Primary hypothyroidism is a common autoimmune disorder of paediatrics as well as the adult population, and may be associated with unusual manifestations, e.g., calf muscle hypertrophy, pericardial effusion, precocious puberty, etc. The prevalence varies from 10-12% in the Indian population.[1] Hypothyroidism, presenting with classic manifestations is readily diagnosed and treated. Occasionally, patients present with less commonly recognised symptoms, making the diagnosis less apparent. Such atypical presentations may be suggestive of another disease or pathological entity. Therefore, the initial focus of attention gets diverted away from hypothyroidism towards investigating for other diseases. We considered it instructive to compile a report about such patients, as it emphasizes the need to be aware of the unusual presentations of hypothyroidism and to consider hypothyroidism when confronted with such atypical clinical manifestations.
CASE 1An 11-year-old female child presented with complaints of growth failure, fatigue, puffiness of face, hoarseness of voice, and deafness for 1 year. She also gave a history suggestive of proximal muscle weakness, hair loss, constipation, and cold intolerance. Her antenatal, natal, and postnatal history were unremarkable as were her past and treatment history. There was no history of any radiation exposure. No other member of the family was affected.
On general examination, her pulse rate was 70/min, regular, all peripheral pulses palpable; BP was 86/70 mm Hg with no postural variation. The presence of coarse facial features, depressed nasal bridge, facial and periorbital puffiness, dry skin, and acanthosis nigricans was noted. She weighed 19.2 kg, her height was 108 cm (both below third percentile); arm span was 104 cm, the upper segment to lower segment ratio was 0.9. Her IQ was normal. Systemic examination revealed bilateral bulky calf muscles, delayed contraction and relaxation of ankle jerks, and pseudomyotonia of calf muscles with negative Gower's sign (Figure 1). Her gait was normal. The rest of the nervous system and other systemic examination were within normal limits. The investigation performed showed hemoglobin of 9.4 g% with normocytic normochromic red blood cells on peripheral smear. The total and differential leucocyte count and platelet counts were normal. Renal and kidney function tests were normal. Urinary examination showed no abnormalities. The bone age was only 5.3 years (by Tanner White House 2). Audiometry showed conductive hearing loss.

Figure 1. Pseudohypertrophy of the calf muscles.
Thyroid hormone deficiency was evident as serum T4 was <1.0 μg/dl (4.5-12.0), serum T3 was <0.25 ng/ml (70-130), and serum TSH was 1186.0 μIU/ml (0.30-5.0). A primary autoimmune etiology was confirmed by raised anti-TPO antibody titre >1300 U/ml. Serum CPK was raised to 1062 U/L and aPTT was prolonged for 47.90 s (34.90). Ultrasonography of the thyroid gland suggests diffuse bilateral enlargement of thyroid lobes. .
A diagnosis of autoimmune thyroid disease causing primary hypothyroidism, was made and she was treated with 50 μg thyroxine once a day. On follow-up after 3 months, she showed significant improvements in her symptoms, thyroid function tests and regression in the volume of the calf muscles was noted. Repeat TSH after 3 months was 2.54 μIU/ml.
