A 59-year-old female was referred for asymptomatic hypercalcemia (calcium 12.5 mg/dl, albumin 3.2 mg/dl) detected on routine health check. She complained of having a neck swelling which had not increased over the last 1year. She denied history of bone pains, fractures or renal calculi. She was postmenopausal since 10 years ago and had hypertension for 2 years. She was also diagnosed to have diabetes during the health check up and was started on oral hypoglycaemic agents. Clinically she was euthyroid and had a 5cm × 5cm, firm, well defined neck swelling which moved with deglutition. There was no bruit or lymphadenopathy. There was no family history of any thyroid or parathyroid dysfunction.
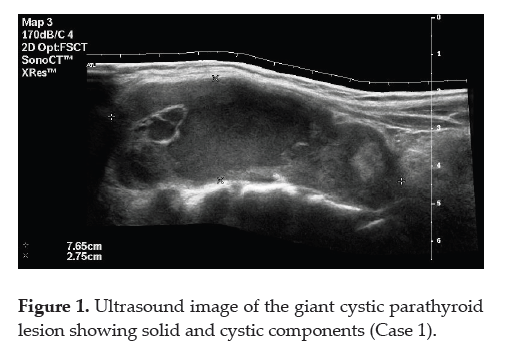
Her repeat serum calcium was 11.9 mg/dl, phosphorus 2.1 mg/dl with corresponding PTH levels 879 pg/ml and creatinine 1.6 mg/dl. Ultrasonography (USG) of the neck showed a 7 × 3 cm complex mass on the posterior aspect of the left thyroid lobe sharply demarcated by a capsule with an anechoic 5 × 2 cm cystic area within it (Figure 1,2). USG of the abdomen and pelvis revealed a 1.8 × 1.5cm calculus in the left renal pelvis with mild hydronephrosis. Her parathyroid sestamibi scan showed retention of tracer in the left lower pole of the thyroid gland on delayed images suggestive of parathyroid adenoma.
Click here to download Figure 1
Figure 1. Ultrasound image of the giant cystic parathyroid lesion showing solid and cystic components (Case 1).
Click here to download Figure 2
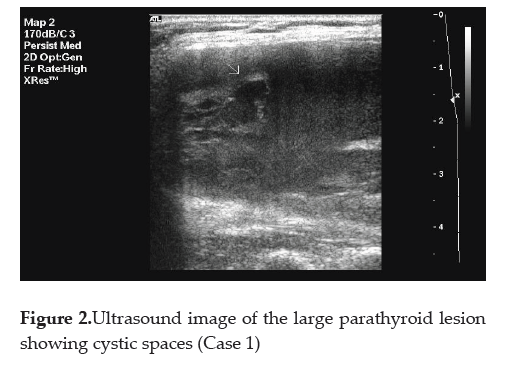
Figure 2. Ultrasound image of the large parathyroid lesion showing cystic spaces (Case 1)
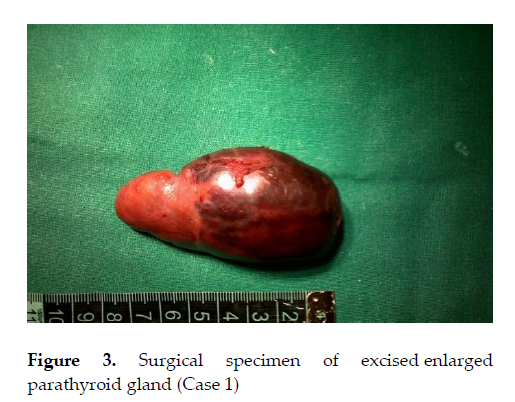
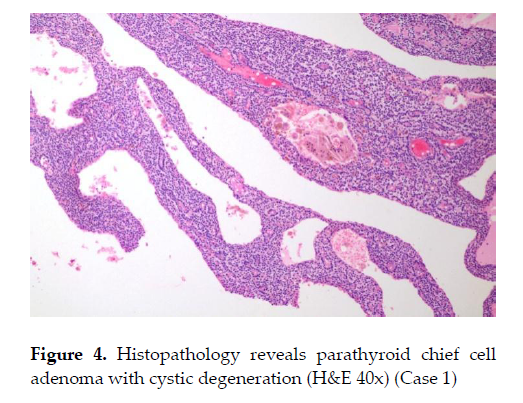
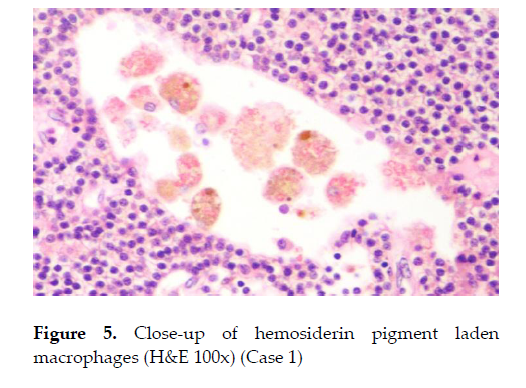
She underwent left parathyroidectomy and intra-op PTH levels decreased to 46.7pg/ml after 20 minutes. Histopathology showed 7 × 4 × 3 cm oval lobulated encapsulated mass, with solid and cystic areas (Figure 3). Microscopic examination confirmed parathyroid chief cell adenoma with cystic changes (Figure 4,5). Post operatively her calcium level dropped to 9 mg/dl and she recovered well from the surgery. She has been asked to undergo surgery for the renal calculus at a later date.
Click here to download Figure 3
Figure 3. Surgical specimen of excised enlarged parathyroid gland (Case 1)
Click here to download Figure 4
Figure 4. Histopathology reveals parathyroid chief cell adenoma with cystic degeneration (H&E 40x) (Case 1)
Click here to download Figure 5
Figure 5. Close-up of hemosiderin pigment laden macrophages (H&E 100x) (Case 1)
