In the past few decades, there has been a progressive increase in the prevalence of young-onset type 2 diabetes (T2DM). T2DM was once considered a disease of older adults but the age of diagnosis is dropping and it is now increasingly diagnosed in adolescents and young adults.[1] The SEARCH for Diabetes in Youth Study highlighted the burden of DM in the youth in the United States of America while the Treatment Options for Type 2 Diabetes in Adolescents and Youth (TODAY) study illustrated the difficulty in achieving and maintaining a good glycaemic control in young-onset T2DM.[2][3] In clinical practice, a diagnosis of T2DM as opposed to type 1 diabetes (T1DM) in a young adult was often perceived as the milder form of diabetes by both the health care providers and the patients.[1][4] Thus, traditionally the focus of research of diabetes in young adults has been on T1DM.
Young-onset T2DM patients are predisposed to increased risk of complications at a younger age. Previous studies showed that young-onset T2DM was associated with more unfavourable cardiovascular risk factors, more aggressive phenotype with more complications and greater mortality when compared with T1DM.[4][5] This is a pilot study conducted in Malaysia with the objectives of comparing the prevalence of diabetic complications in young-onset T2DM with T1DM patients in a tertiary health care institution and to examine the relationship between the diabetic complications with various clinical and metabolic parameters.
METHODOLOGYThis was a retrospective, cross-sectional comparative study conducted at Selayang Hospital, a tertiary health care institution in the state of Selangor. Electronic medical records of all diabetic patients who were seen at the diabetes or medical clinic from January to June 2015 were reviewed retrospectively. The consecutive sampling was conducted over a six-month period in order to capture all active diabetic patients being treated at our hospital at three to six-monthly intervals. These patients were generally referred from primary or secondary care health facilities in the surrounding districts for optimisation of glycaemic control along with management of other cardiovascular risk factors and diabetic complications.
Young-onset T2DM patients were defined as those diagnosed as T2DM before 40 years old. They were differentiated from T1DM by the presence of the following: insidious disease onset, family history of T2DM, obesity, signs of insulin resistance such as acanthosis nigricans and other metabolic conditions commonly associated with T2DM including hypertension, dyslipidemia or polycystic ovarian syndrome.
T1DM patients were those diagnosed clinically as T1DM e.g., presence of diabetic ketoacidosis without significant precipitant, absence of acanthosis nigricans associated with T2DM with or without documented positive insulin autoantibodies. Exclusion criteria were patients given a clinical diagnosis of latent autoimmune diabetes of adults, monogenic diabetes mellitus, e.g., maturity onset diabetes of the young and secondary diabetes. This study was approved by Malaysia Medical Research and Ethics Committee and was done in adherence to the Helsinki Guidelines. Patient consent was not required because our study was retrospective and used deidentified data.
For each patient, data on demographic, anthropometry, clinical history, and laboratory biochemistry including glycated hemoglobin (HbA1c), lipid profile and renal function were collected. Associated cardiovascular risk factors including smoking, hypertension, dyslipidemia as well as their treatment were ascertained. Hypertension was defined as blood pressure ≥140/90 mmHg or on antihypertensive treatment. Dyslipidemia was defined as low density lipoprotein (LDL) ≥2.6 mmol/L, fasting triglyceride ≥1.7 mmol/L, high density lipoprotein (HDL) ≤1.0 mmol/L for males and ≤1.3 mmol/L for females or on lipid lowering therapy. Overweight or obesity was defined by a body mass index (BMI) of ≥23 kg/m2 or waist circumference (WC) ≥90 cm for males and ≥80 cm in females. Adherence to medications, dietary modification and exercise were classified subjectively into good, fair, suboptimal or poor based on the documentation in the medical records of the last clinic visit.