CASE 2A 26-year-old married female presented with the chief complaints of menorrhagia for the last 3 months with intermittent abdominal pain for the last month. She had been bleeding heavily for the last 12 days, along with the passage of clots. Over the last 3 months, her cycle interval had increased from 45 to 60 days and bleeding had increased in duration and amount. Her menarche was at a normal age of 11 years followed by regular cycles until the last 3 months. There was history of weight gain and malaise for last 2-3 yrs. Her physical examination revealed weight 75 kg, height 156 cm and BMI 30.8. She had an apathetic expression. Her pulse was 64 bpm and BP 124/92 mm Hg. Her IQ was normal. She was pale with periorbital puffiness, dry skin and swelling over hands and feet and delayed reflexes. The thyroid gland was not enlarged and there was no galactorrhea. On abdominal examination, an abdominopelvic mass reaching upto the umbilicus was felt, which was cystic, non tender and mobile. Her laboratory tests revealed mild anemia with a dimorphic picture on peripheral blood film. Ultrasound of the abdomen and pelvis showed bilateral enlarged multicystic ovaries. The uterus was normal with endometrial thickness of 6.4 mm. Her TSH 124.6 IU/L (0.2–4.6 IU/L), total T4=1.2 μg/dL (5–12.5 μg/dL), T3=12.5 ng/dL (60–180 ng/dL)]. Ultrasound of the thyroid showed small thyroid lobes with heterogenous coarsened echo pattern suggestive of chronic thyroiditis. Antithyroid peroxidase was positive 1300 U/ml (positive >50). Patient was started on 50 ug of thyroxine and gradually increased to 125 ug. The acute bleeding episode was controlled with oral progesterone and hemostatic drugs. She was started on oral iron supplemenation and calcium. By 6 weeks, both the ovarian cysts had resolved completely. At the 3rd month follow up, the patient was euthyroid with TSH level of 3.67 μIU/ml along with normal menstrual cycles and weighed 64 kg.
CASE 3An 18-year-old female presented to the outpatient department with complaints of gradually progressive swelling over her legs over 3 months. There was no diurnal or postural variation, and it did not respond to diuretics previously prescribed to her. In addition, she had gained 5 kgs weight since 1 year, associated with malaise, fatigability and intolerance to cold. On further questioning, her relatives confirmed that her voice had become hoarse. She also took medications for relieving constipation. The patient was a non-smoker and non-drinker, with no family history of any chronic illness or thyroid disorders.
On examination, her skin was dry and scaly. Her pulse rate was 78/min, bilaterally symmetrical with normal rate, rhythm and volume. She was afebrile, having a normal blood pressure with no postural variation. Her eyes were slightly protruding with normal conjunctiva (Figure 2). A soft, diffuse swelling over her neck without any nodularity or overlying skin changes was observed suggestive of goitre. Bilateral, non-pitting edema was noticed below her knees. There was no evidence of tremor on outstretching her fingers. The rest of the systemic examination was within normal limits.

Figure 2. Hypothyroid ophthalmopathy.
On investigating further, haemogram, ECG, kidney and liver function tests were within normal limits. Fundus examination and perimetry was normal. Thyroid function tests revealed the presence of overt hypothyroidism with a thyrotropin (TSH) level of 94.1 μIU/ml (normal: 0.4-5), free 3,5,3’-triiodothyronine (FT3) of 1.76 pg/dl (normal: 1.8-4.2) and free thyroxine (FT4) of 0.54 ng/dl (normal: 0.8-1.9).Thyroid receptor antibody (TRAb) was 147 U/L (normal range: 0-9 U/L), anti-thyroid peroxidase antibody (Anti TPO Ab) titre was >3000 IU/ml (normal range: 0-50 IU/ml), suggestive of Hashimoto’s autoimmune thyroiditis. Ultrasound study of thyroid revealed bilateral enlargement of the thyroid gland with normal vascularity and absence of any nodular changes. Exophthalmos was documented with by Hertelex ophthalmometry. Clinical activity score (CAS) was 0 and a “NOSPECS” score was class 1.
Subsequently she was started on levothyroxine replacement therapy (dosage 1.6 µg/kg body/wt.). Over the next 6 months, there was gradual regression of pedal edema. She was relieved of her gastrointestinal symptoms and reported feeling more energetic than before. However, her eye changes were more or less unchanged and she continues to present himself at regular intervals for follow up.
