Foot complications are a major cause of morbidity and disability in persons with diabetes mellitus.1 The lifetime risk of a patient with diabetes for foot ulcer is 25%, with an annual incidence of 2%. A diabetic foot ulcer starts with a triad of problems. First, neuropathy leading to the loss of protective sensation; second is foot deformity due to modulation at the neuromuscular junction where muscles are deprived of innervation leading to foot deformities; and lastly, trauma to the foot.2
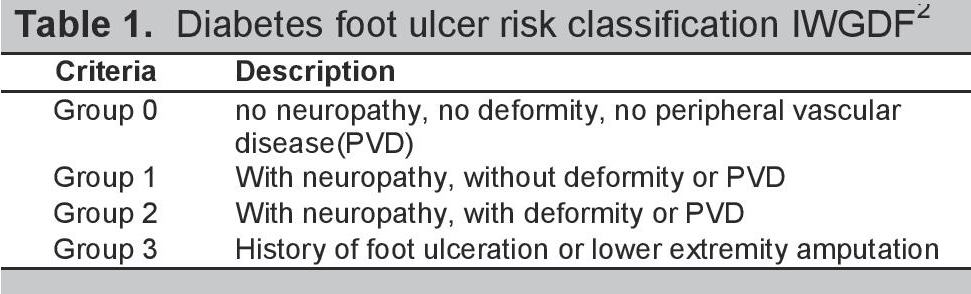
The International Working Group on the Diabetic Foot (IWGDF)2 has classified the risk of developing foot ulcer (Table 1), in spite of this, screening to prevent diabetic foot is often overlooked. The Australian Diabetes, Obesity, and Lifestyle Study (AusDiab)3 noted that in the past twelve months, 77% of their patients had an eye screening for retinopathy and only 49% subjected themselves to foot screening. Both eye and foot complications are manifestations of the microvascular complications of diabetes.
Click here to download Table 1Table 1. Diabetes foot ulcer risk classification IWGDF2
The IWGDF set the correct length of footwear at 1-2 cm longer than the foot. The internal width of the shoe should be equal to the width of the foot at the site of metatarsophalangeal joints.4
Flipflops are one of the most commonly used footwear among developing countries.5 Flipflops are described as an open-toed footwear with a flat sole held by a Y-shaped rubber strap that passes between the first and second toes and around both sides of the foot. They usually do not have a strap around the heels.
Despite the guidelines, 35-54% of foot ulcers are due to trauma from ill-fitting footwear.6-7 Half of the patients with diabetes and peripheral sensory neuropathy had footwear-related injury.8 Patients with diabetic foot ulceration were 5.1 times more likely to have poorly-fitting shoes. Foot-shoe size mismatches can disrupt the biomechanics of the foot and ankle, predisposing to pain and falls.9
Significance of the Study
Preference and knowledge on footwear for patients with diabetes influence the choice of shoes that patients buy, irregardless whether the shoe can fulfill or defeat its purpose as a protective device.
In the Philippines, information on knowledge of and compliance to appropriate footwear is minimal. This study aims to investigate the footwear preferences and practices among Filipino patients with diabetes. Clinical factors that contribute to or influence the use of inappropriate footwear will also be investigated.
The results of this research can provide clinicians and diabetes educators with information on foot and footwear practices and provide information for module formation
Objectives
General Objective
To determine general and clinical characteristics associated with the use of inappropriate footwear among Filipino patients with diabetes.
Specific Objectives
- To investigate the footwear preferences of diabetic patients;
- To determine the proportion of patients belonging to IWGDF diabetic foot ulcer risk groups 0, 1, 2, and 3;
- To determine the proportion of patients with diabetes who use footwear with improper lengths and widths;
- To compare the proportion of patients who use inappropriate footwear across the ulcer risk classification groups.
Study Subjects
Patients included in the study were patients who consulted at Makati Medical Center Outpatient Department.
Inclusion criteria
Patients with Type 1 or Type 2 Diabetes, age 18 years old and above. Patients must be able to read, comprehend and understand Filipino or English and must consent to join the study.
The diagnosis of diabetes mellitus is based on the Unite for Diabetes Philippines Clinical Practice Guidelines:10 Fasting Blood sugar ≥126 mg/dL; 2-hour plasma glucose ≥200 mg/dL after an oral glucose tolerance test; random blood sugar ≥200 mg/dL with signs or symptoms of diabetes.
Exclusion criteria
Impaired fasting glucose, impaired glucose tolerance, gestational diabetes, with foot dressings that may interfere with toe measurement (ulcer dressing), rheumatoid arthritis, limb prosthesis, cerebrovascular disease with residuals, hypothyroidism, currently treated for PTB, unable to maintain standing position, already included in this study from previous consultation, socioeconomic status.
Study Setting
The research was conducted at the Outpatient Department of Makati Medical Center, a tertiary hospital in Makati City, Philippines. The study subjects were all recruited from the Health Service Program of the hospital.
Study Design
Cross-sectional analytic
Sample Size
The minimum sample size was computed to be 169 based on the proportion of patients wearing inappropriate footwear= 46%11 with confidence level= 5%, margin of error= 5%, and estimated number of patients with diabetes during the sampling time= 300.