A 74-year-old female presented with increasing weakness, anorexia and constipation since a month prior to consult. Relatives noticed that she was sleepy throughout the day and had lost 4 kgs over the last 1 month. She was a known hypertensive for the past 10 years, well- controlled on a single oral antihypertensive agent. She was postmenopausal since 25 years ago. She had no history of renal calculi. On examination, there was no evidence of goiter or neck swelling. Systemic examination was normal. On evaluation, her serum calcium level was 18mg/dl, phosphorus 5 mg/dl, creatinine 2.3mg/dl, PTH 2138 pg/ml and 25 Vit D 49.5 ng/ml. An USG of the neck revealed a 3.6 x 2.5 cm cystic thyroid nodule on the right side with a 6 x 4 mm suspicious left inferior parathyroid nodule. Sestamibi scan showed persistent tracer uptake around the lower pole of the right thyroid gland suggestive of parathyroid adenoma. She underwent right inferior parathyroidectomy with intraoperative PTH levels declining to 350 pg/ml. Intraoperative findings revealed a 3 x 2 cm partly cystic nodule weighing 3.5gms. The left inferior parathyroid gland was normal. Microscopic examination confirmed parathyroid adenoma with cystic changes. Postoperatively her calcium level and creatinine normalized within 5 days.
A 62-year-old male presented with a gradually increasing midline neck swelling since 4 months ago together with bone pains and generalized weakness since 3 months ago. He had undergone left inferior parathyroidectomy 5 years back for primary hyperparathyroidism when he presented with bone pains, polyuria and renal calculi. Five years ago, he was also diagnosed to have hypogonadism secondary to empty sella and was advised androgen replacement therapy which he did not start. Clinically there was a 3 x 2 cm midline swelling in the neck, cystic in consistency, moving with deglutition. Systemic examination was normal. On evaluation, serum calcium level was 12.1 mg/dl, phosphorus 3.7 mg/dl, creatinine 1.0 mg/dl, PTH 257 pg/ml, 25VitD 10.7 ng/ml, T3 146ng/dl, T4 8.4 µg/dl and TSH 1.15 µIU/ml. An USG of the neck revealed a 2.9 x 1.9 x 1.9 cm (volume 5.2 cc) large, cystic, oval mass anterior to the isthmus with minimal peripheral vascularity. Sestamibi-SPECT scan showed persistent tracer uptake in the nodule anterior to the isthmus suggestive of parathyroid adenoma. A FNAC revealed parathyroid cell clusters and fluid PTH levels were 25000 pg/ml. As MEN1 syndrome was suspected (in view of recurrent primary hyperparathyroidism with hypopituitarism probably secondary to infarction of pituitary adenoma), he underwent total parathyroidectomy with reimplantation of half of a parathyroid gland in the forearm. Histopathology of the nodule weighing 16 mg revealed parathyroid hyperplasia. The other parathyroid glands were also found to be hyperplastic. Postoperatively his calcium level decreased to 7.8 mg/dl and he was treated with calcium and Vitamin D supplementation. Later, he was worked up for hypopituitarism and started on hormone replacement therapy on an outpatient basis.