CASE 4A 33-year-old female presented to the emergency department with complaints of insidious and gradually progressive breathlessness, along with swelling of both feet. There was no history of medical illness and drug history in the past. Vital signs on admission were recorded (temperature, 37°C; blood pressure, 86/54 mm Hg; heart rate, regular at 68 beats/min). On examination, the apex beat was not felt and the heart sounds were soft and distant. The JVP was raised (6 cm). Chest auscultation revealed bilateral basilar crepitations, and there was mild tenderness in right upper quadrant of the abdomen. Her SpO2 was 95%, and other vitals were stable. Electrocardiogram showed heart rate of 68/min with low voltage pattern with electrical alternans. Bedside echocardiogram demonstrated small heart size with massive pericardial effusion and signs of early diastolic right ventricular (RV) collapse (Figures 3 and 4). There was swinging motion of heart within large effusion, prominent respiratory alteration of RV dimension with right atrial (RA) and RV collapse during diastole. Pericardial effusion was noted in the pericardial cavity and all cardiac chambers were of small size with predominant diastolic heart failure. A provisional diagnosis of pericardial effusion with cardiac tamponade was made. Investigations revealed elevated Pro BNP levels (>1000 pg/ml). Renal functions were slightly deranged (Creatinine 1.6 mg/dl, BUN 30 mg/dl) with normal electrolytes. Liver functions showed elevated transaminases (SGOT 140 IU/L, SGPT 80 IU/L). A thyroid profile revealed TSH=300 mIU/L (N=0.5-4.2 mIU/L), T4 (total)=3µg/dl (N=5.01-12.45 µg/dl), consistent with hypothyroid state. Serum Anti TPO antibody 448.70 U/ml (N=<65). Ultrasound study of the abdomen showed presence of mild hepatosplenomegaly, minimal ascites and evidence of increased systemic venous pressure. We transferred the patient immediately to the Intensive Care Unit for pericardiocentesis. Thyroxine replacement was started. Unfortunately, the patient’s condition deteriorated after 3 days. She went into a state of refractory shock, unresponsive to fluids and vasopressors. We suspected an adrenal crisis, and gave her intravenous hydrocortisone (100 mg TID). However, she could not be resuscitated and expired on the 4th day of hospitalization.
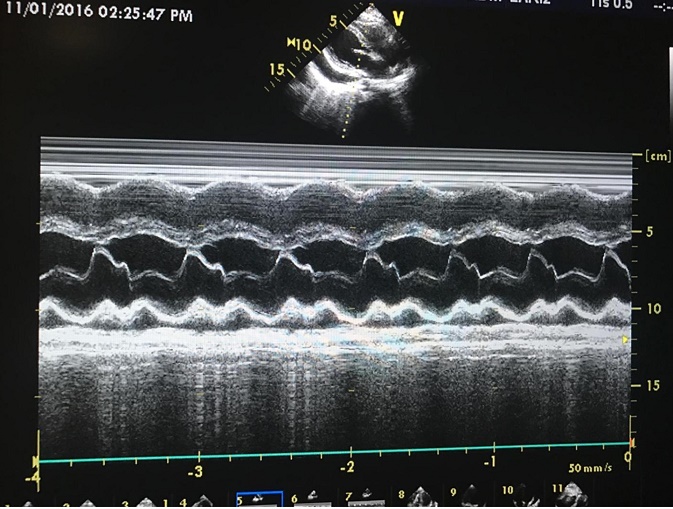
Figure 3. Apical four chamber view shows right atrial and right ventricle diastolic collapse
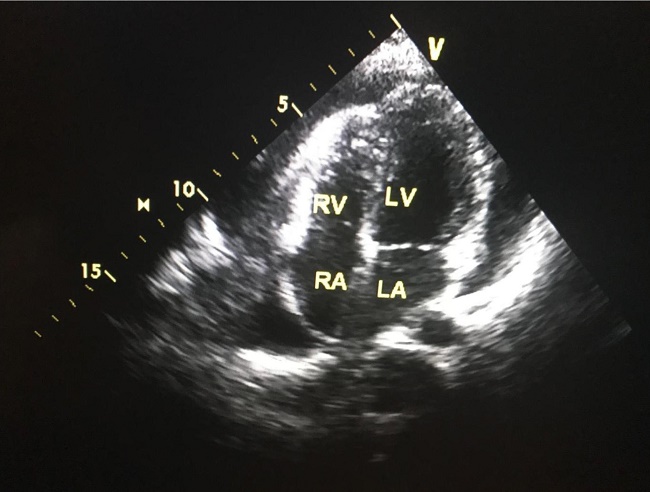
Figure 4. M-mode echo at the level of mitral valve in parasternal long axis shows diastolic right ventricle collapse.
