Primary hypothyroidism is a common paediatric entity which is frequently undiagnosed and untreated. Its protean manifestations include lethargy, hypothermia, hypotonia, constipation and mental retardation.[1] Oral manifestations causing difficulty in feeding include largesized tongue (macroglossia), delayed dentition and crowding of teeth.[2] Long term consequences include growth retardationand pubertal delay, though isosexual precocious puberty may occur in rare cases.[3],[4],[5],[6],[7],[8]
Here we describe a 16-year-old adolescent girl presenting with short stature, delayed puberty and feeding difficulties due to undiagnosed and subsequently untreated hypothyroidism.
CASEA 16-year-old Indian girl presented to the endocrinology out-patient department with short stature and delayed pubertal development with absence of menarche. She also complained of gradually progressive difficulty in chewing food since last 2 years. There was no history suggestive of dental malocclusion, trauma or any abnormalities in jaw opening or closing. There was no family history of growth retardation or pubertal delay, neither any surgical intervention nor radiation exposure during childhood. She was born of an uneventful pregnancy at 36 weeks gestation age by normal spontaneous vaginal delivery with normal birth length and weight. There was no history of any chronic illness during childhood. She studied in 8th grade and her academic performance was average.
On examination, facial puffiness was prominent along with a dry and scaly skin. There was crowding of her incisors (Figure 1). She had a large sized tongue, more evident on protrusion (Figure 2). Her hair seemed brittle with mild alopecia noted in the frontal region. There was no madarosis of eyebrows. There were no signs of goitre while the higher mental functions and neurological examination were within normal limits with slightly sluggish deep tendon reflexes in the lower limbs (grade 1+). Anthropometric measurements revealed a standing height of 134 cm (<3rd percentile for age and sex) and an arm span of 132 cm. She weighed 28 kg (<3rd percentile for age and sex). The mid-parental height as calculated from her parents was 164 cm. Tanner scoring was B1, P1 and A1.

Figure 1. Dental anomalies due to large tongue.
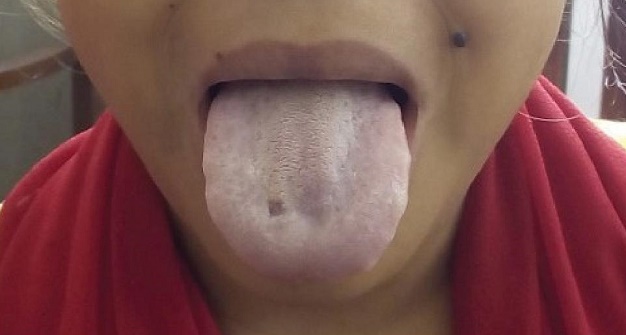
Figure 2. Macroglossia.
Her investigations revealed the following (Table 1): Hemoglobin=10.2 g/dl, and general blood picture suggestive of normocytic normochromic anemia, normal serum electrolytes, CPK and LDH. Liver functions and kidney functions were within normal limits. Thyroid function tests revealed TSH level >150 μIU/L (normal: 0.4-5) with low T4 and T3 levels, suggestive of overt hypothyroidism. Anti-thyroid peroxidase antibody (Anti TPO Ab) was >1000 IU/ml (normal: 0-50 IU/ml). Ultrasound study of the thyroid gland was mostly normal with a few hypoechoic lesions noted. Her bone age from xray of the left hand as calculated by Tanner-Whitehouse 2 was 8.9 years. Her gonadotropin levels (both FSH and LH) were low, implying pre-pubertal status. Thus, her short stature, delayed bone age and delayed pubertal development were attributed to hypothyroidism due to Hashimoto’s thyroiditis.