Diabetic complications assessments involved elucidation of microvascular (retinopathy, nephropathy and neuropathy) and macrovascular (ischemic heart disease, stroke and peripheral vascular disease) complications. Diabetic retinopathy assessment was based on serial ophthalmological findings by ophthalmologists at the ophthalmology clinic. Diabetic nephropathy was defined by the presence of persistent microalbuminuria or macroscopic proteinuria or impaired renal function not explained by other renal pathology. A urine albumin creatinine ratio (ACR) of 2.5 to 30.0 mg/mmol in males and 3.5 to 30.0 mg/mmol in females were considered microalbuminuric.[6] Proteinuria was determined by a urine dipstick of one plus or more. Renal function was evaluated by estimated glomerular filtration rate (eGFR) using the Modification of Diet in Renal Disease (MDRD) formula. Peripheral neuropathy was determined based on the presence of sensory symptoms and/or objective physical findings on neurological examination. Ischemic heart disease was defined as the presence of history of myocardial infarction, angina or previous coronary revascularization. Stroke was defined as history of ischemic or hemorrhagic stroke proven on a computed tomography (CT) of the brain or history of transient ischemic attack. Peripheral vascular disease was defined as history of intermittent claudication with anklebrachial index <0.9, previous lower limb revascularization or amputation for ischemia. In order to examine the occurrence of diabetic complications in relation to the onset of diabetes, we stratified them into two categories, i.e., before or within the first five years or more than five years after the diagnosis of diabetes. All parameters were derived from the latest clinic visit.
Statistical AnalysisAll statistical analyses were performed using the Statistical Package for Social Science version 19.0 for Windows (SPSS Incorporation, Chicago, Illinois, USA). Numerical values were expressed as mean±standard deviations (SD). Categorical data were expressed as percentage. Group means were compared with Student's t test or the Mann Whitney U test where appropriate. Categorical variables were compared using χ2 test or Fisher’s exact test. To examine the association between various clinical and metabolic parameters with the occurrence of microvascular and macrovascular complications, univariate followed by stepwise regression analyses were performed. The variables included in the regression analyses were type of diabetes; age; disease duration; gender; ethnicity; smoking status; adherence to medications, dietary modification and exercise; hypertension; systolic blood pressure (SBP); HbA1c; dyslipidemia; total cholesterol; HDL level; LDL level; triglyceride level; BMI and WC. A p value of ≤0.05 was considered statistically significant.
Subject Characteristics
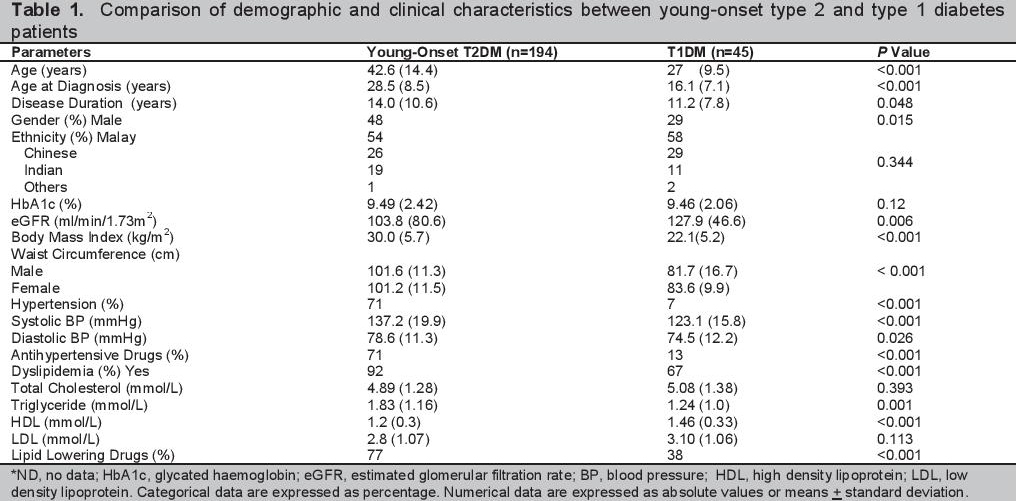
There were 194 young-onset T2DM and 45 T1DM subjects (Table 1). The young-onset T2DM subjects were older in age and had slightly longer duration of disease compared to the T1DM subjects. The mean age of diabetes onset for young-onset T2DM and T1DM was 28.5+8.5 and 16.1+7.1 years (p<0.001) respectively. There was an excess of females, particularly in the T1DM cohort (71% vs 52%, p<0.05). There was no significant difference in ethnic distribution between the two groups. Majority (79%) of the young-onset T2DM patients had family history of diabetes. There was no significant difference in HbA1c between the two groups.
