Metabolic Syndrome is a common condition worldwide and has been associated with increased risk for other comorbidities notably cardiovascular events and diabetes mellitus. It is initially associated with obesity and insulin resistance and over the years, different criteria were developed for the diagnosis of this condition namely NCEP III, WHO, IDF, NCEP/ATP III-AHA/NHLBI, but this basically includes 5 main criteria: abdominal obesity, elevated triglycerides, low High Density Lipoprotein, elevated fasting blood sugar and hypertension.
Several prevalence studies have been done on obesity and numbers vary based on racial and ethnic subgroups. Its prevalence was quoted to be 23.1% to 26.7% in the United States with predominance in the female population.[1],[2] In the Strong Heart Study, Metabolic Syndrome was present in 35% with 7.9% developing cardiovascular events over 7.6 ± 1.8 years of follow-up.[3] In the FINRISK study where they used the modified World Health Organization criteria for Metabolic Syndrome, it was present in 38.8% in men and 22.2% in women.[3] In a local study done by Punzalan et al., entitled Prevalence of Metabolic Syndrome among adult Filipinos, there is 14.2% prevalence of metabolic syndrome in the general population using NCEP criteria.[4] In another prevalence study of metabolic syndrome among adult Filipinos comparing 3 different criteria for diagnosis, some differences seen in the results were as follows: 11.9% using the National Cholesterol Education Program/ Adult Treatment Panel (NCEP/ATP III) criteria, 14.5% prevalence in the general population using IDF criteria and 18.6% prevalence using NCEP/ATP III criteria modified by the American Heart Association/National Heart, Lung and Blood Institute (NCEP/ATP III-AHA/NHLBI) criteria.[5] However, breakdown of prevalence of metabolic syndrome based on different BMI was not specified in this study.
There is evidence that BMI predicts metabolic syndrome differently across racial/ethnic groups. Recent studies have shown that metabolic abnormalities are not only seen in obese population but in normal weight subjects as well. In the CRONICAS Cohort Study which involved South American Hispanic subjects, there was 19.0% overall prevalence of individuals with normal BMI having >3 risk factors (central obesity, high triglyceride, low HDL, elevated fasting blood sugar, elevated blood pressure) of metabolic syndrome in addition to high hs-CRP and HOMA-IR and among these, 43.1 % were already classified as metabolically unhealthy.[6],[7] Comparable prevalence of metabolic abnormality was observe in subjects with BMI of 25 kg/m2 in Non-Hispanic whites as with 19.6 kg/m2 for Asian women and 19.9 kg/m2 for Asian men.[6]
In international studies, it has been shown that Asians and specifically Filipinas were less likely to be obese (BMI≥30 kg/m2, 8.8% ), with lower levels of HDL cholesterol as compared with their Caucasian counterpart and with higher prevalence of metabolic syndrome computed at 34% vs 13% in Caucasians.[8] Filipinos are known to have leaner body mass index with lower incidence of obesity as compared to other race and studies have shown that typical picture of a Filipino with diabetes has lower BMI with increased visceral adiposities (by truncal fat and waist girth) after adjusting for total body fat (by DEXA) as shown in a study done by Araneta et al.,[6] In a community-based cross-sectional study in the Philippines done by Pagsisihan et al., in 2016, they have shown that even at lower BMI cut-offs of 23 kg/m2 in males and 24 kg/m2 in females, it was already associated with the occurrence of at least 1 cardiometabolic disease (Type 2 diabetes mellitus, hypertension or dyslipidemia).[9]
Although there have been local prevalence studies of metabolic syndrome among Filipinos, there has been no study done yet to determine prevalence of metabolic syndrome among the different BMI categories and specifically those with lower and normal BMI. With the present evidences that metabolic syndrome is not only seen in obese population, the researchers would like to determine the prevalence of this group of individuals in the Filipino population. Determination of prevalence of metabolic syndrome and its individual components among the different BMI categories in Filipinos will aid us in targeting modifiable risk factors in at-risk population.
This study aims to determine the prevalence rates of metabolic syndrome and its individual components across different BMI categories (normal-weight, overweight, pre-obese, obese individuals) among patients seen at Wellness Center and Obesity and Weight Management Center, St. Luke’s Medical Center Quezon City (SLMC-QC) and to describe LDL, ALT and creatinine characteristics among patients with metabolic syndrome by BMI category.
