Thyroidectomy has become a standard of care in the management of different thyroid diseases, most importantly, of thyroid malignancies. It is straightforward and associated with minimal morbidity, as the surgical technique has evolved throughout the years. And with this, hospital stay for post-thyroidectomy patients has decreased significantly. Some surgeons even advocate “short-stay thyroid surgery,” defined as <24 hour hospital stay. The benefits include reduced costs, reduced in-patient waiting lists, increased availability of in-patient beds, reduced post-operative complications and the psychological benefit of avoiding prolonged hospitalization.1 However, as with any surgical procedure, it is not without complications. And these complications are barriers to early discharge and may cause significant morbidity to the patients. The different complications related to thyroid surgery include the following: hypocalcemia, bleeding and hematoma formation, recurrent laryngeal nerve injury, superior laryngeal nerve injury, dysphagia, wound infection, poor wound healing, inability to urinate and pain.2
In this study, we focused on the most common complication of thyroid surgery – hypocalcemia. It can occur transiently in up to 30%, and permanently in up to 4% of patients after thyroid surgery.3 It is a common hindrance for early discharge and may cause significant morbidity and fatality (due to cardiac arrhythmia) if not addressed promptly.
Post-thyroidectomy hypocalcemia may be symptomatic or asymptomatic (biochemical). Manifestations of hypocalcemia include perioral numbness, paresthesia of hands/feet, Chvostek’s sign, Trousseau sign, cramps, carpopedal spasms and tetany.
Several studies have enumerated factors that are associated with increased risk of hypocalcemia in patients who underwent thyroidectomy and these include: iatrogenic surgical trauma to the parathyroid glands, incidental parathyroidectomy, the number of functioning glands left behind, extent of surgery, experience of the surgeon, hyperthyroidism, retrosternal goiter, concomitant neck dissection, and thyroid carcinoma.4,5 Even the patient’s age has been found to be negatively correlated with post-operative serum calcium levels6 in one study but protective in another.7 On the other hand, prophylactic calcium or vitamin D supplementation has been shown to decrease the incidence of post-thyroidectomy hypocalcemia as seen in a meta-analysis,8 although there is currently no guideline on this. The extent of thyroidectomy and the thyroid disease are also correlated with risk of hypocalcemia in one study. Patients who underwent total thyroidectomy were found to be more likely to develop hypocalcaemia than those patients who had a completion thyroidectomy. The authors surmised that the two-stage procedure (completion thyroidectomy) resulted in a lower incidence of hypocalcaemia since the parathyroid glands on the side of the previous lobectomy may have had time to recover their function prior to the completion surgery. The authors also noted that thyroidectomy of toxic goiters tend to be more bloody, requiring more diathermy to be used for hemostasis which may compromise the vasculature of the parathyroid glands leading to a higher risk of hypocalcemia post-operatively.9
Thyroid gland weight may also be associated with this complication as seen in 2 studies where gland weight of >100-110 grams was associated with higher rates of post-thyroidectomy hypoparathyroidism.10,11 In a local retrospective study by Celzo, et al in 2005 where they studied 363 patients who underwent different types of thyroidectomy, they found that bilateral operation (thyroidectomy) [p <0.05, OR 4.56 (95% CI: 2.12-9.80)] and age <40 years old [p <0.05, OR 1.04 (95% CI: 1.02-1.07)] were independent predictors of post-thyroidectomy hypocalcemia.12
Several laboratory tests have also been used to predict those who will develop hypocalcemia after thyroidectomy. The use of intact parathyroid hormone level (i-PTH) has been studied thoroughly, and in one study was found to be an early predictor of hypocalcemia.13 Although there are several evidences for the use of i-PTH in predicting hypocalcemia, its availability and cost are its main limitation for widespread use. In our setting, i-PTH results cannot be made available immediately post-thyroidectomy, making it a retrospective index losing its predictive value. Other laboratory tests have also been studied as predictors of hypocalcemia and include: the relative drop in calcium level (baseline/pre-operative versus post-operative levels) defined as ≥1.1 mg/dl drop (the authors proposed a protocol of calcium replacement if this change in serum calcium is noted),14 and the absolute level of ionized or total calcium.4 One study was able to show that serum calcium levels measured at 6-h post-surgery and on day 1 postoperatively are useful in predicting whether the patient will develop hypocalcaemia. Day 1 postoperative calcium level and the slope may differentiate whether the patient will have a temporary or permanent hypocalcaemia.9
But despite all the available data, hypocalcemia is still the most common complication post-thyroidectomy. And with its attendant morbidity and possible mortality, it is a significant barrier to early discharge after thyroid surgery. Hence, there is still need to define this group of patients in order to predict those who will develop this complication post-thyroidectomy. And as one study was able to show, ethnicity may also influence the risk for this complication.7
Study Objectives
The general objective of this study was to determine the incidence and risk factors of post-thyroidectomy hypocalcemia.