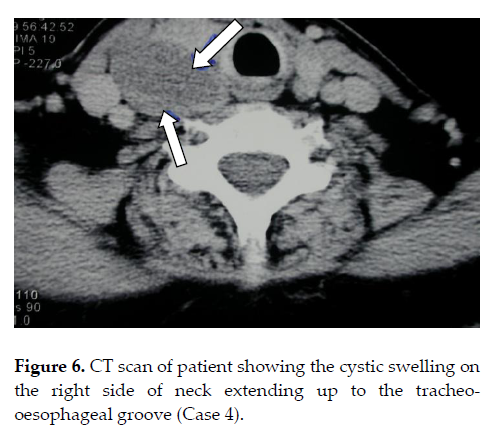
A 52-year-old female presented with history of intermittent dysphagia for solids and liquids since 2 years ago. She had undergone upper GI endoscopy with dilatation on three occasions at different centers. On examination, she had neck fullness on the right with increased local warmth. Barium swallow showed proximal esophagus deviated to the left. A CT scan revealed a 9 X 5 X 3 cm soft tissue collection on the right paratracheal region displacing the thyroid gland anteriorly at C3-T2 level (Figure 6). She underwent excision of the cystic mass (hemorrhagic fluid). The swelling was reported to be a parathyroid cyst on histopathology. Unfortunately she was referred to us only after the histopathology reports. Preoperative calcium and PTH measurements were not available as this pathology was not suspected. Postoperatively her calcium levels were 9mg/dl, albumin 3.4mg/dl, phosphorus 2.6mg/dl and PTH 343 pg/ml.
Click here to download Figure 6
Figure 6. CT scan of patient showing the cystic swelling on the right side of neck extending upto the tracheo-oesophageal groove (Case 4).
Here we describe 4 cases with cystic lesions of the parathyroid gland. Three of these (Cases 1,2 and 3) had parathyroid adenomas with cystic degeneration whereas Case 4 had a true parathyroid cyst. Cystic lesions of the parathyroid gland are rare (0.5%–1% of all parathyroid pathologies). Macroscopic cysts larger than 1 cm in diameter are referred to as parathyroid cysts and necessitate further investigation.2 Some investigators have suggested that the true prevalence of parathyroid cysts remains uncertain and that these lesions may occur more frequently than is generally appreciated.3 Cystic lesions of the parathyroid gland can be either due to true parathyroid cyst as seen in Case 4 or due to cystic degeneration of parathyroid adenoma as seen in Cases 1, 2 and 3. Most of the parathyroid gland adenomas are solid while cystic degeneration is seen in 1-2% of patients with primary hyperparathyroidism.
Approximately 90% of true parathyroid cysts are classified as nonfunctioning cysts with normal calcium concentrations and 10% are functioning cysts with elevated calcium concentration.1-3 However, in one study functioning parathyroid cysts were more common.4 True parathyroid cyst needs to be differentiated from parathyroid adenoma with cystic degeneration. Parathyroid cysts are more frequent in females between 20 to 60 years of age, whereas parathyroid adenomas are more common after 50 years of age.5
Patients with true nonfunctional parathyroid cysts present with compressive symptoms. On the other hand, patients with true functional parathyroid cysts and patients with cystic parathyroid adenoma present with signs and symptoms of hypercalcemia.