CASE 5
An 18-year-old man presented with a history of enlargement of the testes for the last 10 years. He had a normal birth and normal childhood development. However he had failed to gain height during his adolescent years, with no evidence of development of axillary hair, pubic hair, gynecomastia, beard and moustache. There was no history of weight gain, nor any suggestion of mental retardation. On examination, his height was 126 cm (less than 3rd percentile), weight of 36 kg (less than 3rd percentile), body mass index of 22.7 kg/m2, body surface area of 1.10 m2, arm span of 124 cm. The mid parental height was calculated to be 160 cm. His sexual maturity score was axillary hair (A) stage 1, pubic hair (P) stage 1 with a testicular volume of 20 ml (Figure 5). He had coarse facies, dry skin, brittle nails, calf muscle hypertrophy and delayed relaxation of ankle reflexes. There was no evidence of goitre. His investigations revealed a normal haemogram, renal and liver functions. Bone age was 7.2 years (Tanner Whitehouse 2 staging). Hormonal profile was consistent with primary hypothyroidism [TSH >100mIU/L, T4 (total) =2.1 μg/dl]; anti-thyroid peroxidase antibody levels were raised (500 units/ml).FSH, LH and testosterone levels were within normal limits. Ultrasound revealed enlarged testicular volume (right = 24.5 ml, left = 24 ml) with no evidence of varicocele or fluid collection. The patient was subsequently started on levothyroxine replacement and is being followed up regularly for progress of pubertal development. On regular follow up, testicular size remained the same; however, axillary and pubic hair appeared and patient had considerable catch up growth.

Figure 5. Testicular volume >25 ml bilaterally, with no pubic hair in hypothyroid patient.
An 18-year-old male patient was diagnosed to have primary hypothyroidism 6 months back following weight gain, edema and facial puffiness of 3 years duration. His initial thyroid function tests showed the following T4: 2.3 μg/dl (5.01-12.4) T3: 0.35 ng/ml (0.6-1.81) and thyroid stimulating hormone (TSH): 180 μIU/ml (0.35-5.50) and he was started on levothyroxine, with significant improvement of symptoms. He was referred to our hospital after her developed myoclonus for the previous 1 month, 2 months after thyroxine replacement therapy.
On examination, he was conscious, with cognitive impairment and had memory loss for recent events, with the poor attention span, difficulty in finding words, dyscalculia and dysgraphia. His mini mental status examination (MMSE) was 11 suggestive of moderate cognitive impairment. He also had myoclonus, involving both upper limbs and lower limbs.
On investigation, blood routine examination and erythrocyte sedimentation rate were normal and liver function tests, kidney function tests, electrolytes calcium and magnesium were normal, as was the arterial blood gas analysis. His most recent TFTs showed normal T3 and T4 levels, with mild elevation of TSH (TSH-9.1 μIU/ml). Anti-thyroid peroxidase antibody was positive (>1300 IU ml). His electroencephalogram (EEG) showed a diffuse slow wave activity and magnetic resonance images (MRI) non-specific white matter changes (Figures 6 and 7). Cerebrospinal fluid (CSF) study had normal cytology, but slightly increased protein of 69.2 mg% (N=10-50 mg%). Antinuclear antibody titer, anti-double-stranded deoxyribonucleic acid, hepatitis B surface antigen, anti-hepatitis C virus, lupus anticoagulant and Venereal Disease Research Laboratory (VDRL) tests were carried out to evaluate the cause of decreased cognitive function, myoclonus and seizures, which were all negative. CSF protein electrophoresis was normal.