Specifically, this study aimed:
- To determine the overall incidence of post-thyroidectomy hypocalcemia and the incidences of the following types of hypocalcemia: symptomatic and asymptomatic;
- To determine patient-related factors (age, gender, type of thyroid disease [toxic, non-toxic, malignant], thyroid gland weight and post-operative serum ionized calcium) and surgery-related factors (extent of thyroidectomy, performance of neck dissection, type of surgeon, duration of surgery, inadvertent parathyroidectomy, concomitant thyroidectomy complications) associated with post-thyroidectomy hypocalcemia;
- To determine mean time of onset (hours) of symptoms and the frequencies of the different hypocalcemic symptoms among patients with symptomatic post-thyroidectomy hypocalcemia;
- To determine the incidence of patients with manifestations of hypocalcemia post-thyroidectomy but with normal serum ionized calcium level and the mean time of onset (hours) and frequencies of the different symptoms.
Study Design and Subjects
This was a 4-year (2011-2014) retrospective study utilizing chart review of adult Filipino patients who underwent thyroidectomy (total or completion) at St. Luke’s Medical Center Quezon City, Philippines.
Inclusion Criteria
- Adult (≥18 years old), Filipino
- Admitted under or referred to the Section of Endocrinology, Diabetes and Metabolism of St. Luke’s Medical Center, Quezon City, Philippines
- Underwent total or completion thyroidectomy
Exclusion Criteria
- Known and/or with previous history of parathyroid disease
- Abnormal serum creatinine and/or presence of medical renal disease
- With known osteopenia/osteoporosis, any metabolic bone disease and/or active malignancy (except thyroid malignancy)
- On any of the following medications:
- Calcium
- Vitamin D
- Anti-resorptive (bone) drugs
- Menopausal hormone replacement therapy
- Thiazide diuretic
- Anti-epileptic agents
- Patients not monitored with calcium assay
Sample Size Calculation
Assuming that the incidence of post-thyroidectomy hypocalcemia is 30% (Mcleod IK, et al, 2006)3 with maximum allowable error of 5% and reliability of 90%, sample size required was 226 patients.
Data Collection
The annual “Thyroid Cases” censuses from 2011-2014 of the Section of Endocrinology, Diabetes and Metabolism of St. Luke’s Medical Center Quezon City were retrieved. The hospital personal identification numbers (PIN) who underwent total and completion thyroidectomy were submitted to the Medical Records Section of St. Luke’s Medical Center for chart retrieval. Data were gathered through chart review and use of St. Luke’s Medical Center Health Care System Version 1.8.1, using a data sheet. Data collected included the following: age, gender, type of thyroid disease (toxic goiter, non-toxic goiter, malignancy), thyroid gland weight by final histopathology report (grams), post-operative serum ionized calcium level (mmol/L), presence of hoarseness and/or hematoma post-operatively, extent of thyroidectomy (total or completion), performance of any neck dissection, duration of surgery (hours), type of surgeon (trainee or consultant), inadvertent parathyroidectomy based on presence of parathyroid tissue on final histopathology report, onset of hypocalcemia post-operatively (hours) and presence of hypocalcemic symptoms (perioral numbness, acral paresthesia, Chvostek’s sign, Trousseau’s sign, cramps, carpopedal spasms, tetany). Other pertinent data that were reviewed included the following: patient’s present and past medical history that may affect calcium balance, medication history and serum creatinine.
Definition of Terms
- Hypocalcemic - serum ionized calcium of: <1.00 mmol/L with or without any of the following: perioral numbness, acral paresthesia, Chvostek’s sign (new-onset), Trousseau’s sign, cramps, carpopedal spasms, tetany.
- Types
- Symptomatic hypocalcemia – serum ionized calcium of <1.00 mmol/L with any of the following: perioral numbness, acral paresthesia, Chvostek’s sign, Trousseau sign, cramps, carpopedal spasms, tetany (onset should be post-thyroidectomy).
- Asymptomatic hypocalcemia – serum ionized calcium of <1.00 mmol/L without any hypocalcemic symptom/sign as enumerated above.
- Normocalcemic – serum ionized calcium of 1.00-1.30 mmol/L and no symptom/sign of hypocalcemia.
- Total Thyroidectomy – removal of the entire thyroid gland; also includes “near-total thyroidectomy” which means a small amount of thyroid tissue is left behind around important structures that may otherwise be injured.
- Completion Thyroidectomy – removal of the remaining thyroid tissue after a previous partial thyroidectomy (i.e. lobectomy).
Statistical Analysis
Data analysis was performed using IBM SPSS Statistics Program Version 20. Quantitative variables were summarized as mean and standard deviation, while qualitative variables were tabulated as frequency and percentage. Factors associated with post-thyroidectomy hypocalcemia were determined using multiple logistic regression analysis. The level of significance was set at 5%.
Ethical Considerations
The clinical protocol and all relevant documents were reviewed and approved by the Institutional Scientific Review Committee and Institutional Ethics Review Committee of St. Luke’s Medical Center, Quezon City. Patient confidentiality was respected by ensuring anonymity of patient records. All study data were recorded and investigators were responsible for the integrity of the data i.e., accuracy, completeness, legibility, etc. The manner of disseminating and communicating the study results guaranteed the protection of the confidentiality of the patient’s data.
Among the 344 patients who underwent either total or completion thyroidectomy at St. Luke’s Medical Center, Quezon City, Philippines during the study period, 242 were included in the study (Figure 1).