Recruitment and Sampling
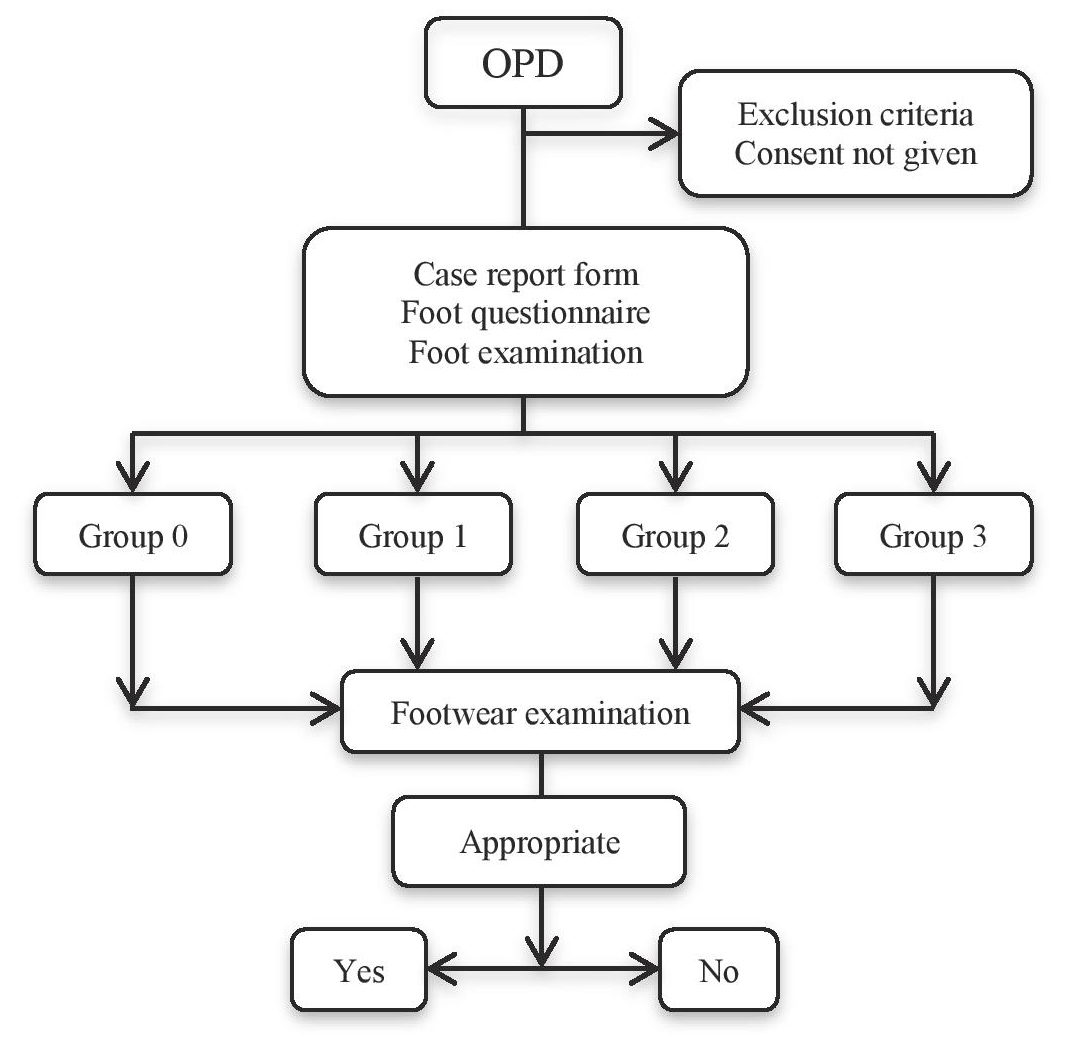
All patients who meet the inclusion criteria over a 9-week period were included in the analysis. The subjects were consecutively recruited (Figure 1).
Click here to download Figure 1Figure 1. Flow chart.
Study Procedure
Recruitment started after approval of the MMC Institutional Review Board (IRB). Patients were evaluated based on the inclusion/exclusion criteria.
Recruitment
Patients who qualified were invited to join the research. The principal investigator performed the recruitment process. The following were fully explained to the patient: purpose of the study, its risks and benefits, the personal information needed, the procedures to be performed, the materials to be used for foot examination. Patients who gave consent were recruited.
Case report form
An investigator administered a questionnaire regarding previous illnesses, demographics, diabetes history, diabetes control and cigarette smoking. Latest laboratory test results were noted. Diabetes control was determined using level of HbA1c. This research used <7% as cut-off for good diabetes control, based on the UNITE for Diabetes Philippine Guidelines.10
Foot questionnaire
Participants were given a questionnaire regarding foot history, knowledge and preferences. Pictures of different types and styles of men’s and women’s footwear were shown to the patient during the interview for easier identification of the types of footwear owned.
Foot examination12
A nurse educator who has specialized on foot care was hired as a research assistant of the principal investigator. The comprehensive foot examination is composed of the following:
Dermatologic:Visual inspection of both feet as to presence of the following:
- Dryness
- Fungal infection
- Nail dystrophy
- Swelling
- Corns
- Discharge
- Calluses
- Inflammation
- Erythema
- Fissures
Musculoskeletal: Visual inspection of both feet as to presence of the following:
- Hammer toes
- Claw toes
- Overlapping digits
- Bunion
- Charcot arthropathy
- Amputation of toes or foot
INTERPRETATION
DEFORMITY: when any of the aforementioned items is present.