Click here to download Table 1Table 1. Comparison of demographic and clinical characteristics between young-onset type 2 and type 1 diabetes patients
Cardiovascular Risk Factors
Young-onset T2DM subjects were more likely to have unfavourable cardiovascular risk factors compared with T1DM. These included the presence of hypertension (71% vs 7%, p<0.001), dyslipidemia (92% vs 67%, p<0.001), overweight or obesity (98% vs.55%, p<0.001). Among the young-onset T2DM subjects who were overweight or obese, 83% had the condition before or within the first five years of diagnosis of DM. The mean BMI for young-onset T2DM subjects was 30.0±5.7 kg/m2 compared to 22.1±5.2 kg/m2 among the T1DM subjects. Both systolic and diastolic blood pressures were significantly higher among the young-onset T2DM subjects despite being treated with antihypertensive drugs. The young-onset T2DM group also had significantly higher triglyceride and lower HDL levels, although 77% of them were already treated with lipid lowering drugs compared to only 38% in T1DM. Similarly, 64% of the young-onset T2DM subjects with hypertension or dyslipidemia already had the risk factors present before or within the first five years of diagnosis of diabetes.
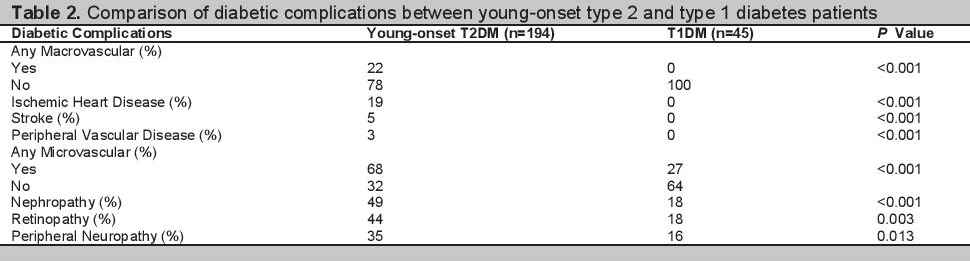
Diabetic ComplicationsDespite similar glycaemic profile, significantly more subjects in the young-onset T2DM group developed macrovascular and microvascular complications than the T1DM group (22% vs 0%, p<0.001 for macrovascular, 68% vs.27%, p<0.001 for microvascular) (Table 2). The differences between the two groups were homogeneous for each individual macrovascular and microvascular complications. The onset of complications appeared to be earlier among the young-onset T2DM subjects. Among the 132 young-onset T2DM subjects who developed diabetic complications, 33% had the complications before or within the first 5 years of diagnosis of DM. As for the 12 T1DM subjects who developed microvascular complications, only 1 subject (8%) was affected within the first 5 years of diagnosis of DM.
Click here to download Table 2Table 2. Comparison of diabetic complications between young-onset type 2 and type 1 diabetes patients
Association between clinical or metabolic parameters and diabetic complications
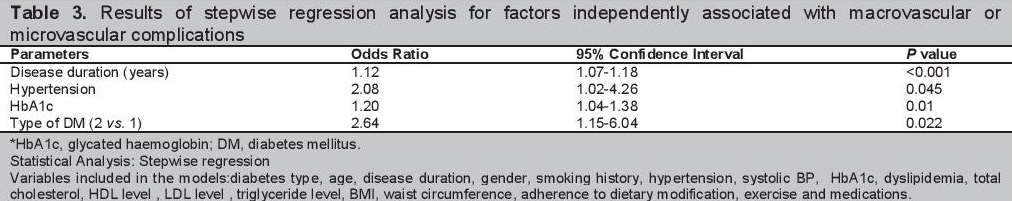
Univariate regression analysis revealed a significant association between age, diabetes duration, types of diabetes, presence of hypertension, dyslipidemia, HbA1c, systolic BP and triglyceride level with diabetic complications. Stepwise regression analysis conducted to look for independent association between the clinical or metabolic parameters with diabetic complications revealed that being diagnosed with young-onset T2DM instead of T1DM, the presence of hypertension, a raised HbA1c and having longer duration of disease were independently associated with increased risk of diabetic complications (Table 3). Being diagnosed with young-onset T2DM as opposed to T1DM carried the highest odds ratio of 2.64.
