The global burden of Type 2 Diabetes Mellitus (T2DM) is rapidly increasing. Data shows that the prevalence of T2DM for all age-groups will double worldwide to 4.4% in the year 2030, with the highest burden in the Asia-Pacific.1,2 In the Philippines alone, the prevalence of diabetes was estimated to be 4.8%, afflicting approximately more than three million Filipinos,3 ranking 8th among leading causes of mortality among Filipino adults.4
T2DM is a chronic and progressive metabolic disorder characterized by elevated levels of blood glucose. Previously, it was primarily a disease of the elderly but because of changing lifestyles, it now affects even the younger population.5 It is possible to reverse the effects and complications of T2DM early in its course. Its treatment goals include maintaining the patient’s glycosylated hemoglobin (HbA1c) level to less than 7% as recommended by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD).6,7 Despite developments in the pharmacologic armamentarium for T2DM, self-care behavior remains the cornerstone of treatment.8 Self-care behavior pertains to various tasks that the patient performs in order to manage the disease. In 2007, the American Association of Diabetes Educators (AADE) identified seven self-care behaviors proven to have direct impact on T2DM management; these include 1) healthy eating, 2) being active, 3) glucose monitoring, 4) medication adherence, 5) problem solving, 6) healthy coping and 7) risk reduction.9 Understanding these behaviors may have more influence on improving outcomes in the management of T2DM. T2DM patients need to understand their essential role in the management of their condition and health care providers must help them modify their behavior in order to prevent complications. It is estimated that as many as 80% of T2DM patients have knowledge deficits on how to manage their disease and they are four times more likely to develop complications.10 A search of the PubMed database did not reveal any published studies about the self-care behavior of Filipino patients.
The general objective of this study is to determine the level of adherence of T2DM patients to self-care recommendations: 1) healthy eating, 2) being active, 3) glucose monitoring, 4) medication adherence, 5) problem-solving, 6) healthy coping and 7) risk reduction. The specific objectives are: 1) to validate a questionnaire that can be used to determine the level of adherence to self-care behavior of T2DM Filipino patients and 2) to determine the level of adherence to self-care behaviors of T2DM patients in the Outpatient Department of the Philippine General Hospital using a validated questionnaire.
The AADE defines healthy eating as following an eating plan that includes not eating too much, counting the amount of carbohydrates consumed, not eating too much fat, drinking less alcohol and eating fruits, vegetables, whole grains and beans and other food with high fiber. Being active means the patient engages in jogging, cycling, gardening or walking without stopping for at least 150 minutes over at least three days per week, with no more than two consecutive days without physical activity.11 Self-monitoring of blood glucose refers to the process of consciously and voluntarily taking a daily reading from a glucose meter, understanding if the blood glucose value is within normal limits and connecting deviant readings to prior behavior like excess eating or intake of medications. Medication adherence refers to the compliance to the medications that have been prescribed by the physician for the treatment of T2DM. Problem solving is defined as the ability of the patient to generate a set of potential strategies for problem resolution. This includes when the patient makes a decision about what to eat or how much to eat, choose which medicines to take or decide to go for a walk. Hence, this means figuring out the problem and finding a way to deal with it. Healthy coping means that the patient tries to find ways to help deal with stress, strong emotions or family situations that can make it hard to manage T2DM affecting quality of life. This pertains to effective risk reduction behaviors such as smoking cessation and regular eye, foot and dental examinations, which maximize health and quality of life.
With the identification of the seven self-care behaviors proven to directly affect T2DM, the AADE developed the Behavior Score Instrument (BSI) to directly measure the patients’ behavior and identify priorities for change. The original English version of the BSI consists of 21 core questions – three questions for each of the seven self-care behaviors.
The first question deals with how often the patient practice the recommended behavior within a week, the second question deals with the importance of the behavior to the patient and the third question deals with how sure the patient is doing the recommended behavior. It was designed by AADE to support three main objectives: 1) to examine all areas of diabetes management in patients which is key to their success, 2) to provide the framework for how diabetes education and training are to be addressed in the practice setting and 3) to measure both patient progress and professional practice outcomes.12 All 21 questions are rated along ordinal scales. The BSI and its scoring system were obtained from AADE and an informal consent was granted to use it in the study for research purposes only.