Neurologic examination is composed of the following:
10-g Semmes-Weinstein monofilament test
Instruction: Apply the monofilament on the patient’s hands (or elbow or forehead) so that he or she knows what to expect. Ask patient to close his/her eyes. The monofilament is placed perpendicular to the skin on the 1st, 3rd, 5th metatarsal heads and plantar surface of hallux, with pressure applied until the monofilament buckles. It should be held for ~1 second then released.
Press the filament to the skin and ask the patient whether he feels the pressure applied by answering: YES or NO and where they feel the pressure by answering LEFT FOOT or RIGHT FOOT. Repeat this application twice at the same site but alternate this with at least one “mock” application in which no filament is applied (total of three questions per site).
Protective sensation is present at each site if the patient correctly answers two out of three applications. Protective sensation is absent when two out of the three answers are incorrect.
Vibration test using the 128-Hz tuning fork
Instruction: Apply the tuning fork on the patient’s wrists (elbow or clavicle) so that he or she knows what to expect. The patient must not be able to see where the examiner applies the tuning fork. The tuning fork is applied on a bony part on the dorsal side of the distal phalanx of the first toe. It should be applied perpendicularly with constant pressure. The patient will be asked if he or she felt the vibration by answering YES or NO and where he or she felt it by answering LEFT FOOT or RIGHT FOOT. The test is normal if the patient was able to feel the vibration.
Pinprick sensation
Instruction: A hair filament is applied proximal to the toenail on the dorsal surface of the hallux. Use just enough pressure to deform the skin. Ask the patient if he or she perceives the sensation by answering YES or NO and where he/she felt it by answering LEFT FOOT or RIGHT FOOT. An abnormal response is when there is inability to perceive it on either hallux.
INTERPRETATION
LOSS OF PROTECTIVE SENSATION (LOPS) was diagnosed when the patient has one or more abnormal results in section D.4C. We ruled out LOPS when the patient has at least two normal tests and no abnormal test.
Vascular examination involved palpation of the posterior tibial artery, dorsalis pedis artery and computation of the ankle brachial index (ABI).
Instruction: Place the blood pressure cuff above the dorsalis pedis then place the doppler probe over the dorsalis pedis artery.
![]()
Interpretation: Normal: 0.9-1.3
Foot Examination Assessment
Patients will then be classified into four categories based on the foot ulcer risks2 in Table 1.
Foot and shoe measurement
Both length and width were measured for foot, using Brannock’s device. The patient was asked to stand, the foot being measured was lifted and placed onto the base of the Brannock’s device13 with the heel firmly located against the back of the heel cup with the researcher firmly holding the subject’s ankle and heel cup together. Foot length was measured from the ankle to the longest toe. Foot width was measured at the level of the metatarsophalangeal joint.
The footwear to be assessed was what the patient was wearing during the clinic visit. It was assumed that the patient wears this shoe regularly. Shoe length was checked using plus12med shoe fitting device. Shoe width was measured using a sliding caliper in centimeters. Flipflops, sandals and open-type of footwear were recorded as inappropriate footwear, and their dimensions were not measured.
Appropriate footwear for this paper was defined as a closed-type of shoe, with length 1-2 cm longer than the foot and internal width equal to the width of the foot at the site of metatarsophalangeal joints.
Statistical Analysis
Descriptive statistics were used to summarize the clinical characteristics of the patients. Frequency and proportion were used for nominal variables, median and IQR for ordinal variables, and mean and SD for interval/ratio variables. Binary logistic regression was used to determine the risk factor associated with appropriateness of footwear. All valid data were included in the analysis. Missing variables were neither replaced nor estimated. Null hypothesis was rejected at 0.05 α-level of significance. STATA 12.0 was used for data analysis.
Ethical Considerations
This study was conducted in accordance to the ethical principles based on the Declaration of Helsinki and the National Guidelines for Biomedical Research of the National Ethics Committee (NEC) of the Philippines. The research protocol underwent approval from the Institutional Review Board (IRB).
All observations will be preceded by a written documentation of informed consent. Participation in the study was purely voluntary and without financial compensation. The interventions and data were recorded only in writing, and was not recorded via video nor audio. The results and patient information were kept strictly confidential by the primary investigator. A unique alphanumeric code was issued to each research subject and the subjects’ names did not appear in any of the data collection tools. The data were stored in the primary investigator’s database, password-protected, and the projected duration of storage would be at least ten years.