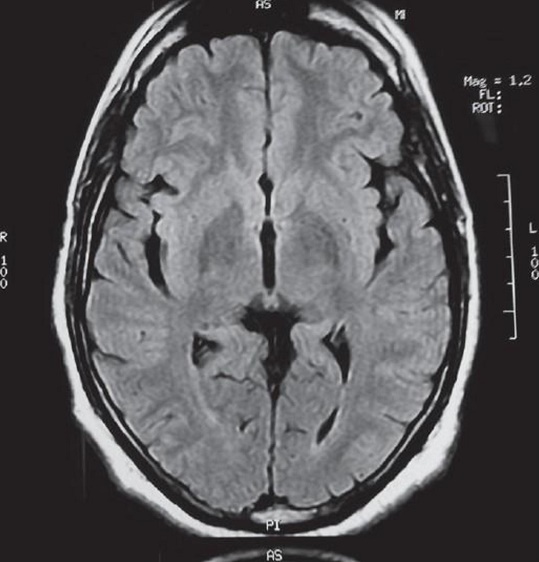
Figure 6. Magnetic resonance images showing non-specific White matter changes in primary hypothyroidism.
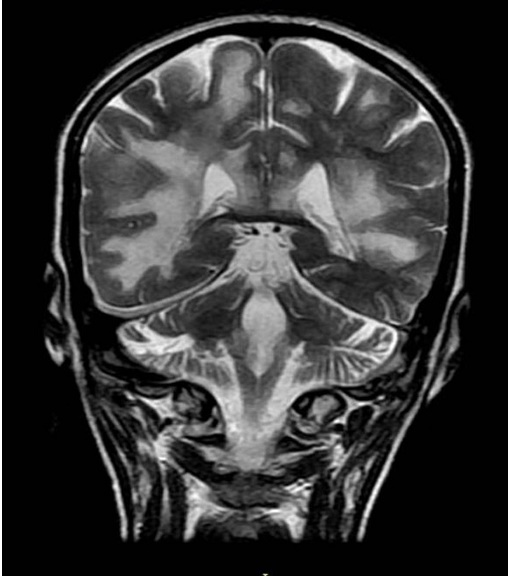
Figure 7. Magnetic resonance images showing non-specific White matter changes in primary hypothyroidism.
In view of these neurologic symptoms, associated with high titers of serum anti-thyroid antibodies and the exclusion of other possible causes of encephalopathy, patient was diagnosed with “steroid-responsive encephalopathy and associated autoimmune thyroiditis” (SREAT)/Hashimoto's encephalopathy. He was started on IV methyl prednisolone 1 g/day for 3 days and was shifted over to oral prednisone 1 mg/kg/day. There was a marked improvement in his symptoms with no further episodes of myoclonus or seizures. One month after discharge, the patient reported a sustained improvement in all parameters, including memory and cognition, making it possible for his to return to an almost normal routine. His MMSE had improved to 26 and he was seizure free. The prednisone dose was tapered over 3 months without the recurrence of symptoms.
CASE 7A 28-year-old female presented to the Emergency Department with a one day history of altered sensorium. She had a history of generalised headache of six months duration, easy fatigability, coarseness of facial features, pedal edema and huskiness of her voice for the last 3 months. She had developed diplopia and diminution in vision over the previous 20 days. She also had a history of irregular menses for 5 years. On examination, pulse rate was 78 beats/minute and regular. Cranial nerves were normal except for right lateral rectus paresis. Fundus was normal. There were no focal neurological deficits. Deep tendon reflexes were normal. Routine blood investigations were normal, except low hemoglobin (6.4 gm/dL). Her hormonal profile showed raised thyrotrophin stimulating hormone (TSH) (>300 μIU/dL, range 0.30-5.5) and low T3 (12.2 ng/dL, range 60-200) and T4 (0.86 microgram/mL, range 4.5-12.0). Prolactin was 65 IU/dL. Further investigation showed positive anti-TPO antibody >1300 [N<65]. A possible diagnosis of an intracranial space occupying lesion was entertained, but magnetic resonance imaging (MRI) of brain showed diffuse pituitary enlargement (Figure 8). A diagnosis of autoimmune thyroiditis and primary hypothyroidism with pituitary hyperplasia was suspected. She was started on oral L-thyroxine 75 mcg/day and low dose of steroids. At 6 months follow-up, she was doing well and T3, T4 and TSH levels were in normal range. Follow-up imaging was not performed as the patient was lost to follow up.