The BSI was sent to University of the Philippines (UP) Manila – Sentro ng Wikang Filipino for translation to the local language. Two other native speakers who do not have knowledge of the original tool were requested to back-translate the Filipino version. Word changes in the questionnaire were done accordingly.
The Filipino version of the BSI was pilot tested on 10 T2DM patients in order to assess the degree to which a respondent’s understanding of each item matched the content that it was meant to elicit. Patients were asked to identify instructions which were hard to follow, questions which were difficult to understand and may require rephrasing and the level of difficulty encountered when answering each questions. Majority of the patients indicated that the BSI was not difficult to answer but several changes were made based on the feedback of the patients: 1) some phrases which are difficult to understand were simplified, 2) some statements at the beginning of each domain were rephrased or eliminated, and 3) the BSI format was modified into tabular form.
The modified BSI underwent quantitative validation following pilot testing. A sample of 98 patients were included, each responding to 21 items and achieving 80% power to detect the difference between the coefficient alpha under the null hypothesis of 0.70 and the coefficient alpha under the alternative hypothesis of 0.80 using a two-sided F-test with a significance level of 0.05. Also provided along with the modified BSI was a cover letter explaining the purpose of the study, the researcher’s contact information and a written assurance on the confidentiality of the answers. Internal consistency and reproducibility (test-retest reliability) were measured. Internal consistency determines the agreement of several questions to measure a single construct. In the study, it was determined using the Cronbach’s alpha within each domain, requiring a value of at least greater than 0.70 for it to be acceptable.13 Reproducibility was also tested by administering the modified BSI two weeks after through a phone call where questions were read verbatim and the patients were asked to give their answer. Twenty-five of the 98 patients who were not reached through phone call were not included in the study; instead, they were replaced. The differences in response between the first and second administration of the BSI were evaluated. Reproducibility was determined using the Cohen’s kappa coefficient.
This is a descriptive cross-sectional study. Diagnosed T2DM patients waiting for consultation at the General Medicine Clinic and Endocrinology Clinic were recruited to the study. Due to foreseen logistics constraints, convenience sampling was utilized. Eligible participants were clinic patients aged 18 years or older with a diagnosis of T2DM in their medical record. Patients were declared ineligible for the study if they are too ill (i.e., patients with >3 major diabetic complications) or cognitively impaired to participate. Major diabetic complications refer to coronary artery disease, peripheral arterial disease, diabetic nephropathy, diabetic neuropathy and diabetic retinopathy.
A total of 126 T2DM patients were included in the study. This sample size was required to determine the level of adherence among the patients assuming that percent adherence in the sample population is 20±8% with α=0.05 and power at 80. This was based on a study estimating that 80% of T2DM patients have knowledge deficits on how to manage their disease.10
Eligible patients waiting in line for consultation at the aforementioned clinics were approached and a description of the study was discussed. Those interested and who gave their consent were then given the modified BSI. They were asked to answer the questionnaire on their own but they were reassured that any questions could be addressed to the researcher immediately. Patients who did not consent to answer the modified BSI were not compelled to join the study.
Data were encoded and analysed using the STATA 12 program. The analysis was stratified by the level of adherence to each of the self-care behaviors. A corresponding score of 1-3 was given to the answers to every question based on the original tool. The average of the scores in every self-behavior domain was computed. An average of 1-1.499 was considered poor adherence, 1.5-2.499 was considered fair adherence and 2.5-3 was considered good adherence in a particular domain. The overall score was computed by getting the mean of the average score in each domain and was interpreted in the same way as in the individual self-care behavior domains.
The details of the study were discussed by the researcher with each of the prospective participants. Eligible patients were not coerced in any way to participate. Patients were only included upon giving consent. The anonymity of participants, as well as the confidentiality of the data obtained, was assured by the researcher. The study was submitted to and was approved by the UP Manila Ethics Review Board (UPMREB-2012-0346-P1).