Parathyroid cysts are of variable sizes, ranging from 1 to 10 cm in greatest dimension, with the average cyst measuring approximately 3 to 5 cm. In 85 - 90% of cases, they are located in the neck and often involve the inferior parathyroid glands.2, 3, 5 In 5 - 10% of cases they have been detected at ectopic sites anywhere from the angle of the mandible to the mediastinum.5 The mediastinal location of the parathyroid cyst can be ascribed to two factors. First, the cyst may descend into the mediastinum because of the weight and negative intrathoracic pressure. Second, an aberrant mediastinal parathyroid gland may give rise to the cyst.2
Degeneration of an existing parathyroid adenoma secondary to hemorrhage into the adenoma, also results in cyst formation. The other different theories proposed are: (1) retention of glandular secretions, (2) persistence of vestigial pharyngobranchial ducts, (3) persistence of Kursteiner's canals, (4) enlargement of a microcyst, or (5) coalescence of the microcysts.2,6 None of these theories is universally applicable, and the processes leading to cyst formation may well differ from one person to the next.
Ultrasonography may reveal a nonspecific cystic structure.1 Analysis of the aspirate generally reveals elevated PTH level, diagnostic of parathyroid cyst.1,5 Nonfunctional parathyroid cysts have high fluid PTH concentrations, in conjunction with normal serum PTH concentrations. 7 In functional parathyroid cysts, cystic fluid PTH levels can reach several million pg/ml.8 PTH levels in the cystic fluid were measured only in the fourth patient.
The histologic distinction between a cystic parathyroid adenoma and the rare functional parathyroid cyst is made by the former having a preponderance of chief cells with multilocular degenerative thick-walled cysts and the latter usually consisting of a unilocular thin-walled cyst.
Treatment strategies for parathyroid cysts include surgical excision or aspiration or injection of sclerosing agents.1 Surgical treatment seems to be the preferred intervention for functional and symptomatic parathyroid cysts as in our patient.1 Fine-needle aspiration yields the diagnosis and may be considered the treatment of choice for nonfunctional parathyroid cysts. It leads to cystic regression without recurrence.1 Several reports in the literature support fine-needle aspiration as a therapeutic modality.1,7,8 For recurrent nonfunctional parathyroid cyst, sclerotherapy with use of tetracycline and alcohol has also been described. It has been effective but is associated with the risk of subsequent fibrosis and recurrent laryngeal nerve palsy.1 If aspiration cannot be done safely or the cyst recurs after successful aspiration, surgical excision should be done.5
1. Fortson JK, Patel VG, Henderson VJ. Parathyroid cysts: A case report and review of the literature. Laryngoscope. 2001;111:1726-1728.
2. Gurbuz AT, Peetz ME. Giant mediastinal parathyroid cyst: An unusual cause of hypercalcemic crisis—case report and review of the literature. Surgery. 1996;120:795-800.
3. Safran D. Functioning parathyroid cyst. South Med J. 1998;91:978-980.
4. McCoy KL, Yim JH, Zuckerbraun BS et al. Cystic parathyroid lesion: Functional and nonfunctional parathyroid cysts. Arch Surg 2009 Jan;144(1):52-6
5. Ihm PS, Dray T, Sofferman RA, Nathan M, Hardin NJ. Parathyroid cysts: Diagnosis and management. Laryngoscope. 2001;111:1576-1578.
6. Shields TW, Immerman SC. Mediastinal parathyroid cysts revisited. Ann Thorac Surg. 1999;67:581-590.
7. Pacini F, Antonelli A, Lari R, Gasperini L, Baschieri L, Pinchera A. Unsuspected parathyroid cysts diagnosed by measurement of thyroglobulin and parathyroid hormone concentrations in fluid aspirates. Ann Intern Med. 1985; 102:793-794.
8. Spitz AF. Management of a functioning mediastinal parathyroid cyst. J Clin Endocrinol Metab. 1995;80:2866-2868.
Articles and any other material published in the JAFES represent the work of the author(s) and should not be construed to reflect the opinions of the Editors or the Publisher.
Authors are required to accomplish, sign and submit scanned copies of the JAFES Declaration that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere.
Consent forms, as appropriate, have been secured for the publication of information about patients; otherwise, authors declared that all means have been exhausted for securing such consent.
The authors have signed disclosures that there are no financial or other relationships that might lead to a conflict of interest. All authors are required to submit Authorship Certifications that the manuscript has been read and approved by all authors, and that the requirements for authorship have been met by each author.