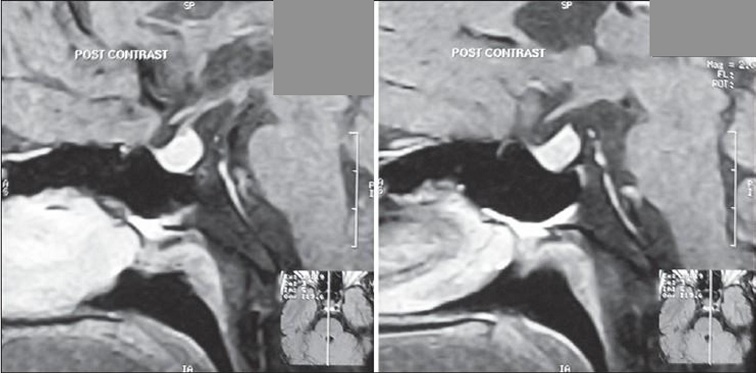
Figure 8. Magnetic resonance images showing pituitary hyperplasia in primary hypothyroidism.
In our case series, the female to male ratio was found to be 1.4:1. The sex distribution of the various unusual manifestations in our primary hypothyroidism patients is given in Table 1.
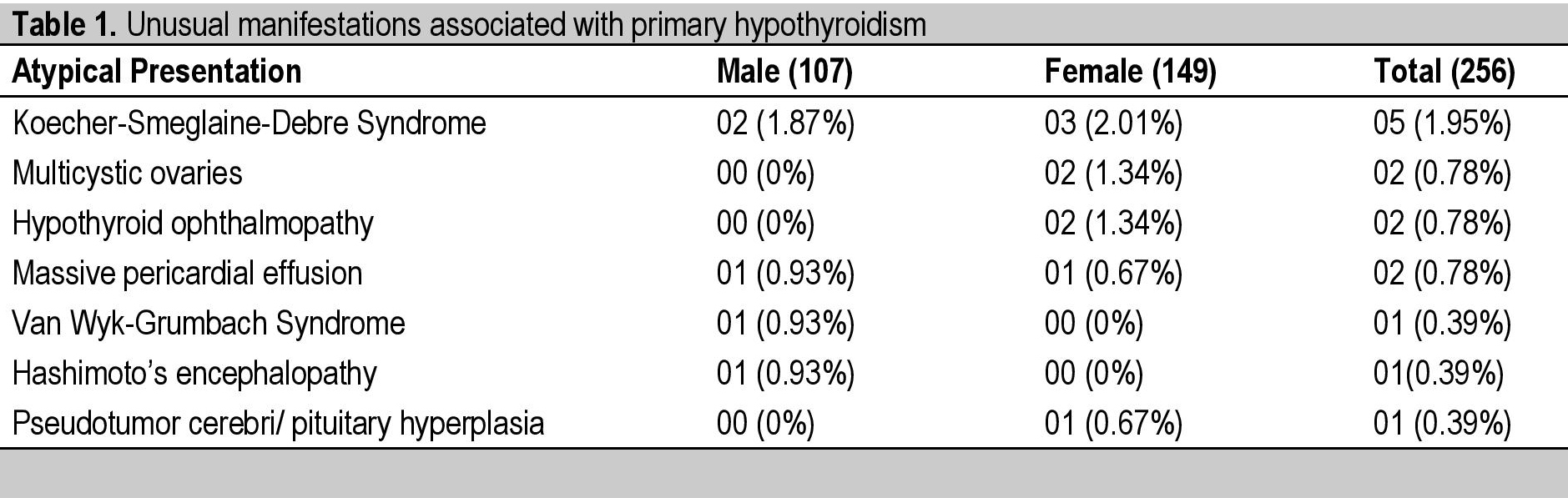
Table 1. Unusual manifestations associated with primary hypothyroidism
Hypothyroidism is failure of the thyroid gland to produce enough thyroid hormone to meet the metabolic needs of the body.[1] Hypothyroidism presents with a myriad of subtle and nonspecific manifestations like weight gain, poor concentration, depression, fatigue, muscular weakness, menstrual irregularities, short stature, etc. Some features of hypothyroidism are more suggestive like dryness of skin, proximal myopathy, constipation, cold intolerance and dry brittle hair.[2] The presentation of hypothyroidism depends on various factors like age and sex.[1] In 2003, a large study involving 40,000 patients attending an Omani health facility revealed that almost half of the patients were asymptomatic, while fatigue was evident as the most common symptom presenting in 30%; the other common presenting features were constipation, weight gain, and carpal-tunnel syndrome. Sleep apnoea, snoring, menorrhagia, dysphagia and dysarthria were seldom present.[3]
There are some unusual manifestations of hypothyroidism reported in the medical literature. As their exact prevalence in a hypothyroid population has not been studied epidemiologically, they often prove to be diagnostic challenges. The patients presenting with such manifestations are often misdiagnosed because of unawareness amongst the primary care providers, ultimately leading to a long delay in treatment and poor therapeutic outcomes. The care of such patients can be improved by familiarizing primary care providers with these unusual manifestations. In the present report, we document the presence of unusual presenting manifestations of hypothyroidism in a cohort of 256 patients diagnosed with primary hypothyroidism within a 2 year period in a tertiary care centre.