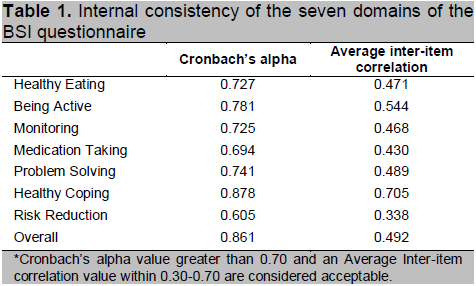
A total of 98 patients were included for validation. Majority of the participants were females (61.2%), high school graduates (41.9%), unemployed (66.3%) and take at least two medications for diabetes (41.8%). Validity was tested based on internal consistency and reproducibility. Internal consistency was measured by measuring the value of Cronbach’s alpha in each of the seven self-care behavior domains (Table 1). Majority of the domains had acceptable values of greater than 0.70 except for medication taking (0.694) and risk reduction (0.605). In the medication taking domain, reversed questioning could probably be the reason for the lower Cronbach’s alpha value. Instead of being asked how frequently the participants take their medications, they were asked how frequently they missed those medications. In constructs where Cronbach’s alpha values are expected to deviate negatively, a value of greater than 0.50 is considered a sign of acceptable internal consistency.14 Hence, even with the relatively lower Cronbach’s alpha value, the researcher opted not to modify the question since reverse questioning also reduces response bias.15 Similarly, in the risk reduction domain, the questions require recall of events within the year compared to the other domains that only require recall of events within the previous week. Therefore, the questions were not modified as well, even with the low Cronbach’s alpha value. The average inter-item correlation measures the correlation between an item and the rest of the questions in each domain requiring values between 0.30-0.70 in order to be acceptable, which means that each of the items measure different entities and are not redundant. The modified BSI revealed a satisfactory overall Cronbach’s alpha of 0.861 and an acceptable average inter-item correlation of 0.492. Considering the educational attainment of the participants as well as the high overall Cronbach’s alpha, the two domains with relatively lower values were still included in the study questionnaire without any revisions.
Click here to download Table 1
Table 1. Internal consistency of the seven domains of the BSI questionnaire
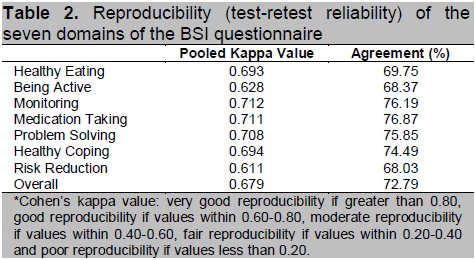
The overall Cohen’s kappa coefficient for reproducibility of the BSI was “good” (0.679, 72.79% agreement). Out of the 21 items, five had very good reproducibility (>0.80), nine had good reproducibility (0.60-0.80), six had moderate reproducibility (0.40-0.60) and the rest had fair reproducibility. None of the domains had poor agreement (Table 2). Since the modified BSI was found to have acceptable internal consistency and reproducibility based on the computed Cronbach’s alpha and Cohen’s kappa coefficient, the actual data collection for the study proceeded without major revisions on the tool.
Click here to download Table2
Table 2. Reproducibility (test-retest reliability) of the seven domains of the BSI questionnaire
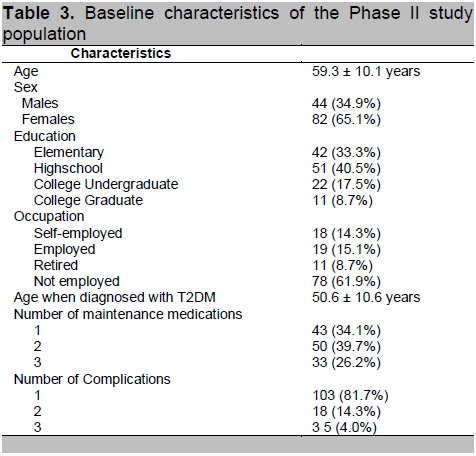