Click here to download Table 3Table 3. Results of stepwise regression analysis for factors independently associated with macrovascular or microvascular complications
In comparison to T1DM, our young-onset T2DM subjects had a more aggressive phenotype with more adverse cardiovascular risk factors. Despite similar glycaemic control, they developed more macrovascular and microvascular complications. A significant proportion of these complications occurred early in relation to the onset of T2DM, a pattern which was not observed in the T1DM group. The significant differences in prevalence of diabetic complications especially the macrovascular complications between our young-onset T2DM and T1DM patients (22% vs 0%) were most probably due to the earlier development of an atherogenic milieu among the young-onset T2DM patients in the presence of multiple adverse cardiovascular risk factors such as hypertension, atherogenic dyslipidemia with high TG and low HDL along with obesity. In the presence of prolonged period of asymptomatic dysglycaemia before the diagnosis of young-onset T2DM, they were predisposed to vascular damage which had probably commenced before the diagnosis of diabetes. The high prevalence of microvascular complications observed in the young-onset T2DM group despite similar glycaemic control could only be partially explained by the slightly longer disease duration and difference in age in comparison to the T1DM group. It was believed that the high prevalence of hypertension, atherogenic dyslipidemia and obesity among the young-onset T2DM patients which mostly were already present either before or within the first five years of diagnosis of diabetes also contributed significantly to the high prevalence of microvascular complications. The etiologic role of cardio-metabolic risk factors in the pathogenesis of microvascular complications have been implicated in several studies.[7][9] The overall findings of our study were consistent with the published literature demonstrating the adverse phenotype with high burden of cardiovascular disease associated with youngonset T2DM patients.[2][4][5]
We also found that being a young-onset T2DM patient (as opposed to T1DM), the presence of hypertension, a raised HbA1c and having longer duration of disease were independently associated with increased risk of macrovascular and microvascular complications. Dyslipidemia and obesity were not independent risk factors in our analysis. The lack of association was probably related to the fact that most of the patients with dyslipidemia were already well treated with a statin. The effect of obesity could not be ascertained due to the inability to calculate BMI with missing height data in 56% of our subjects. While hypertension, poor glycaemic control and long disease duration were expected to confer increased risk of diabetic complications and has been well described in the literature, this was the first study in Asia to demonstrate that being a young-onset T2DM patient independently confers an increased risk of diabetic complications up to 2.6 times above that of a type 1 DM. Similar findings had been reported in a United Kingdom population.[4] In the presence of adverse cardio-metabolic phenotype among the young-onset T2DM patients, controlling glycaemia alone is not likely to attenuate the susceptibility to premature macrovascular and microvascular complications. Early detection of dysglycaemia via vigilant screening in young adult at risk followed by aggressive control of all the associated cardiometabolic risk factors will be pertinent.
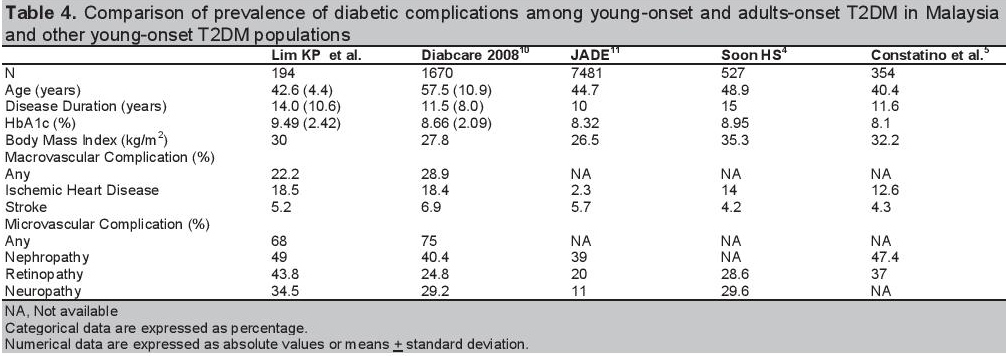
In the comparison of prevalence of diabetic complications of young-onset with the adult-onset T2DM population in Malaysia, our young-onset T2DM patients were younger, had slightly longer disease duration but poorer HbA1c.[10] Although the overall prevalence of macrovascular and microvascular complications was lower than the adult-onset T2DM patients from Diabcare, the individual prevalence of diabetic complications was similar for macrovascular and higher for microvascular complications. This implies that multiple diabetic complications were more likely to occur within the same individual for our young-onset T2DM patients compared to the adult-onset T2DM. In the comparison of prevalence of diabetic complications with other young-onset T2DM populations, it was, higher overall for macrovascular and microvascular complications across all groups.[4][5][11] (Table 4) Compared to the Joint Asia Diabetes Evaluation (JADE) cohort in Asia,[8] our young-onset T2DM patients had longer disease duration despite being slightly younger in age indicating an earlier age of diabetes onset. The HbA1c was poorer while the BMI was higher. As a result, the prevalence of microvascular complications as well as ischemic heart disease was much higher. In comparison with the Caucasian populations from United Kingdom and Australia, our young-onset T2DM patients had similar disease duration and BMI but were younger in age.[4][5] Both the prevalence of macrovascular and microvascular complications was similar except for retinopathy. As glycaemia is the main contributor to the development of retinopathy, this finding was most probably driven by the higher HbA1c in our young-onset T2DM patients. Based on these observations, it appeared that our young-onset T2DM patients behaved more closely to the Caucasian than the Asian cohort in terms of macrovascular complications likely to be driven by the high BMI with associated cardiovascular risk factors. A similar pattern was also observed in a local study of newly diagnosed T2DM patients with predominance of insulin resistance over insulin secretary dysfunction largely driven by the high mean BMI.[12] As for microvascular complications, our young-onset T2DM patients reported the highest prevalence for all individual components likely to be attributable to poor glycaemic control.
