Since Simmonds reported the first case of pituitary abscess in 1914, only 200 cases have been reported in medical literature. There are no specific clinical presentations and imaging features that will make a preoperative diagnosis of a pituitary abscess possible. Pituitary abscess is an important differential diagnosis in patients presenting with a sellar-suprasellar mass.
CASEWe present the case of a 43-year-old female presenting with secondary amenorrhea. Ten months prior to her admission, she presented with cessation of menses. Two months prior to admission, she had bilateral temporal loss of vision. The patient had no known prior infection or surgical procedure done. The patient was fertile and was able to conceive twice before. Apart from bitemporal hemianopsia, the rest of the physical examination was normal. Preoperative diagnosis was a non-functioning pituitary adenoma with hypopituitarism and optic chiasmal compression. During transsphenoidal surgery, instead of a solid mass, there was egress of purulent fluid upon puncturing of the capsule, findings compatible with an abscess. There was immediate improvement in visual acuity and visual fields after surgery. The patient was treated with intravenous ceftriaxone 2 g every 12 hours for 14 days. She developed a cerebrospinal fluid leak, which was successfully treated with acetazolamide and drainage of CSF via lumbar tap. There was no post-operative diabetes insipidus.
Magnetic resonance imaging (MRI) of the pituitary gland showed a hetergenous sellar-supra-sellar rim-enhancing mass (Figure 1).
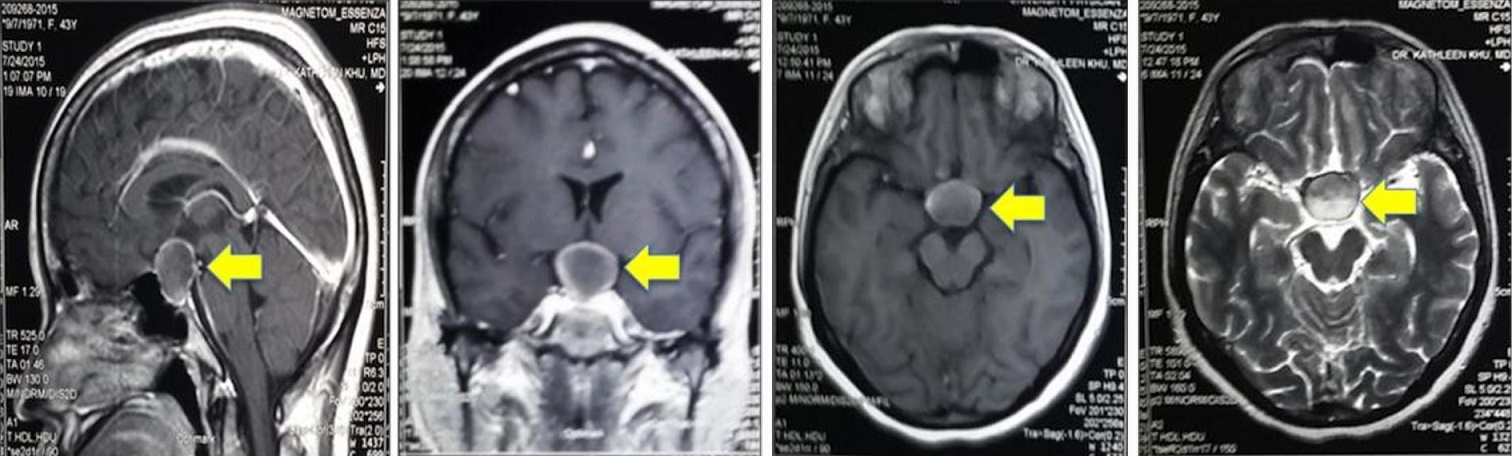
Figure 1. Post-gadolinium MRI showing (arrow) a 2.6 x 2.4 x 1.8 cm round rim-enhancing sellar-suprasellar mass with nodular component and mixed soft tissue and fluid signals compressing the optic chiasm. (a) Sagittal; (b) coronal; (c) Isointense on T1W1; and (d) hyperintenste on T2W1.