A total of 126 patients were included in the study. The participants from the validation testing were included. The overall demographic characteristics are summarized in Table 3. Majority of the participants were females (65.1%). This could be explained by the fact that T2DM is more prevalent in Filipino females.16 The study population distribution according to education and occupation indicated that a high proportion of patients belonged to the lower socioeconomic status, which is expected in a public tertiary hospital. The mean age was 59.3 ± 10.1 years while the mean age of diagnosis was 50.6 ± 10.6 years. In a recent national study, it was found that the mean age of onset of diabetes in Filipinos is 52.2 ± 11.3 years, 17 which is consistent with the present study. Most of the participants reported having only one diabetic complication, the majority involving the eye, strengthening the popular belief that vision loss is the most feared complication of diabetes. 18
Click here to download Table 3
Table 3. Baseline characteristics of the Phase II study population
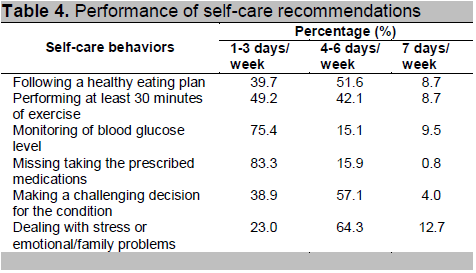
Eighty-three percent of the participants were found to be compliant to medications with minimal deviations from their regimen. In all other domains, less than 10% of the patients adhere to self-care recommendations daily. Majority of the participants follow healthy coping (64.3%), problem-solving (57.1%), healthy diet (51.6%) and active lifestyle (42.1%) four to six times a week (Table 4). Monitoring of blood glucose was the least followed recommendation with 75.4% taking their blood glucose level only once to thrice a week. This is probably because 1) only a minority of participants are using insulin, requiring daily glucose monitoring, 2) many of the participants are in the low socioeconomic status, 3) many participants do not own a blood glucose meter and 4) many of the participants are not properly advised by their physician.
Click here to download Table 4
Table 4. Performance of self-care recommendations
Majority of the patients were able to have blood pressure monitoring (92.1%), lipid profile check (77.8%) and an eye examination (68.3%) within the previous year (Table 5). Eighty-four (66.7%) of the participants were non-smokers contributing to the large proportion of participants who do not smoke at present (88.1%). However, there was note of low compliance to foot care (37.3%), dental care (27.8%) and vaccination (15.9%).
Click here to download Table 5
Table 5. Performance of risk reduction

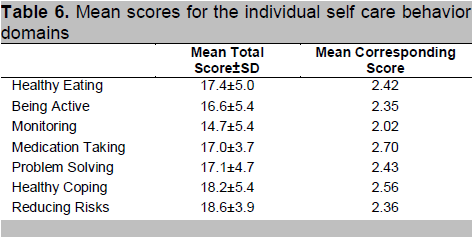
Each domain has a total of 27 points divided into three major questions: frequency of adherence (7 points), importance (10 points) and surety of compliance (10 points). In all domains, the importance of following the recommended behavior received the highest total points (mean =7.38) while frequency has a mean of 3.52 and surety of doing the behavior has a mean of 6.18 (Table 6). These points have their corresponding scores in order to determine the level of adherence.
Click here to download Table 6
Table 6. Mean scores for the individual self care behavior domains
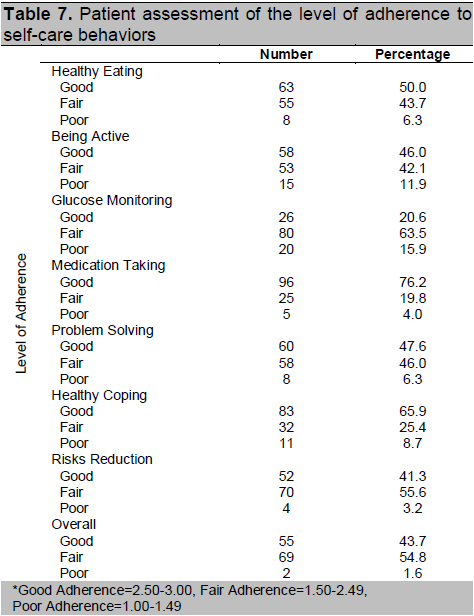
Majority of the participants have good adherence in five of the seven identified self-care behaviors: medication taking (76.2%), healthy coping (65.9%), healthy eating (50.0%), problem solving (47.6%) and being active (46.0%). In terms of glucose monitoring and risks reduction, 63.5% and 55.6% of the participants have fair adherence respectively. Overall, 43.7% have good compliance to the self-care behaviors while 54.8% and 1.6% have fair and poor compliance respectively (Table 7).
