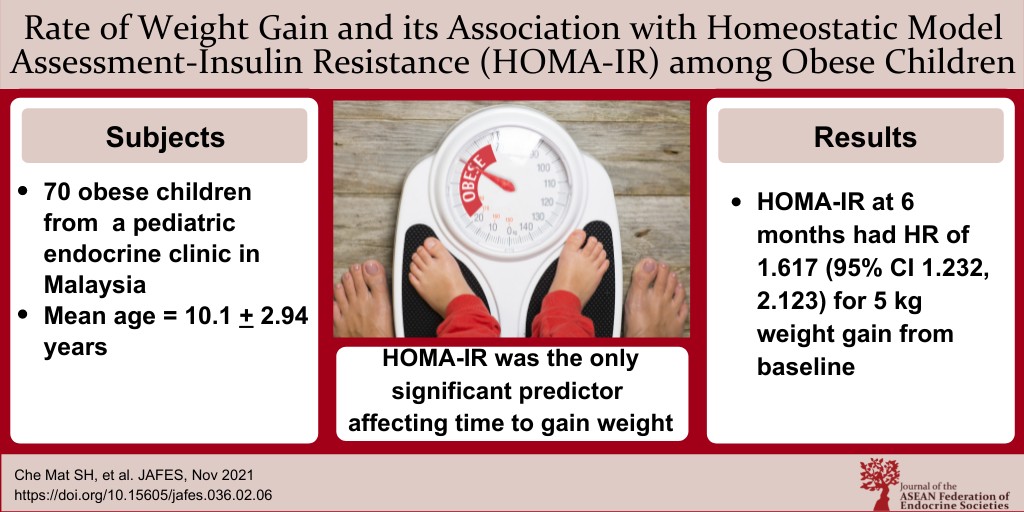
Rate of Weight Gain and its Association with Homeostatic Model Assessment-Insulin Resistance (HOMA-IR) among Obese Children attending Paediatric Endocrine Clinic, Hospital Universiti Sains Malaysia
DOI:
https://doi.org/10.15605/jafes.036.02.06Keywords:
HOMA-IR, prognostic factor, obesity, insulin resistanceAbstract
Objective. We aimed to study the median time to gain weight from baseline and factors that were associated with rate of weight gain among obese children attending pediatric endocrine clinic Hospital USM.
Methodology. We recruited 70 participants with the mean age of 10.1 + 2.94 years with exogenous or simple form of obesity from June 2019 until September 2020. We analyzed their demography (age, gender, ethnicity, family background), measured their anthropometry (weight, height, BMI) and monitored monthly weight increment and finally analyzed their HOMA-IR at baseline and after 6 months of follow up.
Results. The mean time to gain 5 kg from baseline was 16 weeks (95% CI): (15.2, 16.7). Multivariate analysis showed only HOMA-IR after 6 months was a significant predictor affecting time to gain 5 kg; Adjusted HR: (95%CI) 1.617(1.232, 2.123), (p=0.001).
Conclusion. The time to gain 5 kg from baseline weight was increased 1.6 times in the presence of insulin resistance at 6 months follow up in patients with obesity. More intensive education and closed follow-up are recommended for children with obesity.
Downloads
References
Dietz WH. Overweight in children and adolescence. N Engl J Med. 2004;350(9), 855-7. https://pubmed.ncbi.nlm.nih.gov/14985480. https://doi.org/1056/NEJMp048008.
Wang Y, Lim H. The global childhood obesity epidemic and the association between socio-economic status and childhood obesity. Int Rev Psychiatry. 2012;24(3):176-88. https://pubmed.ncbi.nlm.nih.gov/22724639.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4561623. https://doi.org/10.3109/09540261.2012.688195.
De Onis M, Blössner M, Borghi E. Global prevalence and trends of overweight and obesity among preschool children. Am J Clin Nutr. 1992;92(5):1257-64. https://pubmed.ncbi.nlm.nih.gov/20861173. https://doi.org/10.3945/ajcn.2010.29786.
World Health Organization. Regional Office for the Western Pacific. The Asia-Pacific perspective: Redefining obesity and its treatment. Sydney: Health Communications Australia. https://apps.who.int/iris/handle/10665/206936.
Ten S, Maclaren N. Insulin resistance syndrome in children. J Clin Endocrinol Metab. 2004;89(6):2526-39. https://pubmed.ncbi.nlm.nih.gov/15181020.
https://doi.org/10.1210/jc.2004-0276.
Keskin M, Kurtoglu S, Kendirci M, Atabek ME, Yazici C. Homeostasis model assessment is more reliable than the fasting glucose/insulin ratio and quantitative insulin sensitivity check index for assessing insulin resistance among obese children and adolescence. Pediatrics. 2005;115(4):e500-3. https://pubmed.ncbi.nlm.nih.gov/15741351. https://doi.org/10.1542/peds.2004-1921.
Chang-Rueda C, Cañas-Urbina A, Trujillo-Murillo K, et al. Correlation of HOMA-IR with BMI-for-age percentile in children and adolescent from the Soconusco region of Chiapas, Mexico. Rev Fac Med. 2019:67(4):635-8. https://doi.org/10.15446/revfacmed.v67n4.67159.
Peplies J, Börnhorst C, Günther K, et al. Longitudinal association of lifestyle factors and weight status with insulin resistance (HOMA-IR) in preadolescent chidren. Int J Beh Nutr Phys Act. 2016;13(1):97. https://pubmed.ncbi.nlm.nih.gov/27590045.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5009569. https://doi.org/10.1186/s12966-016-0424-4.