Prior to surgery, her pituitary function was evaluated. Hyperprolactenemia as the cause of amenorrhea was ruled out because the prolactin level was normal at 92.2 uIU/ml, (N: 92-868). The patient had hypogonadotrophic hypogonadism as shown by the low follicle stimulating hormone (FSH) 0.35 miU/ml (N: 0.6-9.5) and low estradiol 29.7 pg/ml, (N 127-476). The patient also had secondary hypothyroidism her TSH 0.5 μiU/ml (N: 0.3-5.4) and fT4 9.4 pmol/L (N: 11-24) were both low. The patient also had secondary hypocortisolism with an 8AM cortisol of 39.54 nmol/L (N: 138-690). Serum adrenocorticotrophic hormone level was not determined.
The patient did not present with diabetes insipidus. The pre-operative serum sodium was 136 mmol/L, postoperative serum sodium was 135 mmol/L (N: 136-144). Preoperative urine specific gravity was 1.024 and post operative urine specific gravity was 1.012.
There was no history of antecedent infection. There were no signs and symptoms such as fever. The patient had clear breath sounds and normal examination of the abdomen and genital area. Complete blood count showed a hemoglobin of 127 g/L, (N: 135-180), white blood cells 5.23 x 109/L (N: 4.5-11.0), neutrophils 41% (N: 50-70%) and lymphocytes 46% (N: 20-50%).
Histopathology showed benign cyst contents (Figure 2). Gram stain of the abscess showed a PMN 0-1/OIF, Gram-positive cocci 0-1/OIF. However, the abscess culture had no growth after 5 days of incubations. Work up for tuberculosis was also negative. Acid-fast bacilli smear was negative, as well as the polymerase chain reaction for M. tuberculosis.
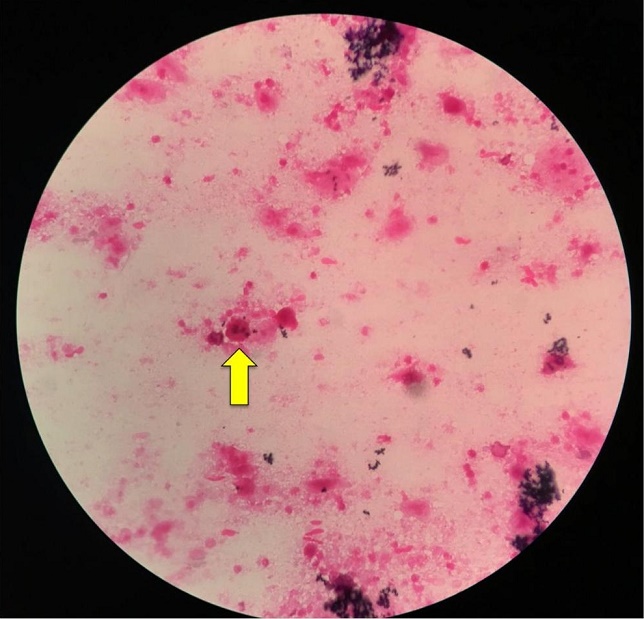
Figure 2. Histopathology specimen. Neutrophil (arrow) is seen in a background of proteinaceous or eosinophilic material with no other diagnostic cellular material (H & E, 100x).
The primary treatment for pituitary abscess is drainage. Empiric antibiotic coverage with Ceftriaxone 2 grams was given intravenously every 12 hours for 14 days. Patient had immediate improvement of blurring of vision post-operatively. The patient was able to count fingers during visual field confrontation test. There was no post-operative diabetes insipidus. Patient had cerebrospinal leak, which was resolved by giving acetazolamide. Patient was discharged on prednisone 7.5 mg/day and levothyroxine 100 mcg/tab, once a day.