Click here to download Figure 1Figure 1. Distribution of subjects according to incidence of hypocalcemia N=242
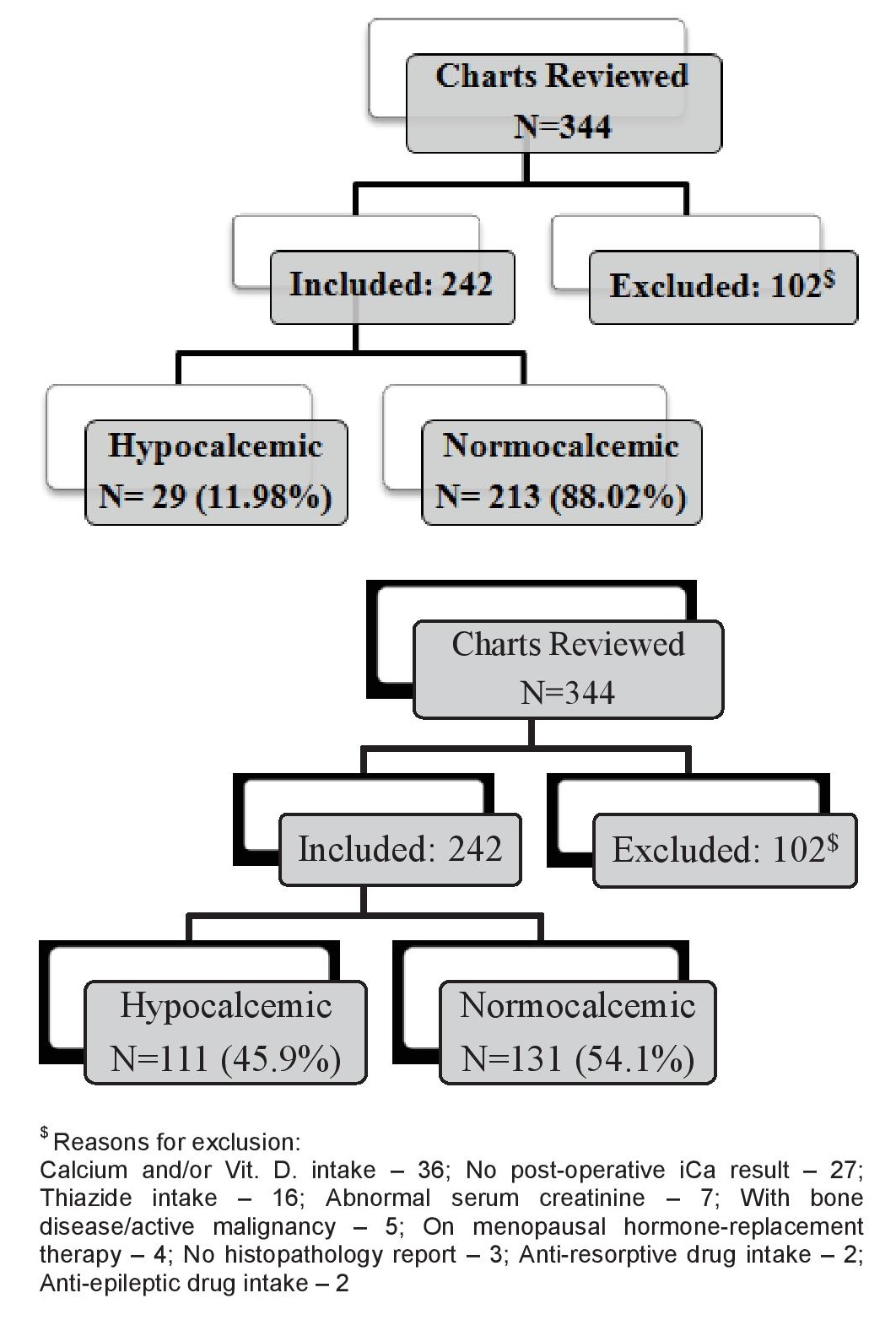
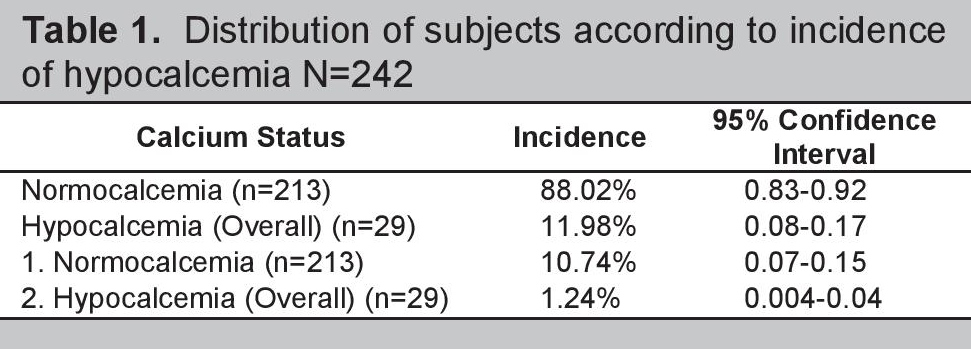
Hypocalcemia developed in 29 patients with an overall incidence of post-thyroidectomy hypocalcemia of 11.98% (95%CI: 0.08-0.17). Among the hypocalcemic patients, 26 were symptomatic (10.74%) while the remaining 3 were asymptomatic (1.24%) (Table 1).
