity is suppressed. Bone metabolism markers can also be used to evaluate treatment responses, and can detect the changes earlier, within 3-4 months.2
Osteoporosis can be prevented with careful assessment of the risk factors. Since the management of osteoporosis requires high cost and long-term monitoring, it is recommended that early detection and prevention especially among high risk population.
1. NIH consensus development panel on osteoporosis prevention and therapy. Osteoporosis prevention, diagnosis and therapy. JAMA 2001;285:785-95.
2. Setyohadi Bea. Panduan Diagnosis dan Penatalaksanaan Osteoporosis. 2010:1.
3. Kanis J. Assessment of fracture risk. Who should be screened? In: al FMe, ed. Primer on the metabolic bone disease and disorders of mineral metabolism. 5th ed. Washington DC: American Society for Bone and Mineral Research; 2003:316-23.
4. Kanis J, Borgstrom F, De Laet C et al. Assessment of fracture risk. Osteoporosis Int 2005;16:581-9.
5. Siklarin P, Shoback DM, Langman CB. History and physical examination of osteoporosis. In: al FMe, ed. Primer on the metabolic bone disease and disorders of mineral metabolism. 5th ed. Washington DC: American Society for Bone and Mineral Research; 2003:143-4.
6. Looker A, Bauer DC, Chesnut CH III, et al. . Clinical use of biochemical markers of bone remodelling: Current status and future direction. Osteoporosis Int 2000;11:467-80.
7. Delmas Pea. Expert committee of the committee of scientific advisors of the International Osteoporosis Foundation for the use of bone markers in postmenopausal osteoporosis. Osteoporosis Int 2000;Suppl 6:S2-17.
8. International Society for Clinical Densitometry. ISCD course syllabus: Use of bone densitometry for the diagnosis of osteoporosis; 2009.
9. WHO Study Group. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. World Health Organ Tech Rep Ser 1994;843:1-129.
10. Black D, Rosen, CJ. Biphosphonates for the Prevention and Treatment of Osteoporosis. In: MJ F, ed. Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism Washington D.C.: American Society for the Bone and Mineral Research; 200.
11. Direktorat Gizi Departemen Kesehatan RI. Daftar Komposisi Bahan Makanan: Bhratara; 1996.
12. Meunier P. Osteoporosis: Diagnosis and management. 1st ed. London: Mosby; 1998.
Authors are required to accomplish, sign and submit scanned copies of the JAFES Declaration that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere.
Consent forms, as appropriate, have been secured for the publication of information about patients; otherwise, authors declared that all means have been exhausted for securing such consent.
The authors have signed disclosures that there are no financial or other relationships that might lead to a conflict of interest. All authors are required to submit Authorship Certifications that the manuscript has been read and approved by all authors, and that the requirements for authorship have been met by each author.