Click here to download Table 7
Table 7. Patient assessment of the level of adherence to self-care behaviors
Half of the participants have good adherence to healthy eating. Most reported not eating too much while consuming more fruits and vegetables. More than half of the patients reported following a healthy eating plan just 4-6 times a week, with some allotting one diet-free day a week. Healthy eating is an integral part of diabetes self-care because it improves blood glucose levels, lipid profile and blood pressure.19 HbA1c was found to significantly decrease in patients receiving intensive dietary advice compared to those receiving just the standard of care.20 Hence, adherence to healthy eating, preferably as advised by a physician or a dietitian, should be emphasized to T2DM patients.
Exercise, when done on a regular basis, improves lipid and glycemic control, increases insulin sensitivity and contributes to the maintenance of blood pressure, reducing the risk for T2DM complications. It is also the only intervention found to directly affect cardiorespiratory fitness while reducing the risk for cardiovascular disease.21 The current study found that majority of T2DM patients have good adherence to an active lifestyle. But since most of the participants were elderly, the usual form of activity reported was brisk walking. This is contrary to previous studies stating that T2DM patients tend to be less likely to engage in physical activities22 and that it is an underused therapy in the medical care of T2DM.23 However, it should be noted that the results of the current study are based on self-report of a non-structured exercise intervention. In a systematic review done by Kavookjian et al.,11 it is the structured exercise intervention that improves cardiovascular outcomes than non-structured interventions like brisk walking. There is no discrete exercise regimen that can be generalized to T2DM patients since it should be tailored individually according to person’s needs, priorities and capabilities.
Self-monitoring of blood glucose is actually a patient-centered control process of consciously and voluntarily managing T2DM which involves not only taking a reading from a glucose meter but also understanding if the blood glucose value is within normal limits, connecting deviant readings from prior behavior like eating or intake of medications, implementing an action plan for blood glucose control and giving less weight to subjective feelings like dizziness. In the current study, majority of the participants were classified as having fair adherence to glucose monitoring (63.5%). The participants find it important to monitor blood glucose levels (mean points=7.0, mean score=2.54) though they are not sure that it would be done (mean points=5.27, mean score=2.04). More than 75% of the participants monitor their blood sugar less than thrice a week. This could be because only about 26.2% of the participants are insulin-requiring necessitating daily monitoring. In a systematic review done by McAndrew et al.,24 no existing studies support that glucose monitoring improves the control of blood glucose levels among T2DM patients not using insulin. Still, this should not stop patients from self-monitoring their blood glucose levels at key pre-determined times because patients adjusting their treatment and self-care behavior accordingly were found to have improvement in their HbA1c levels by 0.25%.25,26
In the current study, results showed good adherence to medication taking (76.2%). Though this is a respectable figure, the results are based on self-reports of patients seeking consult in the outpatient department. In a study done by Mason et al.,27 there was note of discrepancy in the adherence among T2DM patients taking oral hyperglycemic agents, where 75.4% were adherent based on electronic monitoring compared to 92.4% based on self-report. Since adherence to the treatment medications is a worldwide problem and is primarily related to the simplicity of the regimen, severity of T2DM and the possible consequences of missed doses, patient education and counseling should be emphasized. Specific interventions to improve this behavior still need further studies.28
Problem solving is defined as “a learned behavior that includes generating a set of potential strategies for problem resolution, selecting the most appropriate strategy, applying the strategy and evaluating the effectiveness of the strategy.”29 Though problem solving was identified as the most difficult behavior to teach T2DM patients,30 the current study found that majority of participants have fair to good adherence (93.6%) to problem solving. Many of the participants claim that they are used to the demands of diabetes, making it easy to make decisions. Because of this, the study cannot conclude if the participants effectively solve their problems. In a systematic review, patients receiving group sessions of problem-oriented therapy have decreased HbA1c and total cholesterol levels.31 In the local setting, further studies to determine correlation between problem solving and blood sugar levels should be undertaken because there is no current standardized tool to assess problem solving in T2DM is available.