Psychosocial Support
Results of the foot examination and assessment of the footwear were fully disclosed and explained to the patient. The investigator enumerated ways of preventing the progression of areas at risk to foot ulcer or amputation. A pamphlet on proper foot care and footwear were given after the patient participated in the study. Follow-up care and further management of the results obtained from the study were endorsed to the patients’ attending physicians
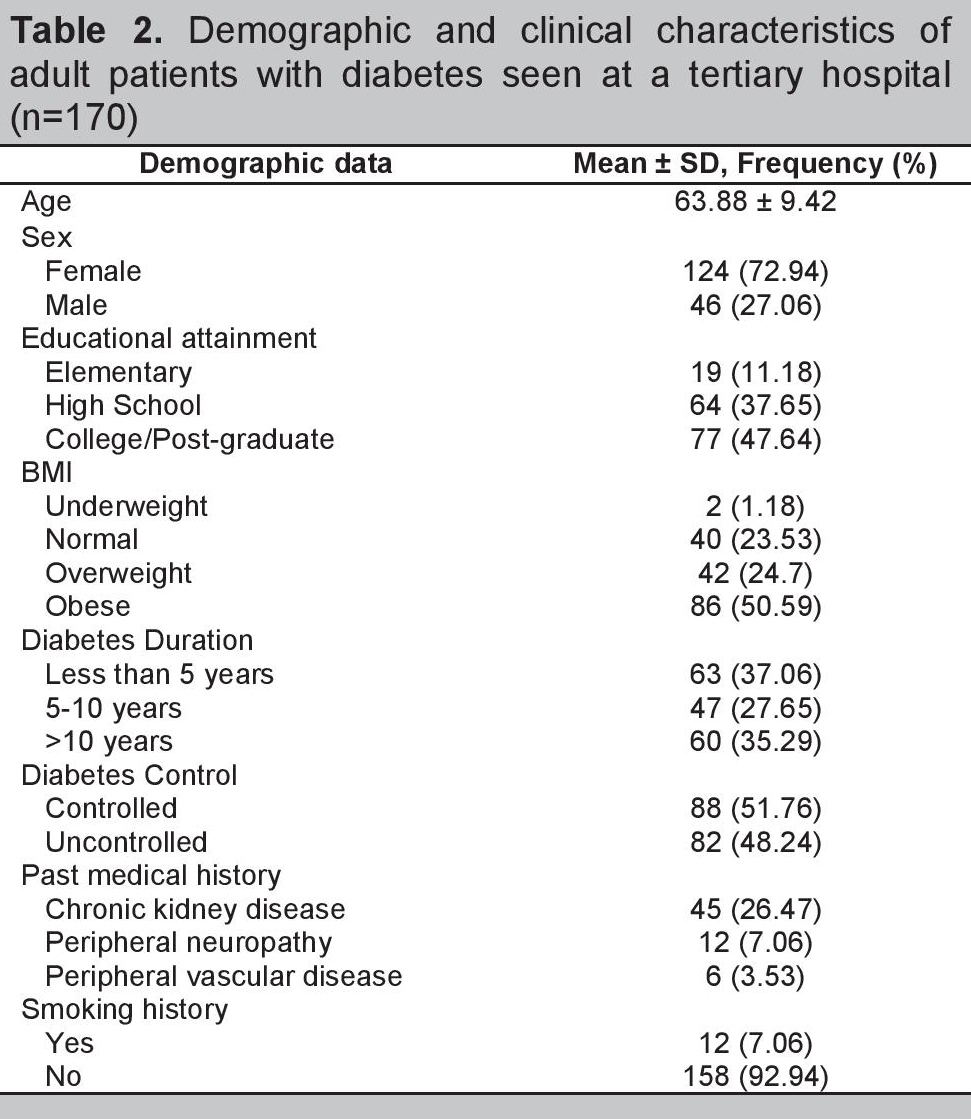
The total number of participants was 170, with a mean age of 64 years old, mostly females (72.94%), majority (88.82%) residing in Metro Manila. Nearly half (47%) were able to obtain college level education. Half the patients (50.59%) were obese based on the Body Mass Index Asia Pacific Classification. The duration of diabetes in 37.06% of the population was less than 5 years. Majority (81%) used oral hypoglycemic agents with half (51.76%) of them having good control of disease.
Hypertension was the most common co-morbidity; 7% of the population were smokers. Peripheral vascular disease was already diagnosed in 4% while 7% of the participants were currently treated for peripheral neuropathy (Table 2).
Click here to download Table 2Table 2. Demographic and clinical characteristics of adult patients with diabetes seen at a tertiary hospital (n=170) 2
For the foot history, 9% were reported to have foot ulcer, while 1% had undergone toe amputation. Numbness and burning/shooting pain were the most common symptoms experienced by these patients.
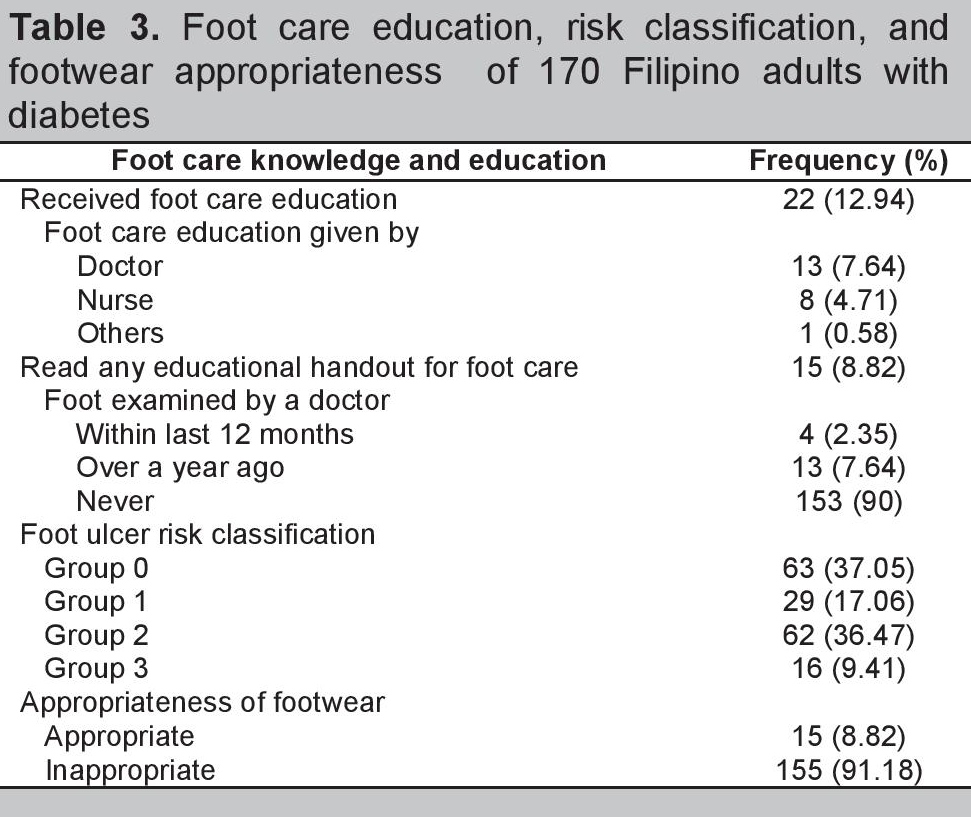
Regarding knowledge and education on foot care (Table 3), 87% reported they have not received foot care education. Of those who did receive foot care education, 59% were taught by a physician, 36% were instructed by a nurse.