Click here to download Table 1Table 1. Study population.
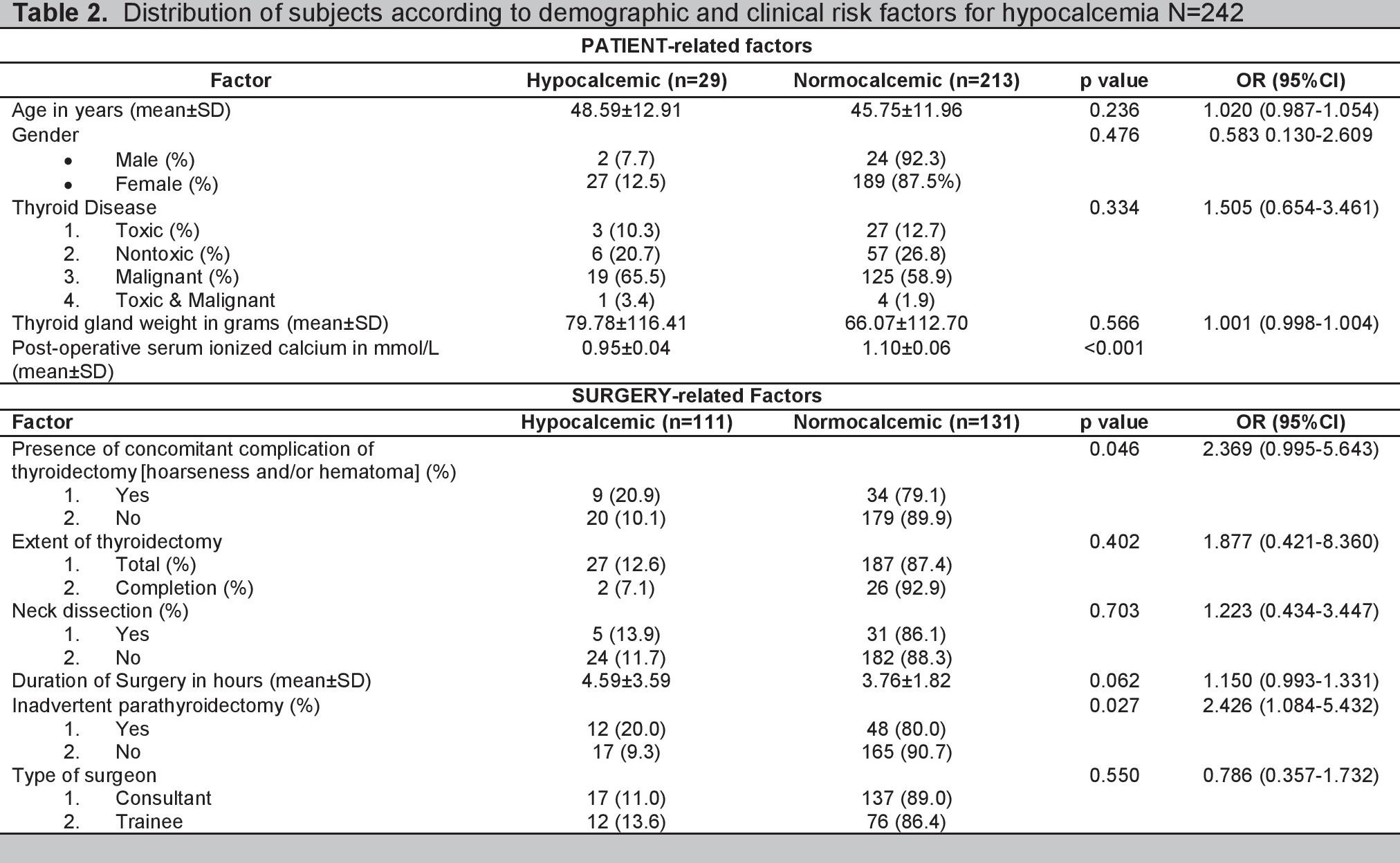
In the univariate analysis, the other patient-related factors were not significantly associated with hypocalcemia (age, gender, thyroid disease and thyroid gland weight). However, we can see that hypocalcemia occurred more often among females (12.5%) than males (7.7%) and that the mean thyroid gland weight is heavier in absolute terms in the hypocalcemic group (79.78 vs 66.07 grams).
As for the surgery-related factors, the presence of concomitant complication of thyroidectomy (hoarseness and/or hematoma) and inadvertent parathyroidectomy were found to be significantly associated with the outcome [p=0.046, OR 2.369 (95% CI: 0.995-5.643)] and p=0.027, OR 2.426 (95% CI: 1.084-5.432), respectively]. Extent of thyroidectomy and performance of neck dissection were not significantly associated with hypocalcemia; there was longer duration of surgery in the hypocalcemic group but this did not reach statistical significance. The status of the surgeon, as consultant or as trainee, was not significantly associated with hypocalcemia (Table 2).