Healthy coping is defined as “responding to a psychological and physical challenge by recruiting available resources to increase the probability of favorable outcomes in the future.”32 It is a substantial continuing rather than occasional behavior in T2DM management.33 Emotional factors such as depression, motivational factors, poor communication and low socioeconomic status compromises adherence.34 In the current study, there is reported good adherence to healthy coping (65.9%). This can be probably attributed to the strong family ties of Filipinos. Filipinos, being family-centric, tend to cope with illness through the help of family and friends.35 They typically hold to the idea that ill persons should not live physically and financially apart from their families.36
In the current study, it was found that there was poor adherence to foot care, dental care and vaccinations. One potential reason for this is that patients were not educated regarding these preventive measures. Another possibility is that physicians do not provide advice on these practices until patients report symptoms. The current study therefore suggests that more attention be given to these aspects of care.
The current study found that T2DM patients in the Philippine General Hospital have fair adherence to the seven self-care behaviors. This calls for further improvement to maximize their benefits, hence, the following recommendations: 1) T2DM patients should receive intensive dietary advice either from their physician or a dietitian, 2) Structured exercise intervention should be individually tailored for every patient, 3) Patients should be taught how to adjust specific behaviors depending on the blood glucose monitoring, 4) Families of diabetic patients should be involved in the treatment process, 5) Regular foot check-up, dental check-up and regular influenza and pneumococcal vaccinations should be offered to all T2DM patients, together with yearly eye examination, regular blood pressure and lipid monitoring and smoking cessation, and 6) Efforts to constantly remind and educate patients on the need to consistently adhere to these behaviors to improve diabetes should be observed.
In the modified BSI, it is recommended to remove or modify certain parameters based on the patients’ clinical profile. For instance, patients should be classified as those who are insulin-requiring and those who are not. There should be a separate scoring between these two groups especially in the blood glucose monitoring domain. This will make the stratification more accurate.
Further studies are also deemed necessary on the objective methods of measuring certain domains like medication adherence and problem solving. Being able to measure these behaviors objectively may help health care providers better educate T2DM patients.
1. Tan DA. Changing disease trends in the Asia-Pacific. Climacteric. 2011; 14(5):529-534.
2. Wild S, Roglic G, Green A, Sicree R, King H. Global Prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care. 2004; 27:1047–1053.
3. Food & Nutrition Research Institute – Department of Science and Technology (FNRI-DOST). Philippine Nutrition Facts & Figures 2008.
4. Department of Health – Division of Public Health Surveillance & Informatics Division. Field Health Services Information System (DOH-FHSIS) 2009.
5. Ismail-Beigi F. Pathogenesis and glycemic management of Type 2 Diabetes Mellitus: A physiological Approach. Archives of Iranian Medicine. 2012; 15(4):239-246.
6. American Diabetes Association. Standards of Medical Care in Diabetes. Diabetes Care. 2013; 36(1):S11-S66.
7. Nathan DM,Buse JB,Davidson MB,Heine RJ,Holman RR,Sherwin R, Zinman B. Management of hyperglycemia in type 2 diabetes: A consensus algorithm for the initiation and adjustment of therapy: A consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2006; 29(8):1963-1972.
8. Del Prato S, Penno G, Miccoli R. Changing the treatment paradigm for Type 2 diabetes. Diabetes Care. 2009; 32:217-222.
9. Boren SA. AADE7 self-care behaviors: Systematic reviews. The Diabetes Educator. 2007; 33(6):866-871.
10. Boren SA, Gunlock TL, Schaefer J, Albright A. Reducing risks in diabetes self-management: A systematic review of literature. The Diabetes Educator. 2007; 33(6): 1053-1077.
11. Kavookjian J, Elswick BM, Whetsel T. Interventions for being active among individuals with diabetes: A systematic review of the literature. The Diabetes Educator. 2007; 33: 962-988.
12. American Association of Diabetes Educators. Using the Behavior Score Dashboard from http://www.diabeteseducator.org, 2011.
13. Peyrot M, Peeples M, Tomky D, Charron-Prochownik D, Weaver T. Development of the American Association of Diabetes Educators’ Diabetes self-management assessment report tool. The Diabetes Educator. 2007; 33:818.
14. Bowling A. Research Methods in Health. In Investigating health and health services. Second edition. Buckingham: Open University Press, 2002.