In our study the most common unusual presenting feature was Koecher-Debre-Smeglaine Syndrome (KDSS), which was present in five pediatric patients (2 males and 3 females) out of 256 hypothyroid patients. KDSS usually presents in the age group between 18 months and 10 years with the combination of hypothyroidism, calf muscle pseudo-hypertrophy, delayed muscle contraction and delayed relaxation of reflexes, along with percussion myxoedema.[4] The adult variant of KDSS is known as Hoffman’s Syndrome. Muscles of the extremities, limb girdle, trunk, hands and feet are commonly involved. The affected muscles are bulky, rubbery or firm, hypotonic and weaker than healthy muscles, hence the descriptive term “Herculean muscles.” The involved muscles do not show any specific microscopic features and the underlying pathogenesis is still obscure, although the accumulation of glycosaminoglycans and glycogen are thought to play a role.[4],[5] KDSS shows a good response to levothyroxine therapy, as was seen in our patients.
The other relatively common atypical presentation in our study was multicystic ovaries found in two patients. Hypothyroidism is a rare cause of ovarian hyperstimulation syndrome (OHSS) which usually occurs in the setting of exogenous FSH treatment.[6] Hypothyroidism is usually overlooked as a cause of ovarian cysts and patients may undergo surgery without any improvement.[6] A number of theories have been proposed to explain the development of multicystic ovaries in hypothyroid patients. The homologous structure of TSH and FSH causes stimulation of ovarian FSH receptors (specificity-spillover) by excessively raised serum TSH levels in patients with untreated hypothyroidism.[7] Multicystic ovaries can be caused by a differential increase in FSH concentrations along with low LH concentrations due to modification of GnRH pulse frequency by increased TRH in hypothyroid patients.[8] Hyperprolactinemia possibly due to elevated hypothalamic TRH may suppress LH secretion. Also, the clearance of FSH is reduced in hypothyroidism, and there may be activating FSH receptor mutations enhancing the effect of elevated TSH on the ovaries.[6] These multicystic ovaries are extremely important to diagnose in primary hypothyroid patients who may undergo unnecessary surgery since levothyroxine therapy resolves the condition, as was apparent in our study.
Two women presented with orbitopathy. Graves’ ophthalmopathy (GO) occurs in close temporal relation with hyperthyroidism but rarely can occur in hypothyroid and even in euthyroid subjects. The prevalence of GO in euthyroid and hypothyroid subjects ranges from 1.6% to 8.4%.[9] The symptoms differ between hyperthyroid and hypothyroid GO patients in various aspects. GO in hypothyroid patients is more asymmetrical with lesser soft tissue involvement and less marked clinical manifestations.[9] TRAbs are present in 69% of euthyroid and hypothyroid patients with GO. The number further increases to 75% when AntiTPO and TRAbs are considered together.[9] The mean TBI concentration is less in hypothyroid and euthyroid patients with ophthalmopathy as compared to hyperthyroid patients during the initial 6 months.[9]
We had 2 patients who presented with massive pericardial effusion as the primary clinical manifestation of hypothyroidism. Although mild pericardial effusion is common cardiovascular manifestation of hypothyroidism, the occurrence of massive pericardial effusion is a rare phenomenon.[10] Pericardial effusion (PE) in hypothyroidism is a part of the spectrum of polyseropathy characterized by extravasation of albumin and inadequate lymphatic drainage. The pericardial fluid is typically straw colored with high concentration of globulins and lymphocytes.[11],[12] Treatment of hypothyroidism is mandatory along with pericardiocentesis.