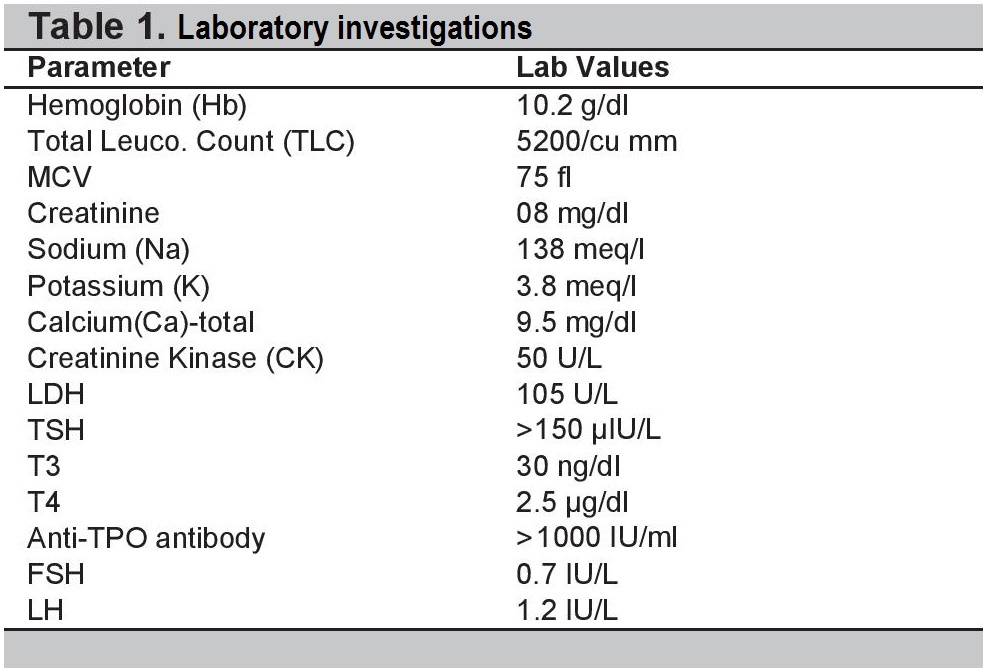
Table 1. Laboratory investigations.
She was started on levothyroxine replacement and counselled appropriately. After 6 months of therapy, she noted improvement in her chewing abilities. She is being monitored regularly for catch up growth and subsequent pubertal development.
Thyroid disorders are a fairly common occurrence in the paediatric population, and the prevalence of juvenile hypothyroidism was found to be 9.3-10.5% in the developing world.[9] The presentation ranges from asymptomatic, isolated biochemical abnormalities of thyroid function tests to overt clinical manifestations. Autoimmune thyroid disease, thyroid dysgenesis, binding protein abnormalities, TSH receptor mutations, thyroid hormone resistance, iodine deficiency, infectious thyroiditis are the common thyroid disorders observed in this age group.[1]
Overall, Hashimoto’s Autoimmune Thyroiditis is the most common cause of hypothyroidism in iodine-sufficient areas of the world. The worldwide incidence is estimated to be 0.3–1.5 cases per 1000 individuals with a definite gender predilection for females (M:F=15:1).
Deficiency of thyroid hormones during intra-uterine life leads to impairment of normal fetal brain development.[1] In childhood, hypothyroidism manifests as prolonged jaundice, umbilical hernia, constipation, lethargy, hypothermia and cold or mottled skin. Feeding difficulties are seen due to various oral manifestations like delayed eruption of teeth, malocclusion, large sized tongue (macroglossia) and thick lips.[2] Macroglossia can be attributed to accumulation of glycosaminoglycans and over-development of tongue musculature.[10]
Hypothyroid children may present with short stature and delayed onset of puberty. Height deficit correlates with duration of untreated hypothyroidism and can be estimated by calculating the difference between chronological and bone age.[3] They generally have very low T4 values and highly elevated TSH. On treatment with levothyroxine, bone age advances faster in comparison to height gain, hence final height always remains short of the genetic growth potential.
Besides, thyroid hormone deficiency results in delay of onset or retardation of progress of puberty, since it interferes with gonadotropin secretion.[4] Treatment with levothyroxine normalises the gonadotropin secretion and allows further progress of puberty. In rare cases, long standing untreated hypothyroidism may result in paradoxical isosexual precocious puberty (Van- Wyk Grumbach Syndrome) due to action of high levels of TSH on the FSH receptors.[5]
Our patient had features of macroglossia, short stature and delayed puberty owing to long duration of undetected and untreated hypothyroidism. Hence, clinicians must be aware of the protean manifestations of primary hypothyroidism and treat the child timely to prevent long term adverse consequences.
Primary hypothyroidism must be diagnosed and treated early to provide opportunity for adequate gain in height and timely onset and progress of puberty before complete skeletal maturation occurs.
Ethical ConsiderationInformed consent has been taken before submission of the manuscript.
Statement of AuthorshipAll authors certified fulfillment of the ICMJE authorship criteria.
Author DisclosureThe authors have declared no conflict of interest.
Funding SourceNone.
[1] Morreale de Escobar G. The role of thyroid hormone in fetal neurodevelopment. J Pediatr Endocrinol Metab. 2001;14(6):1453-62. PubMed.