METHODOLOGYThis was a 3-year (2013-2016) retrospective study utilizing chart review of adult patients seen at the Wellness Center and Obesity and Weight Management Center at St. Luke’s Medical Center Quezon City (SLMC-QC), a 650-bed capacity tertiary hospital in the Philippines. Patients seen in the Wellness Center and Weight Management Center include healthy individuals for annual executive check-up as well as individuals with previously known health concerns. Included were adult patients at least 18 years old and above seen both as outpatient and inpatient with computed BMI ≥18.5 kg/m2 with complete anthropometric measurements (height, weight, BMI and waist circumference), blood pressure monitoring and or anti-hypertensive medications, blood chemistries (Fasting Blood Sugar (FBS), Triglycerides, High Density Lipoprotein (HDL), Alanine Amino Transferases (ALT), Creatinine). Medication history for intake of anti dyslipidemic medications, oral hypoglycemics and/or insulin were also noted and recorded. Elevated ALT was defined as >63 U/L, Elevated LDL >130 mg/dL and elevated creatinine as >1.3 mg/dL. Exclusion criteria include pregnancy, patients with missing height or weight measurement, patients with chronic kidney disease with edema and on dialysis, patients with decompensated congestive heart failure and patients with decompensated liver disease.
Lists of all patients seen at the Wellness Center and Obesity and Weight Management Center of St. Luke’s Medical Center Quezon City (SLMC-QC) were retrieved. Patients with complete anthropometric measurements (height, weight, waist and hip measurement) were identified. Data were gathered through chart review and use of St Luke’s Medical Center Health Care System version 1.8.1, using a data sheet. Data collected included the following: age, gender, height, weight, computed body mass index, waist and hip measurement, blood pressure, list of anti-hypertensive, anti-diabetic and lipid-lowering medications, blood chemistry results of fasting blood sugar, triglycerides and High Density Lipoprotein (HDL). Other pertinent data that were reviewed included the serum creatinine and serum alanine aminotransferase (ALT) levels. Data on their first visit were recorded and included in the analysis.
For this study, metabolic syndrome was defined as patients who meet the criteria as set by NCEP/ATP III-AHA/NHLBI (2005). Any 3 of the following 5 features: waist circumference: Southeast Asian cut-off: Male ≥ 90 cm and Female ≥80 cm; raised Triglycerides: ≥150 mg/dL or specific treatment for this lipid abnormality; reduced HDL cholesterol : <40 mg/dL in males or 50 mg/dL in females or specific treatment for this lipid abnormality; raised BP: SBP ≥130 mmHg or DBP ≥85 mmHg or treatment of previously diagnosed hypertension; raised Fasting Plasma Glucose: FPG ≥100 mg/dL or previously diagnosed Type 2 Diabetes Mellitus.
Body Mass Index was computed using weight in kilogram divided by height in meter squared and were divided into NORMAL: 18.5-22.9 kg/m2; OVERWEIGHT: 23- 24.9 kg/m2; PRE-OBESE: 25-29.9 kg/m2 and OBESE: ≥30 kg/m2. Classification of BMI categories was based on the Asia-Pacific cut-offs.
Sample size was calculated based on the comparison of prevalence of metabolic syndrome in the general population and in the obese individuals. Assuming that prevalence of metabolic syndrome in the general population is 14.2% (Punzalan, 2004) and in the obese population is hypothesized to be 50% higher, with an alpha error of 5%, power of 80% and 1-tailed test of hypothesis, sample size required is 356 per group or 1424 for 4 groups. Actual sample size obtained however was only 1367. Results however showed that the hypothesized 50% higher prevalence of metabolic syndrome in the obese than the non-obese turned out to be more than 100% in our results. Thus, the actual sample size obtained in the study was more than enough to get a statistically significant result.
Statistical AnalysisData were processed and encoded in Microsoft Excel and data analysis done using SPSS version 20. Prevalence of metabolic syndrome and its individual components were tabulated and presented in percentage. Comparison of the prevalence of metabolic syndrome and its individual components across different BMI categories was computed using Chi square test. Level of significance was set at alpha level of 0.05 with 95% confidence interval. Results were considered significant if p-value was <0.05.
Ethical ConsiderationThe clinical protocol and all relevant documents were reviewed and approved by Institutional Ethics Review Committee of St. Luke’s Medical Center, Quezon City. Patient confidentiality was respected by ensuring anonymity of patient records. All study data were recorded and investigators were responsible for the integrity of the data i.e. accuracy, completeness and legibility. The manner of disseminating and communicating the study results guaranteed the protection of the confidentiality of patient’s data.
Data collection was done by the main investigator. To ensure confidentiality, each patient was assigned a reference number. Data collection forms are kept confidential and encoded in excel file. In this process, only the members of this study have access to the patients’ information. Data will be kept for 10 years and stored in the research library of the section. After the study, soft copy of the data will be stored by the main proponent and any hard copy of the data collection forms will be shredded.
A total of 1367 subjects were included in the study. The clinical and demographic characteristics of subjects included are shown in Table 1. Mean age of patients included was 53.3 (SD=12.4 years) with youngest of 18 years old and oldest at 86 years old. In terms of gender, there is a larger percentage of females included at 52.9%. Highest percentage of the subjects was in the pre-obese subgroup at 37.2% and least are subjects in the normal subgroup at 15%. The mean BMI was 28.2 kg/m2 with lowest of 18.5 and highest of 67.9 kg/m2.