One child with primary hypothyroidism presented with the rare syndrome known as Van Wyk-Grumbach syndrome (VWGS). This refers to the occurrence of paradoxical isosexual precocious puberty along with short stature and delayed bone age in a case of long standing untreated primary hypothyroidism.[13] The VWGS syndrome is seen more commonly in girls.4,5,14 It presents as precocious isosexual puberty, delayed bone age, vaginal bleeding and ovarian cystic changes in girls and as isolated testicular enlargement (macro-orchidism) in boys without phallic enlargement, pubic hair development, or morning erections. Short stature and delayed bone age are seen in both.[4],[5],[14] This occurs as a result of high TSH levels in primary hypothyroidism stimulating ovarian and testicular FSH receptors leading to isosexual precocious puberty. The theory is supported by the fact that VWGS does not occur in secondary or tertiary hypothyroidism and the degree of precocity is directly proportional to the TSH concentration.[4],[5],[14]
In our study, we found one patient presenting with “steroid-responsive encephalopathy and associated autoimmune thyroiditis (SREAT)/Hashimoto’s encephalopathy. “Steroid-responsive encephalopathy and associated autoimmune thyroiditis (SREAT) is a rare steroid responsive encephalopathy presenting with persistent or fluctuating neurological and neuropsychological deficits associated with anti-thyroid antibodies.[15] The diagnosis is often difficult because of varied subtle manifestations and rarity of the syndrome. The exact pathophysiology is unknown but various hypotheses have been proposed like autoimmune cerebral vasculitis, toxic effects of thyroid-stimulating hormone on the central nervous system and neuronal reaction mediated by antibodies.[16] Anti-thyroid antibodies are considered as the markers of autoimmunity but they probably do not have a role in pathogenesis.[15] The EEG changes are nonspecific in 90-98% of patients, while brain MRI may show abnormalities in 49% patients, namely cerebral atrophy, focal cortical abnormality, diffuse subcortical abnormality and non-specific subcortical focal white matterabnormality.[15] The syndrome is steroid responsive while in 5% non-responsive cases azathioprine, IVIG, or plasmapheresis can be tried.[15]
Lastly, one patient with primary hypothyroidism in our study presented with a pituitary mass. In this situation, the decreased levels of thyroid hormone lead to loss of negative feedback, resulting in increased secretion of TRH from hypothalamus and TSH from pituitary. Under constant TRH stimulation, pituitary thyrotropes become hyperplastic and hypertrophied and present as a pituitary mass.[17] Although sellar enlargement is more common in primary hypothyroid children than in adults, patients seldom present with neurological signs of sellar expansion, unlike adults who may present with headache and other neurological symptoms.[17]
Besides the usual clinical manifestations of primary hypothyroidism, there are others that are very unusual,and hence are not easily recognised by the treating physician. The timely identification of these atypical presentations is very important for early intervention and treatment of hypothyroidism.
Ethical ConsiderationInformed consent has been taken before submission of the manuscript.
Statement of AuthorshipAll authors certified fulfillment of the ICMJE authorship criteria.
Author DisclosureThe authors have declared no conflict of interest.
Funding SourceNone.
[1] Unnikrishnan AG, Kalra S, Sahay RK, Bantwal G, John M, Tewari N. Prevalence of hypothyroidism in adults: An epidemiological study in eight cities of India. Indian J Endocr Metab. 2013;17(4):647-52. PMID: 23961480. PubMed Central DOI.