Click here to download Table 3Table 3. Foot care education, risk classification, and footwear appropriateness of 170 Filipino adults with diabetes
Sandals were the most common footwear used upon consultation. Flipflops were the preferred footwear both at home and outside. Further analysis on indoor footwear showed more than half of the population (53%) preferred to walk barefoot, however, but only inside the house.
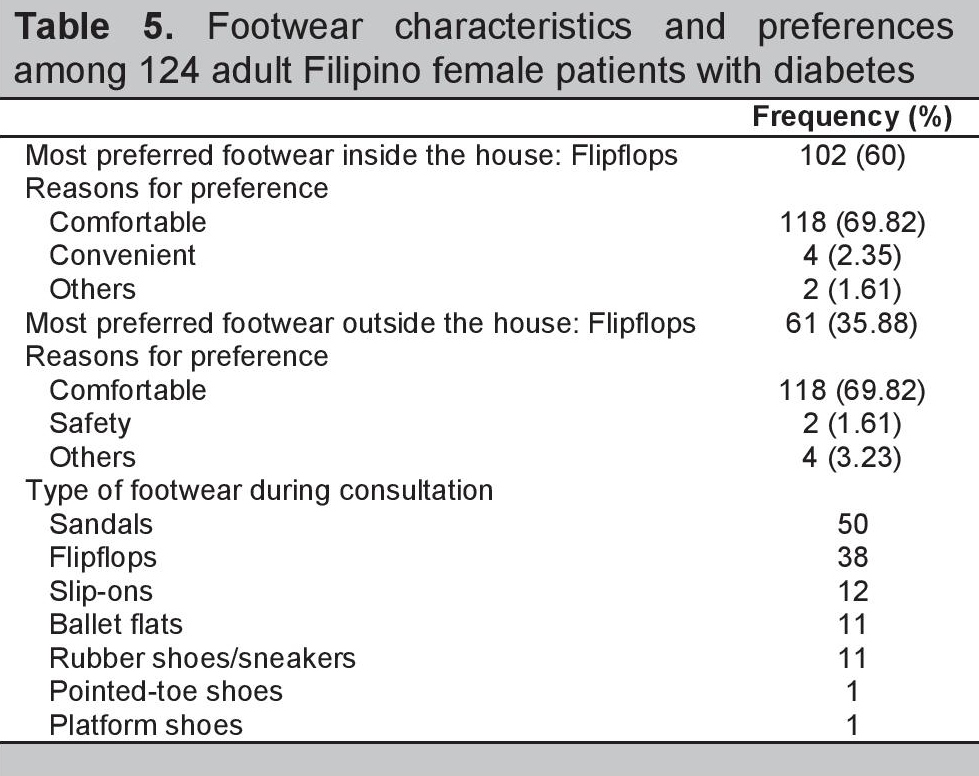
Comfort was the primary consideration in their choice for indoor and outdoor wear in 95% of the female and 86% of the male respondents. Only 6.5% of the males and 1.61% of the females considered foot safety as a reason for their preference (Tables 4 and 5).
Click here to download Table 4Table 4. Footwear characteristics and preferences among 46 adult Filipino male patients with diabetes
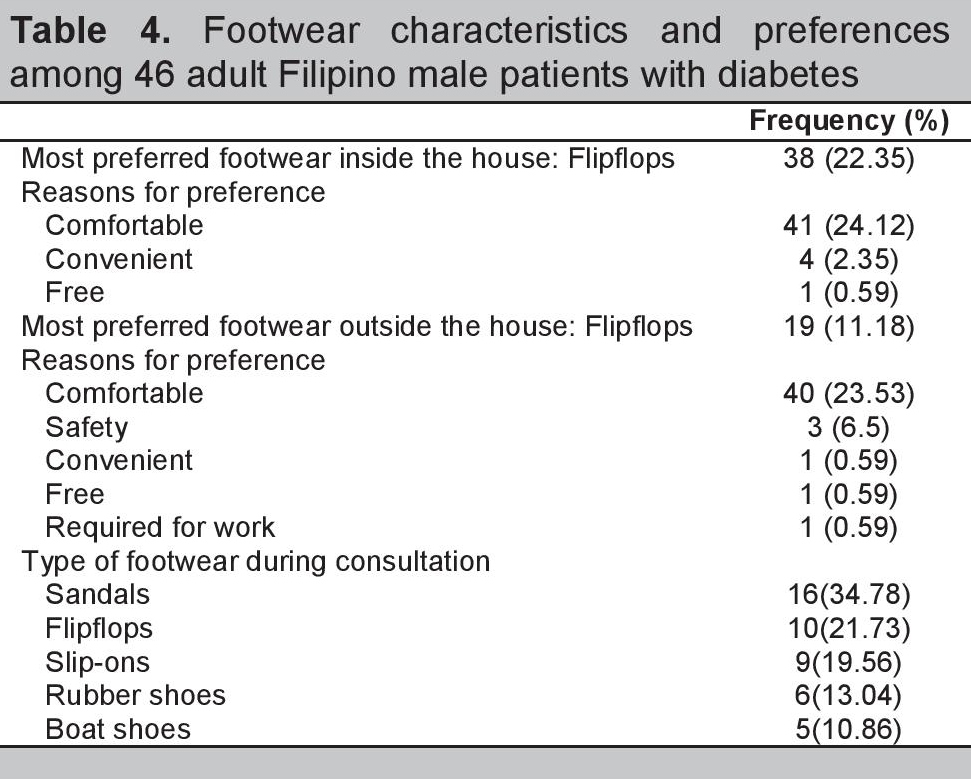
Click here to download Table 5
Table 5. Footwear characteristics and preferences among 124 adult Filipino female patients with diabetes
Upon foot examination, the most common dermatologic finding was dryness, seen in 51% of the population, followed by calluses at 13%. Of the 31% assessed to have a foot deformity, the majority was from bunions (17.06%). More than half (57%) had loss of protective sensation; about 19% had peripheral vascular disease.