Click here to download Table 2Table 2. Distribution of subjects according to demographic and clinical risk factors for hypocalcemia N=242
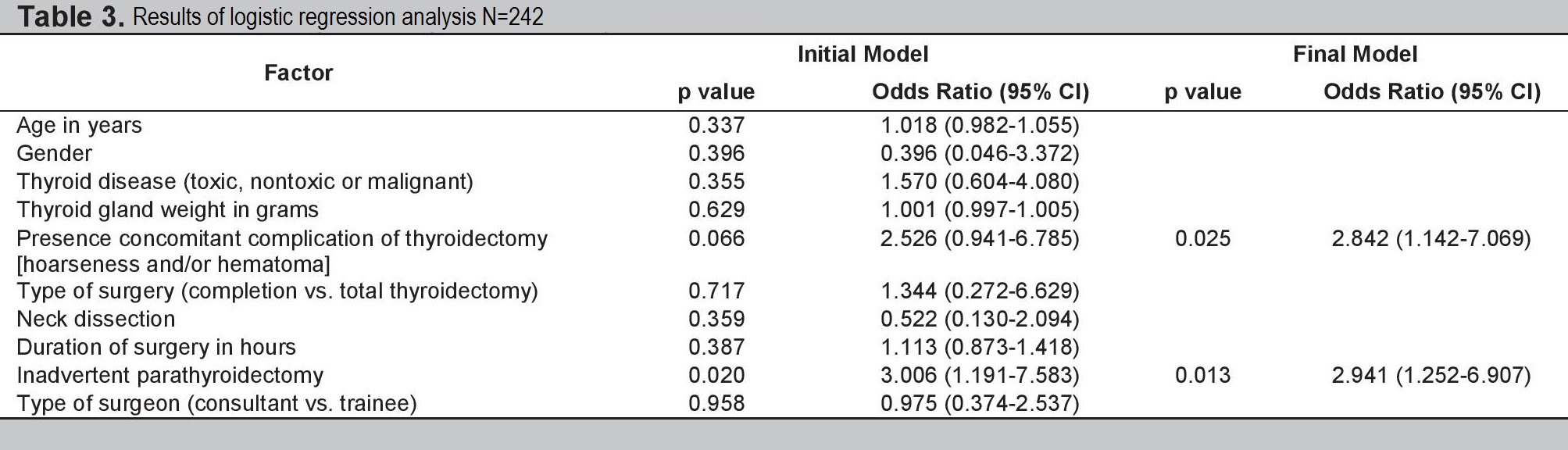
When all the factors were entered into multiple logistic regression analysis, we can see that in both the initial and final models, the presence of concomitant complication of thyroidectomy and inadvertent parathyroidectomy were significantly associated with hypocalcemia with p values of <0.05 and odds ratio of 2.842 (95%CI: 1.142-7.069) and 2.941 (95%CI: 1.252-6.907) respectively (Table 3).
Click here to download Table 3Table 3. Results of Logistic Regression Analysis N=242
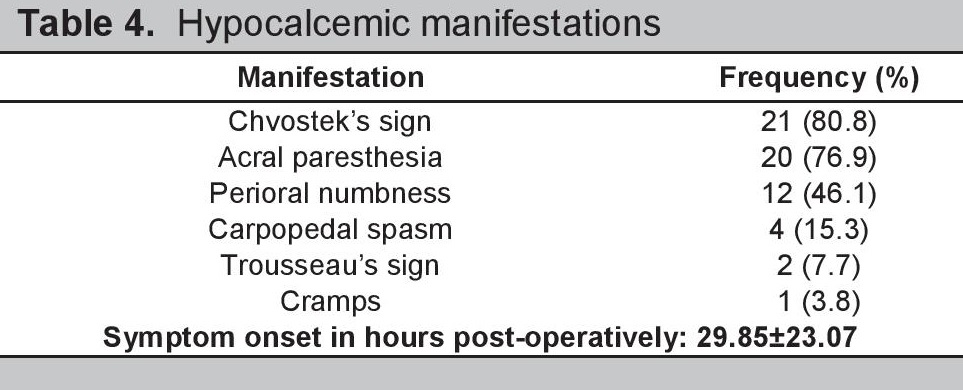
The onset of manifestations of post-thyroidectomy hypocalcemia for this study was 29.85±23.07 hours post-operatively. The most common manifestations of hypocalcemia were Chvostek’s sign and acral paresthesia present in 80.8% and 76.9% of patients, respectively. Other manifestations noted were perioral numbness (46.1%), carpopedal spasm (15.3%), Trousseau’s sign (7.7%) and cramps (3.8%) (Table 4).