Pituitary abscess is a rare and potentially life threatening condition. Simmonds reported the first case of pituitary abscess in 1914.[1] Since then, only 210 cases have been reported worldwide.[2] It may be caused by hematogenous seeding from an infection located elsewhere in the body or via direct extension of an adjacent infection.[3] It may occur in a previously healthy patient without pre-existing infection or pituitary gland lesion such as an adenoma.[4]
In a review of 24 cases done by Vates, the most common clinical presentations were non-specific headache, pituitary dysfunction, and visual disturbances.[5] In a review of 33 cases done by Fuyi, the most common presenting symptoms of pituitary abscess are panhypopituitarism, diabetes insipidus (DI), and non-specific headache. Among the 12 females included in this review, seven presented with amenorrhea. Three of the patients had resolution of amenorrhea post operatively after 32, 44 and 57 months of follow up. Two patients had persistent amenorrhea after 57 and 188 months of follow up. There was no mention about improvement of amenorrhea in the remaining two patients.[6] In a case series done by Lemoncito et al., two cases of pituitary abscess also presented with persistent amenorrhea despite surgical drainage of the abscess after 3 and 6 months of follow up.[7]
Our patient presented with panhypopituitarism, and left temporal hemianopsia. She did not present with DI or headache. She also has no prior infection. Her clinical presentation was more similar to the profile of patients described in the review of Vates. The panhypopituitarism may have been caused by the destructive process of the abscess on the pituitary leading to amenorrhea, beginning secondary hypothyroidism, and hypocortisolemia. The unilateral temporal hemianopsia is caused by the mass effect of the abscess, which was resolved immediately upon drainage of the abscess. However, resolution of the amenorrhea is not guaranteed as reported in the study of Fuyi and Lemoncito.Our patient presented with panhypopituitarism, and left temporal hemianopsia. She did not present with DI or headache. She also has no prior infection. Her clinical presentation was more similar to the profile of patients described in the review of Vates. The panhypopituitarism may have been caused by the destructive process of the abscess on the pituitary leading to amenorrhea, beginning secondary hypothyroidism, and hypocortisolemia. The unilateral temporal hemianopsia is caused by the mass effect of the abscess, which was resolved immediately upon drainage of the abscess. However, resolution of the amenorrhea is not guaranteed as reported in the study of Fuyi and Lemoncito.[6],[7]
Therefore monitoring for improvement of the amenorrhea in our patient is necessary during follow up to determine the need for hormonal replacement therapy.In the review by Vates, the most consistent finding on pituitary imaging was enlargement of the sella turcica, which demonstrated moderate to high signal levels on T2-weighted MR images, suggestive of a fluid-containing cyst and mildly intense or hypointense on T1-weighted MR images.[5] According to Fuyi, a post gadolinium rim-enhancing mass on MRI is noted in 64% of the patients with pituitary abscess.[6]
The MRI findings observed in our patient were a combination of the imaging features described in the two reviews mentioned. The MR image showed a high intensity signals on T2-weighted images and a rim enhancing mass. However, these findings are not specific for a pituitary abscess.. Differentials of rim-enhancing mass may include Rathke’s cleft cysts, cystic craniopharyngiomas or cystic adenoma.[6] There seems to be no specific diagnostic features that will help in making a diagnosis of a pituitary abscess pre-operatively.
The most common isolated organisms in pituitary abscesses are Gram-positive cocci. [2],[3],[6] However there are two cases wherein the isolated gram-positive cocci did not grow in the culture,[5] The gram stain of the patient’s abscess showed polymorphic neutrophils 0-1 /OIF and Gram-positive cocci 0-1/OIF; but there was no growth in the abscess culture. There were also no acid-fast bacilli seen and TB PCR was negative. A negative growth in the culture may have been caused by the preoperative use of antibiotics. The patient was given cefuroxime 1.5 intravenously, one hour prior to her operation.
Early diagnosis and aggressive antibiotic treatment may decrease mortality to 8.3%.6 Together with the clinical findings, the result of the MRI can be useful to guide appropriate management. Prognosis is generally good after drainage and antibiotic therapy. However, hormonal recovery is insufficient in most case series but improvement in vision has been documented.[5] Recurrence of the abscess has been reported and monitoring should be part of follow-up care.[6]
Pituitary abscess is an important differential diagnosis for sellar and suprasellar mass even in patients without prior history of infection or surgical procedure. There are no specific clinical and radiologic features that will enable a preoperative diagnosis of pituitary abscess. Correct diagnosis is important since the management includes drainage of the abscess and appropriate antibiotic coverage. Vision may improve after drainage of abscess, however hormonal recovery is not always observed in patients with abscess even after appropriate management.
Ethical ConsiderationPatient consent was obtained before submission of the manuscript.
Statement of AuthorshipAll authors certified fulfillment of ICMJE authorship criteria.
Author DisclosureThe authors declared no conflict of interest.
Funding SourceNone.
[1] Hanel RA, Koerbel A, Prevedello DM, Moro MS, Araújo JC. Primary pituitary abscess: Case report. Arq Neuropsiquiatr. 2002;60(3-B):861-5. PubMed DOI.