Based on the foot ulcer risk classification, the majority of the patients belonged to Groups 0 and 2 (37% and 36% respectively), followed by Group 1 at 17%, and lastly Group 3 at 9%. Combining the groups at risk (Groups 1-3), 62% of the population analyzed were at risk for foot ulcer.
Of the 170 subjects, foot to shoe length and width measurements were performed in 78 of the participants; the rest of the participants were excluded because their footwear was inappropriate for patients with diabetes. Of the patients whose shoes were measured, 15 had appropriate and 63 had inappropriate footwear.
Of the 63 patients who had inappropriate shoes, 13 participants had disparity in foot to shoe length, while 10 participants had disparity in foot to shoe width. Of the female participants, 21 had inappropriate foot to shoe length and 19 had inappropriate foot to shoe width. Overall, 91% of the respondents wore inappropriate footwear.
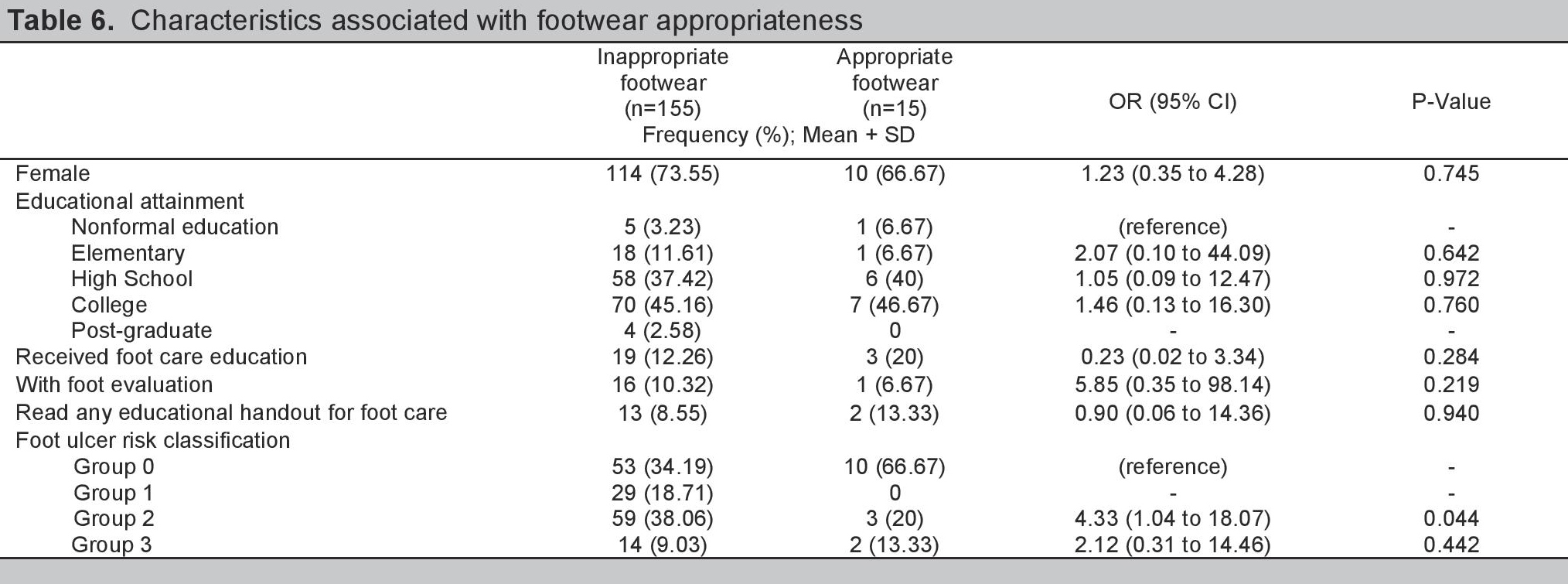
In Table 6, binary logistic regression was conducted with select patient characteristics in the model. It showed insufficient evidence to determine an association between the use of inappropriate footwear and patient sex, educational attainment, foot care evaluation and examination. Among the foot ulcer risk classification groups, results suggest that patients in the ulcer risk classification Group 2, compared to Group 0, were more likely to use inappropriate footwear (OR 4.33, 95% CI 1.04 to 18.07, p = 0.044). For foot ulcer risk Group 3, we had insufficient evidence to demonstrate a significant difference between this foot ulcer risk group versus Group 0.