15. Field AP. Discovering statistics using SPSS 2nd edition. London: Sage, 2005.
16. Baltazar JC, Ancheta AC, Aban IB. Prevalence and correlates of diabetes mellitus and impaired glucose tolerance among adults in Luzon, Philippines. Diabetes Research and Clinical Practice. 2004; 64:107-115.
17. Jimeno CA, Sobrepena LM, Mirasol RC. DiabCare 2008: Survey on glycaemic control and the status of diabetes care and complications among patients with type 2 diabetes mellitus in the Philippines. Philippine Journal of Internal Medicine. 2012; 50(1): 15-22.
18. Euala K, Schneiderman J (Novartis Pharmaceuticals Canada Inc.). Angus Reid Vision Critical poll. December 2011.
19. Povey RC, Clark-Carter D. Diabetes and healthy eating: A systematic review of literature. The Diabetes Educator. 2007; 33(6):931-959.
20. Perry TL, Mann JI, Lewis-Barned NJ, Duncan AW, Waldron MA, Thompson C. Lifestyle intervention in people with insulin-dependent diabetes mellitus (IDDM). European Journal of Clinical Nutrition. 1997; 51:757-763.
21. Boule N, Kenny G, Haddad E, Wells G, Sigal R. Meta-analysis of the effect of structured exercise training on cardiorespiratory fitness in type 2 diabetes mellitus. Diabetologia 2003; 46:1071-1081.
22. Boyle R, O’Connor P, Pronk N, Tan A. Stages of Change for physical activity, diet and smoking among HMO members with chronic conditions. American Journal of Health Promotion. 1998; 12(1):25-30.
23. Albright A, Franz M, Hornsby G. American College of Sports Medicine position stand: Exercise and type 2 Diabetes. Medicine & Science in Sports & Exercise. 2000; 32(7):1345-1360.
24. McAndrew L, Schneider SH, Burns E, Leventhal H. Does patient blood glucose monitoring improve diabetes control?: A systematic review of literature. The Diabetes Educator 2007; 33(6):991-1011.
25. Farmer AJ, Perera R, Ward A. Metaanalysis of individual patient data in randomized trials of self-monitoring of blood glucose in people with non-insulin treated type 2 diabetes. British Medical Journal. 2012; 344:e486.
26. Schwedes U, Siebolds M, Mertes G, Group SS. Meal-related structured self-monitoring of blood glucose: Effect on diabetes control in non-insulin-treated type 2 diabetic patients. Diabetes Care 2002; 25:1928-1932.
27. Mason BJ, Matsuyama JR, Jue SG. Assessment of sulfonylurea adherence and metabolic control. Diabetes Educator. 1995; 21:52–57.
28. Odegard PS, Capoccia K. Medication taking and diabetes: A systematic review of literature. The Diabetes Educator. 2007; 33(6):1014-1029.
29. Mulcahy K, Maryniuk M, Peeples M. Diabetes Self-management education core outcomes measures. Diabetes Education. 2003; 29:768-784.
30. Bonnet C, Gagnayre R, d’Ivernois JF. Learning difficulties of diabetic patients: A survey of educators. Patient Education and Counseling. 1998; 35:139-147.
31. Hill-Briggs F, Gemmell L. Problem Solving in Diabetes Self-management and Control: A systematic review of literature. The Diabetes Educator. 2007; 33(6):1032-1150.
32. Kent D, et al. Healthy coping: Issues and implications in diabetes education and care. Population Health Management. 2010; 13(5):227-233.
33. Beeney L, Bakry A, Dunn S. Patient psychological and information needs when the diagnosis is diabetes. Patient Education and Counseling. 1996; 29(1):109-116.
34. Rubin R. Adherence to pharmacologic therapy in patients with Type 2 diabetes mellitus. American Journal of Medicine. 2005; 18(suppl 5A):27S-34S.
35. Aguilar F. Filipinos in global migrations: At home in the world? Philippine Social Science Council. 2002.
36. Oka Y. Self-reliance in interdependent communities: Independent living of disabled persons in the Asia-Pacific region. http://www.independentliving.org/LibArt/oka.html. 1988Tables