Click here to download Table 4Table 4. Hypocalcemic manifestations
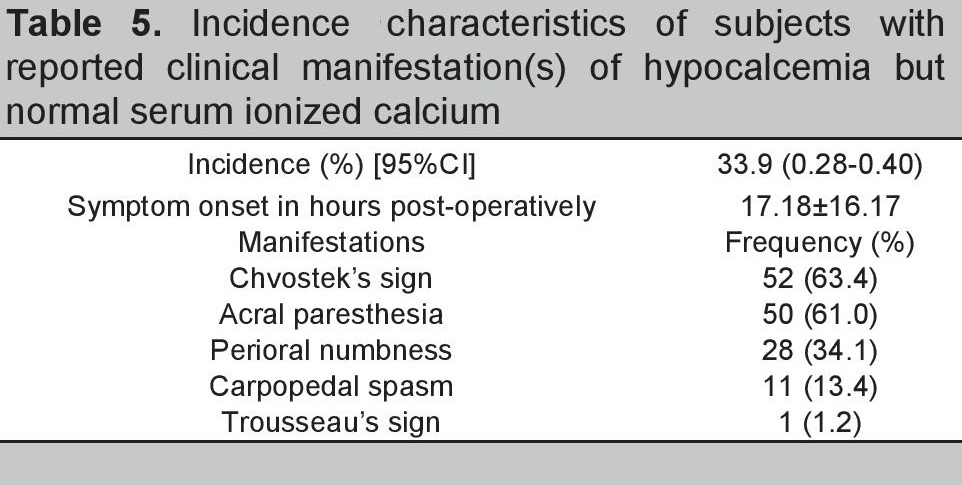
Eighty-two (82) subjects or 33.9% of the population studied, presented with clinical manifestations seen in patients with hypocalcemia but were noted to have normal serum ionized calcium level on testing. These patients presented with the symptoms at 17.18±16.17 hours post-operatively. Majority of these patients presented with positive Chvostek’s sign (52%) and acral paresthesia (50%) (Table 5).
Click here to download Table 5Table 5. Incidence characteristics of subjects with reported clinical manifestation(s) of hypocalcemia but normal serum ionized calcium
The overall incidence of post-thyroidectomy hypocalcemia in this study was 11.98%. This is lower than reported in the study of Mcleod, et al., in 2006.3 This incidence falls within the general rates reported in literature which varies widely depending on the population studied (i.e., extent of thyroidectomy, definition of hypocalcemia) and can reach up to >50%.15 The majority of hypocalcemic subjects in our study were symptomatic (10.74%). In a previous local retrospective study,12 the overall prevalence rate of post-thyroidectomy hypocalcemia was 21%. The type-specific rates were: 31% symptomatic (with or without low calcium levels), 16% true hypocalcemia, 26% asymptomatic hypocalcemia. However, direct comparison with the findings of this present study is not possible since the patients in the previous local study included subjects who underwent any extent of thyroidectomy, whereas the present study focused only on those who underwent total or completion thyroidectomy.
Most of the typical risk factors noted to be predictors of post-thyroidectomy hypocalcemia in literature were not found to be significantly associated with post-thyroidectomy hypocalcemia in the present study. These included the following: age, type of thyroid disease, thyroid gland weight, extent of thyroidectomy, performance of neck dissection and duration of surgery. Being a surgical procedure, success of thyroidectomy has been attributed to the experience of the surgeon. As such, complications may therefore be minimized under hands of an expert. However, for this study, there was no significant association noted in the post-thyroidectomy hypocalcemia between procedures done by consultants and trainees in our institution. This is consistent with one study where a review of 232 records of total thyroidectomies was done. Thyroidectomies done by endocrine surgery consultants were compared with those done by trainees. Safety, which was defined as postoperative hypoparathyroidism, recurrent laryngeal nerve palsy, and hemorrhage and efficacy defined as postoperative radioactive iodine uptake in the two groups were compared. Their results showed that the rates of occurrence of permanent hypoparathyroidism and recurrent laryngeal nerve palsy were comparable in the two groups and that postoperative radioactive iodine uptake was not significantly different.16
The finding in this study of a greater number of females who developed post-thyroidectomy hypocalcemia, though not statistically significant, may be attributed to females being more prone to calcium and vitamin D deficiency than males17 and considering the age group of this cohort, the female subjects would probably be perimenopausal as well. In one large study, female gender had an odds ratio of 1.62 (95%CI 1.45–1.80) (p<.001) in developing post-thyroidectomy hypocalcemia.7
The most significant finding in this study is the correlation of post-thyroidectomy hypocalcemia with the presence of hoarseness and/or hematoma (both of which are also post-thyroidectomy complications) and inadvertent parathyroidectomy. In one study, the incidence of transient hoarseness was noted to be at 6.86%,18 which is far less common than hypocalcemia. In this study, the presence of hoarseness and/or hematoma is strongly associated with the development of post-thyroidectomy hypocalcemia [OR 2.842 (95%CI: 1.142-7.069)]. Hoarseness depicts injury to the recurrent laryngeal nerve and is most often a result of extensive neck surgery, as in cases of large goiters or those who undergo neck dissection. Hematoma formation may also be attributed to extensive neck surgery. Both these complications may signify extensive neck tissue manipulation and injury with subsequent tissue swelling that can compromise the vascular supply of the parathyroid glands and cause hypocalcemia.
Inadvertent parathyroidectomy on the other hand is clearly associated with post-thyroidectomy hypocalcemia as shown in our study [OR 2.941 (95%CI: 1.252-6.907)]. Removal of the parathyroid glands can lead to transient or even permanent decrease in parathyroid hormone levels and lead to hypocalcemia.