Click here to download Table 6Table 6. Characteristics associated with footwear appropriateness
This study evaluated the general characteristics associated with inappropriate footwear. Results showed only 8.82% of the population wore appropriate footwear. This result is lower compared to the studies of Nixon et al.9 among US veterans with diabetes and Harrison et al.15 which showed 25.5% and 24% of the subjects, respectively, wore appropriate footwear.
The IWGDF16 described an appropriate shoe as one that is well-fitted, comfortable and can protect the foot from injury. In this study, our poor results can be attributed to several factors, but at the top of the list was the patient’s predilection to wear flipflops or open-type sandals. It was the primary choice of footwear among 82% of the respondents for indoors and 47% for outdoors. These data were higher compared to the study done by Chandalia et al.14 in India, where flipflops were the primary choice in 48% of the respondents. This was also validated in a study by Morbach et al.5 who concluded that flipflops were preferred in developing countries such as India (65%) and Tanzania (88%). Flipflops are inappropriate because these are open-type footwear which fail to protect the foot from injuries.
The tendency to develop foot ulcers is compounded because 53% of the respondents said “walking barefoot” was their secondary preference for indoors. The IWGDF16 recommends avoiding walking barefoot because this is a common source of foot injuries. This finding is also evident in a study done in India14 where 45% of the participants also walked barefoot indoors
Comfort was the foremost consideration for footwear preference, the Philippines is a tropical country with humid temperatures most days of the year and flipflops, which are open-type sandals, are the most comfortable type of footwear for our climate.
This is a dilemma for clinicians and diabetes educators who must reconcile what footwear is comfortable versus what is protective for the patient’s feet. The description of protective footwear in the guidelines4,16 is made for countries with cooler climates and good podiatry services.
Prescriptive footwear is advised for patients with foot ulcer risk in categories 1-3.4,16 These types of footwear are manufactured by a pedorthist who can custom-made a shoe to compensate for a foot deformity or LOPS. However, the majority of patients with diabetes in developing countries do not have access to a podiatrist or a pedorthist who can tailor-fit a shoe to become an “appropriate footwear.” Therefore, it is not logistically feasible in our setting to follow the recommendations of our Western counterparts. Second, if a customized shoe is not an option, there is no local or international guideline, even from major societies, which can assist clinicians from developing countries on how to advice patients with diabetes belonging to categories 1-3 in their choice for off-the-shelf footwear that can be a good alternative for a customized shoe. The challenge for diabetes educators and clinicians is to make guidelines on how to choose an “appropriate footwear” for patients with diabetes with foot ulcer risk in developing countries
This sentiment was also reflected in the most recent IWGDF 2015 guideline16 on footwear and offloading. The article highlighted the controversy on how to apply the guideline to developing countries, noting that the current research on footwear and foot care mostly originate from economically developed regions. It emphasized that specific recommendations are needed for developing countries, because of the differences in climate, resources, adherence and efficacy.
People with diabetic neuropathy often wear shoes that are too small in order to increase the sensation of fit.17 These findings were not demonstrated in this study.
Binary logistic regression was used to determine association between appropriateness of shoe size in relation to associated factors. Of particular interest are the patients who received foot care education and those with higher levels of educational attainment who are expected to have appropriate footwear. However, there was no difference among educational levels and those who received foot care education. This finding is similar to a Cochrane metaanalysis18 where education had a short-term influence on foot care knowledge and patient behavior. One RCT19 concluded that the difference in foot care knowledge between intervention and control group disappeared after seven years. Lastly, Lincoln et al.20 concluded that limited education did not reduce the incidence of foot ulcer and amputation. Hence, one-time foot care education is not sufficient to protect patients from lower extremity complications. This highlights the need for physicians to continually remind patients on proper foot care and footwear to prevent foot ulcers and amputation.
For foot ulcer risk classification, Group 2 patients were more likely to wear inappropriate footwear compared to Group 0. Group 3 did not reach statistical significance probably because of the small sample size of the group. Nevertheless, there is a trend for higher group levels to wear inappropriate footwear.
Majority (91%) of the participants wear inappropriate footwear. This finding is due to multifactorial causes: preference, climate, economic reasons and foot ulcer risk category. Educational attainment and foot care education did not improve the statistics of footwear appropriateness. Flipflops and sandals are the primary preferences of the participants. This study has shown that there is benefit to developing local guidelines on proper footwear for patients with diabetes because of the difference in demographics among countries.
AcknowledgementsWe would like to thank the section of Endocrinology of Makati Medical Center for its continued support to its trainees for research.
Statement of AuthorshipAll authors have approved the final version submitted.
Author DisclosureAll the authors declared no conflicts of interest.
Funding SourceNone.
1. International Diabetes Federation Consultative Section, International Working Group on the Diabetic Foot. Diabetes and foot care: Time to act. IDF, 2005.