Click here to download Table 4Table 4. Comparison of prevalence of diabetic complications among young-onset and adults-onset T2DM in Malaysia and other young-onset T2DM populations
According to the fifth Malaysia National Health and Morbidity Survey (NHMS) conducted in 2015, the prevalence of diabetes among individuals aged 39 and below has increased by more than double compared to the third NHMS in 2006.[13] One of the main implications of this trend is a substantial increase in the number of child bearing age women with young-onset T2DM. Apart from a higher risk of complications associated with diabetes during pregnancy such as miscarriage, preterm labour, macrosomia, birth injury, neonatal hypoglycaemia, congenital malformations and perinatal mortality; numerous studies have shown that diabetes during pregnancy also confers an increased risk of obesity and diabetes in the offspring.[14][15] This leads to a looming epidemic of young-onset T2DM associated with more aggressive phenotype and higher prevalence of macrovascular and microvascular complications. Ultimately, this phenomenon will pose a significant burden to the health and economic status at the individual as well as society level as these individuals are predisposed to increased risk of complications during their productive years.
This is a pilot study in Malaysia examining the youngonset T2DM population by comparing the burden of diabetic complications in reference to the T1DM population and exploring the association between various clinical or metabolic risk factors with diabetic complications. By examination of historical records, it allowed retrospective capture of all events. The limitations of this study included a potential bias in subject selection from a single tertiary health institution which was not representative of the overall diabetic population in Malaysia. The other limitations included the small number of subjects, gender imbalance especially in the T1DM group and a significant amount of missing data for BMI and WC. In the absence of macrovascular event registered in the T1DM group, this study was also not powered to demonstrate the potential differential effects of the individual clinical or metabolic risk factors on macrovascular and microvascular complications. The influence of genetic factors could not be excluded as there was no data on family history of cardiovascular disease. Ideally, a larger number of subjects from multiple centres including primary, secondary as well as tertiary health facilities should be examined to minimize the impact of selection bias, gender imbalance and incomplete data.
A national registry for young-onset T2DM should be created to establish a longitudinal prospective cohort. A comprehensive national young-onset T2DM cohort along with more data from the region will be essential to study the natural history of young-onset T2DM and to develop a strategic approach in management of young-onset T2DM.
This study highlighted the aggressive nature of young-onset T2DM compared to T1DM with higher prevalence of macrovascular and microvascular complications and earlier occurrence in relation to the onset of diabetes. Early detection of dysglycaemia via vigilant screening in young adults at risk followed by intensive and aggressive control of the cardiovascular risk factors and glycaemic burden will be essential to prevent premature morbidity and mortality.
AcknowledgementsWe would like to thank Adam bin Bujang, Statistician, Clinical Research Centre, Kuala Lumpur for the statistical analysis.
Statement of AuthorshipAll authors have given approval to the final version submitted.
Author DisclosureAll the authors have declared no conflict of interest to the work carried out in this paper.
Funding SourceThis study was funded by Ministry of Health, Malaysia.
[1] Wilmot EG, Idris I. Early onset type 2 diabetes: Risk factors, clinical impact and management. Ther Adv Chronic Dis. 2014;5(6):234-44. DOI.