The onset of hypocalcemia manifestations in the present study was noted to be 29.85±23.07 hours post-operatively, which means that hypocalcemia may occur as early as 6 hours up to >24 hours post-operatively. This is because the greatest decline in post-operative serum calcium levels, compared to pre-operative levels, can occur on the morning of the first post-operative day (12-18 hours after the operation) as seen in one study.14 Furthermore, the same researchers noted that a maximum of 36 hours was needed to observe a decrease in serum calcium levels close to those expected to cause symptoms.14 As for the manifestations, majority of the patients with hypocalcemia presented with a positive Chvostek’s sign (80.8%) and acral paresthesia (76.9%). But we are unable to validate these clinical findings due to the study design.
It is interesting that a significant number of subjects in our study (33.9%) presented with clinical manifestations of hypocalcemia, but had normal serum ionized calcium level on testing. This condition has been termed “symptomatic hypocalcemia” in several studies. The finding in our study contrasts with findings in 2 other studies. The study of Kim et al., in 2011 showed that among the 62 hypocalcemic patients in their study, only 9 patients (14.5%) met the criteria for symptomatic hypocalcemia. The other 45 patients (72.5%) experienced both symptomatic and biochemical abnormalities while the remaining 8 patients (12.9%) showed only biochemical hypocalce¬mia.15 In the study of Tolone et al., in 2013, they found that symptomatic hypocalcemia developed only in 9.5%, while laboratory hypocalcemia developed in 18%.6 This “mismatch” between the manifestations of hypocalcemia and biochemical evidence is also evident in one study where only 24 out of 45 patients (53.3%) presented with symptomatic and biochemical abnormalities on the same day. The mismatch was seen in the other 21 patients (46.6%). There was a 1-day gap between the initial occurrence of hypocalcemic symptoms/signs and bio¬chemical evidence in 11 patients (17.7%), a 2-day gap in 8 patients (12.9%), and a 3-day gap in 2 patients (3.2%).15 This “mismatch” occurs because symptoms may be affected by the velocity of the drop in calcium and not merely by calcium level itself.15 This explanation is difficult to substantiate in our study since pre-operative calcium levels were not determined, hence the degree of drop (or delta change) in serum calcium cannot be known. Furthermore, the manifestations of hypocalcemia are fairly non-specific and may be seen in other post-surgical patients as a result of anesthesia or other electrolyte abnormalities.
Analyzing post-thyroidectomy hypocalcemia may aid decisions on post-operative monitoring as well as prevention. This study showed 11.98% incidence of post-thyroidectomy hypocalcemia in our institution. Against this baseline the effects of reductions in morbidity may be measured in the future.
In the clinical prediction of patients who may develop post-thyroidectomy hypocalcemia, those who present with hoarseness and/or hematoma post-operatively should also be closely monitored for hypocalcemia, as these concomitant complications are strong risk factors for hypocalcemia. Patients who had inadvertent parathyroidectomy must also be monitored thoroughly during the immediate post-operative period and perhaps longer, since these patients are at greater risk for developing permanent hypoparathyroidism which may require lifetime supplementation with calcium and active vitamin D.
The mean time of onset of hypocalcemic manifestation shown in this study emphasizes the key role of vigilance in monitoring patients for hypocalcemia post-thyroidectomy even beyond the first post-operative day.
This study has several limitations. The retrospective nature of this study did not give the researchers the opportunity to validate the hypocalcemic manifestations reported in the charts. Also, it was not routine practice in our institution to request for calcium or vitamin D assays pre-operatively particularly in asymptomatic patients. Hence, the researchers cannot ascertain the calcium or vitamin D status of the patients pre-operatively but using the exclusion criteria of this study, most of the conditions that can affect these values were eliminated. To circumvent the above limitations, a prospective study is necessary. Most of the typical risk factors mentioned in literature were not significant in this study, but perhaps an extension and/or addition of more patients may either yield the same results or may show a difference.
The presence of hoarseness and/or hematoma were found to be strong risk factors. The exact mechanism is not clear, and we recommend further studies regarding this risk factor.
Also, a significant percentage of the study population presented with symptoms of hypocalcemia despite normal calcium levels. This “mismatch” may need further studies that is designed to eliminate confounding factors if possible, to elucidate the characteristics of such patients. Future researchers may also consider following-up these patients as to who developed or will develop permanent hypocalcemia.
AcknowledgementsThe authors are grateful for the help of Macario F. Reandelar, Jr. MD, MSPH in the statistical analysis of the data gathered for this study.
Statement of AuthorshipAll authors have approved the final version submitted.
Author DisclosureAll the authors declared no conflicts of interest.
Funding SourceNone.
1. Mirnezami R, Sahai A, Symes A, Jeddy T. Day-case and short-stay surgery: The future for thyroidectomy? Int J Clin Pract. 2007;61(7):1216-22. http://dx.doi.org/10.1111/j.1742-1241.2006.01234.x.