2. Peters EJG, Lavery LA. Effectiveness of the diabetic foot risk classification system of the International Working Group on the Diabetic Foot. Diabetes Care. 2001;24(8):1442-7. http://dx.doi.org/10.2337/diacare.24.8.1442. 3. Tapp RJ, Zimmet P, Harper A, et al. Diabetes care in Australian population. Frequency of screening examinations for eye and foot complications of diabetes. Diabetes Care. 2004; 27(3):688-93. http://dx.doi.org/10.2337/diacare.27.3.688. 4. Bakker K, Appelqvist J, Schaper J, for the International Working Group on the Diabetic Foot Editorial Boardt. Practical guidelines on the management and prevention of the diabetic foot 2011. Diabetes Metab Res Rev. 2012;28(Suppl 1):225–31. http://dx.doi.org/10.1002/dmrr.2253. 5. Morbach S, Lutale JK, Viswanathan V, et al. Regional differences in risk factors and clinical presentation of diabetic foot lesions. Diabetic Med. 2004;21(1):91-5. http://dx.doi.org/10.1046/j.1464-5491.2003.01069.x. 6. MacFarlane RM, Jeffcoate WJ. Factors contributing to the presentation of diabetic foot ulcers. Diabetic Med. 1997;14(10):867–70. http://dx.doi.org/10.1002/(SICI)1096-9136(199710)14:10<867::AID-DIA475>3.0.CO;2-L. 7. McGill M, Molyneaux L, Yue DK. Which diabetic patients should receive podiatry care? An objective analysis. Intern Med J. 2005;35(8):451-6. http://dx.doi.org/10.1111/j.1445-5994.2005.00880.x. 8. Reiber G. Who is at risk of limb loss and what to do about it? J Rehabil Res Dev. November 1994;31(4):357–62. 9. Nixon BP, Armstrong DG, Wendell C, et al. Do US Veterans wear appropriately sized shoes? The veterans affairs shoe size selection study. J Am Podiatr Med Assoc. 2006;96(4):290-2. http://dx.doi.org/10.7547/0960290. 10. UNITE for Diabetes Philippines. Available at http://obesity.org.ph/v4/wp-content/uploads/2014/07/Diabetes-United-for-Diabetes-Phil.pdf. Accessed November 2015. 11. Mwandri MB. The outcome of using the 60-second diabetic foot screen to identify the diabetic foot at risk in Tanzania. Wound Healing Southern Africa. 2012;5(2):86-9. 12. Boulton A, Armstrong D, Albert S, et al. Comprehensive foot examination and risk assessment. Diabetes Care. 2008;31(8):1679-85. http://dx.doi.org/10.2337/dc08-9021. 13. Instructions and fitting tips. Available at http://brannock.com/pages/instructions-fitting-tips. Accessed March 2016. 14. Chandalia HB, Singh D, Kapoor V, Lamba PS. Footwear and foot care knowledge as risk factors for foot problems in Indian diabetics. Int J Diabetes Dev Ctries. 2008;28(4):109–13. http://dx.doi.org/10.4103/0973-3930.45269. 15. Harrison SJ, Cochrane L, Abboud RJ, Leese GP. Do patients with diabetes wear shoes of the correct size? Int J Clin Pract. 2007;61(11):1900-4. http://dx.doi.org/10.1111/j.1742-1241.2007.01554.x. 16. Bus SA, Armstrong DG, van Deursen RW, et al. IWGDF Guidance on footwear and offloading interventions to prevent and heal foot ulcer in patients with diabetes. Available at http://www.iwgdf.org/files/2015/website_footwearoffloading.pdf. Accessed February 14,2016. 17. Parnés A. If the shoe fits … footwear and patients with diabetes. Int J Clin Pract. 2007;61(11):1779–90. http://dx.doi.org/10.1111/j.1742-1241.2007.01581.x. 18. Dorresteijn JAN, Kriegsman DMW, Assendelft WJJ, Valk GD. Patient education for preventing diabetic foot ulceration. Cochrane Database Syst Rev. 2014;12:1-55. http://dx.doi.org/10.1002/14651858.CD001488.pub5. 19. Hämäläinen H, Rönnemaa T, Toikka T, Liukkonen I. Long-term effects of one year of intensified podiatric activities on foot care knowledge and self-care habits in patients with diabetes. The Diabetes Educator. 1998;24(6): 734-40. http://dx.doi.org/10.1177/014572179802400609. 20. Lincoln NB, Radford KA, Game FL, Jeffcoate WJ. Education for secondary prevention of foot ulcers in people with diabetes: A randomized controlled trial. Diabetalogia. 2008;51(11):1954-61. http://dx.doi.org/10.1007/s00125-008-1110-0.Authors are required to accomplish, sign and submit scanned copies of the JAFES Author Form consisting of: (1) the Authorship Certification that the manuscript has been read and approved by all authors, and that the requirements for authorship have been met by each author, (2) the Author Declaration that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere, (3) the Statement of Copyright Transfer [accepted manuscripts become the permanent property of the JAFES and are licensed with an Attribution-Share Alike-Non-Commercial Creative Commons License. Articles may be shared and adapted for non-commercial purposes as long as they are properly cited], (4) the Statement of Disclosure that there are no financial or other relationships that might lead to a conflict of interest. For Original Articles involving human participants, authors are required to submit a scanned copy of the Ethics Review Approval of their research. For manuscripts reporting data from studies involving animals, authors are required to submit a scanned copy of the Institutional Animal Care and Use Committee approval. For Case Reports or Series, and Images in Endocrinology, consent forms, are required for the publication of information about patients; otherwise, authors declared that all means have been exhausted for securing such consent. Articles and any other material published in the JAFES represent the work of the author(s) and should not be construed to reflect the opinions of the Editors or the Publisher.