Ismail MN, Chee SS, Nawawi H, Yusoff K, Lim TO, James WPT. Obesity in Malaysia. Obesity Reviews. 2002;3(3):203-8. https://doi.org/10.1046/j.1467-789X.2002.00074.x.
Kasmini K, Idris MN, Fatimah A, Hanafiah S, Iran H, Bee MNA. Prevalence of overweight and obese school children aged between 7 to 16 years amongst the major 3 ethnic groups in Kuala Lumpur, Malaysia. Asia Pac J Clin Nutr. 1997;6(3):172-4. https://pubmed.ncbi.nlm.nih.gov/24394759.
Ho TF, Chay SO, Yip WC, Tay JS, Wong HB. The prevalence of obesity in Singapore primary school children. Aust Paediatr J. 1983;19(4):248-50. https://pubmed.ncbi.nlm.nih.gov/6673725. https://doi.org/10.1111/j.1440-1754.1983.tb02113.x.
Liu W, Liu W, Lin R, et al. Socioeconomic determinants of childhood obesity among primary school children in Guangzhou, China. BMC Public Health. 2016;16:482. https://pubmed.ncbi.nlm.nih.gov/27277601. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4898378. https://doi.org/10.1186/s12889-016-3171-1.
Karimollah Hajian-Tilaki, Behzad Heidari. Childhood obesity, overweight, socio-demographic and life style determinants among preschool children in Babol, Northern Iran. Iran J Public Health. 2013; 42(11):1283-91. https://pubmed.ncbi.nlm.nih.gov/26171341. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4499070.
Alagappan M, Rampal L, Zalilah MS. Prevalence of overweight/obesity and its associated factors among secondary school students in semi urban area in Malaysia. Med J Malaysia. 2019;74(6):513-20. https://pubmed.ncbi.nlm.nih.gov/31929478.
Mathialagan A, Nallasamy N, Razali SN. Physical activity and media environment as antecedents of childhood obesity in. Asian J Pharm Clin Res. 2018;11(9):287-92. https://doi.org/10.22159/ajpcr.2018.v11i9.17095.
Nurul Izzah A, Nadia M, Wan Rozita WM, Tengku Rozaina TM, Rafiza S, Lokman Hakim S. The prevalence of overweight and obesity and its association factors among Malays’ Adolescents: Findings from seafood consumption survey in Peninsular Malaysia. J Childhood Obes. 2019; 4:2. https://childhood-obesity.imedpub.com/the-prevalence-of-overweight-and-obesity-and-its-association-factors-among-malays-adolescents-findings-from-seafood-consumption-su.pdf.
Obesity: The prevention, identification, assessment and management of overweight and obesity in adult and children [Internet]. Centre for Public Health Excellence at NICE (UK); National Collaborating Centre for Primary Care (UK). London: National Institute for Health and Clinical Excellence (UK); 2006 Dec.National Institute for Health and Clinical Excellence: Guidance. https://pubmed.ncbi.nlm.nih.gov/22497033. Bookshelf ID: NBK63696.
Coppock JH, Ridolfi DR, Hayes JF, St Paul M, Wilfley DE. Current approaches to the management of pediatric overweight and obesity. Curr Treat Options Cardiovasc Med. 2014;16(11):343. https://pubmed.ncbi.nlm.nih.gov/25205083. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4418422. https://doi.org/10.1007/s11936-014-0343-0.
Kim K, Hong S, Kim EY. Reference values of skeletal muscle mass for Korean children and adolescents using data from the Korean National Health and Nutrition Examination Survey 2009-2011. PLOS ONE. 2016;11(4):e0153383. https://pubmed.ncbi.nlm.nih.gov/27073844. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4830599. https://doi.org/10.1371/journal.pone.0153383.
Wei C, Ford S, Hunt L, Crowne EC, Shield JPH. Abnormal liver function in children with metabolic syndrome from a UK based obesity clinic. Arch Dis Child. 2011;96(11):1003-7. https://pubmed.ncbi.nlm.nih.gov/21097793. https://doi.org/10.1136/adc.2010.190975.
Tock L, Prado WL, Caranti DA, et al. Nonalcoholic fatty liver disease decreases in obese adolescents after multidisciplinary therapy. Eur J Gastroenterol Hepatol. 2006;18(12):1241-5. https://pubmed.ncbi.nlm.nih.gov/17099371. https://doi.org/10.1097/01.meg.0000243872.86949.95.
Odeleye OE, de Courten M, Pettitt DJ, Ravussin E. Fasting hyperinsulinemia is a predictor of increased body weight gain and obesity in Pima Indian children. Diabetes. 1997;46(8):1341-5. https://pubmed.ncbi.nlm.nih.gov/9231660. https://doi.org/10.2337/diab.46.8.1341.
Maffeis C, Moghetti P, Grezzani A, Clementi M, Gaudino R, Tatò L. Insulin resistance and the persistence of obesity from childhood into adulthood. J Clin Endocrinol Metab. 2002;87(1):71-6. https://pubmed.ncbi.nlm.nih.gov/11788625. https://doi.org/10.1210/jcem.87.1.8130.
Hardy OT, Czech MP, Corvera S. What causes the insulin resistance underlying obesity? Curr Opin Endocrinol Diabetes Obes. 2012;19(2):81-7. https://pubmed.ncbi.nlm.nih.gov/22327367. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4038351. https://doi.org/10.1097/MED.0b013e3283514e13.
Published
How to Cite
Issue
Section
License
Copyright (c) 2021 Siti Hasmiza Che Mat, Najib Majdi Yaacob, Suhaimi Hussain

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The full license is at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.