2. Hopkins B, Steward D. Outpatient thyroid surgery and the advances making it possible. Curr Opin Otolaryngol Head Neck Surg. 2009;17(2):95-9. PMID:19373959. 3. McLeod IK, Arciero C, Noordzij JP, et al. The use of rapid parathyroid hor-mone assay in predicting postoperative hypocalcemia after total or comple¬tion thyroidectomy. Thyroid. 2006;16(3):259–65. http://dx.doi.org/10.1089/thy.2006.16.259. 4. Abboud B, Sargi Z, Akkam M, Sleilaty F. Risk factors for post thyroidectomy hypocalcemia. J Am Coll Surg. 2002;195(4):456-61. http://dx.doi.org/10.1016/S1072-7515(02)01310-8. 5. Rosato L, Avenia N, Bernante P, et al. Complications of thyroid surgery: Analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J Surg. 2004;28(3):271-6. http://dx.doi.org/10.1007/s00268-003-6903-1. 6. Tolone S, Roberto R, del Genio G, et al. The impact of age and oral calcium and vitamin D supplements on postoperative hypocalcemia after total thyroidectomy. A prospective study. BMC Surgery. 2013;13(Suppl 2):S11. http://dx.doi.org/10.1186/1471-2482-13-S2-S11. 7. Baldassarre RL, Chang DC, Brumund, KT, and Bouvet M. Predictors of hypocalcemia after thyroidectomy: Results from the nationwide inpatient sample international scholarly research network. ISRN Surgery. 2012(2012), Article ID 838614. 8. Alhefdhi A, Mazeh H and Chen H. Role of postoperative vitamin D and/or calcium routine supplementation in preventing hypocalcemia after thyroidectomy: A systematic review and meta-analysis. The Oncologist. 2013;18(5):533–542. http://dx.doi.org/10.1634/theoncologist.2012-0283. 9. Pfleiderer, AG, Ahmad N, Draper, MR, Vrotsou K, Smith WK. The timing of calcium measurements in helping to predict temporary and permanent hypocalcaemia in patients having completion and total thyroidectomies. Ann R Coll Surg Engl. 2009;91(2):140–6. http://dx.doi.org/10.1308/003588409X359349. 10. McHenry CR, Piotrowski JJ. Thyroidectomy in patients with marked thyroid enlargament: Airway management, morbidity and outcome. Am J Surg 1994;60(8):586-91. PMID:8030813. 11. Zambudio AR, Rodriguez J, Riquelme J, Soria T, Canteras M, Parrilla P. Prospective study of postoperative complications after total thyroidectomy for multinodular goiters by surgeons with experience in endocrine surgery. Ann Surg. 2004;240(1):18-25. PMID: 15213613. 12. Celzo MFI, Picorro MAL, Alcances LRA, Jasul G. Clinical predictors of post-thyroidectomy hypocalcemia: A retrospective review. Philipp J Intern Med. 2005;43(6): 331-41. 13. Kim JP, Park JJ, Son HY, Kim RB, Kim HY, Woo, SH. Effectiveness of an i-PTH measurement in predicting post thyroidectomy hypocalcemia: Prospective controlled study. Yonsei Med J. 2013;54(3):637-42. http://dx.doi.org/10.3349/ymj.2013.54.3.637. 14. Tredici P, Grosso E, Gibelli B, Massaro MA, Arrigoni C, Tradati N. Identification of patients at high risk for hypocalcemia after total thyroidectomy. ACTA Otorhinolaryngologica Ital. 2011;31(3):144-8. PMCID: PMC3185817. 15. Kim JH, Chung MK, Son YI. Reliable early prediction for different types of post-thyroidectomy hypocalcemia. Clin Exp Otorhinolaryngol. 2011;4(2): 95-100. http://dx.doi.org/10.3342/ceo.2011.4.2.95. 16. Mishra A, Agarwal G, Agarwal A, and Mishra SK. Safety and efficacy of total thyroidectomy in hands of endocrine surgery trainees. Am J Surg. 1999; 178(5): 377–80. http://dx.doi.org/10.1016/S0002-9610(99)00196-8. 17. Bergenfelz A, Jansson S, Kristoffersson A, et al. Complications to thyroid surgery: Results as reported in a database from a multicenter audit comprising 3,660 patients. Langenbecks Arch Surg. 2008;393(5):667–73. http://dx.doi.org/10.1007/s00423-008-0366-7. 18. Fernando R, Chandrasinghe PC, Bandara M, Renuka MBS, Athulugama NS. Hypocalcemia and hoarseness following total thyroidectomy for benign disease: Relationship of incidence to the size of the gland. WJOES. 2011;3(1):7-9. http://dx.doi.org/10.5005/jp-journals-10002-1046.Authors are required to accomplish, sign and submit scanned copies of the JAFES Author Form consisting of: (1) the Authorship Certification that the manuscript has been read and approved by all authors, and that the requirements for authorship have been met by each author, (2) the Author Declaration that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere, (3) the Statement of Copyright Transfer [accepted manuscripts become the permanent property of the JAFES and are licensed with an Attribution-Share Alike-Non-Commercial Creative Commons License. Articles may be shared and adapted for non-commercial purposes as long as they are properly cited], (4) the Statement of Disclosure that there are no financial or other relationships that might lead to a conflict of interest. For Original Articles involving human participants, authors are required to submit a scanned copy of the Ethics Review Approval of their research. For manuscripts reporting data from studies involving animals, authors are required to submit a scanned copy of the Institutional Animal Care and Use Committee approval. For Case Reports or Series, and Images in Endocrinology, consent forms, are required for the publication of information about patients; otherwise, authors declared that all means have been exhausted for securing such consent. Articles and any other material published in the JAFES represent the work of the author(s) and should not be construed to reflect the opinions of the Editors or the Publisher.