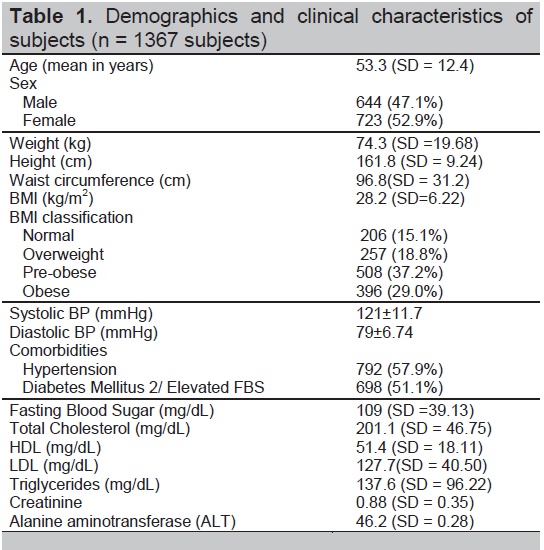
Table 1. Demographics and clinical characteristics of subjects (n=1367 subjects)
In individuals with metabolic syndrome, there is a noted female predominance in the lower BMI at 33.3% in the normal subgroup in contrast to a male predominance of patients in the higher BMI subgroup at 64.6% in the obese subgroup as shown in Table 2.

Table 2. Presence of metabolic syndrome in relation to different BMI categories and gender
Among the 1367 subjects, the most prevalent feature of metabolic syndrome is central obesity at 82.9%, followed by hypertension, elevated blood glucose and low HDL with high triglyceride as the least common (Table 3). Other metabolic parameters such as elevated LDL, ALT and creatinine level have 42.9%, 16.4 % and 3.4% overall prevalence rates respectively (Figure 1).
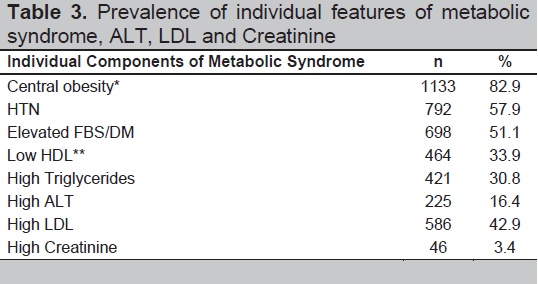
Table 3. Prevalence of individual features of metabolic syndrome, ALT, LDL and Creatinine
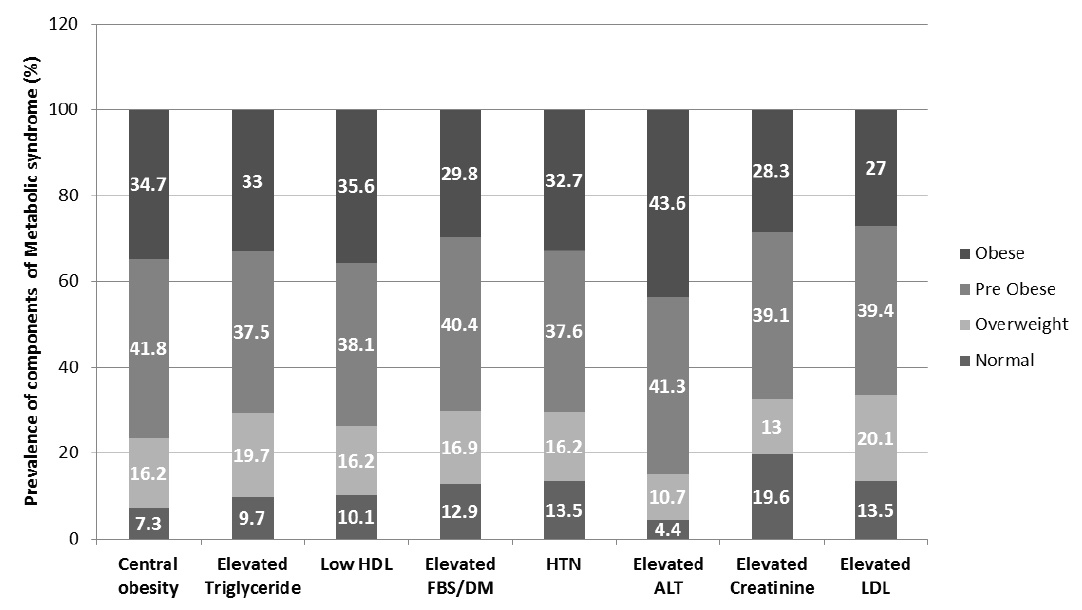
Figure 1. Prevalence of individual components of metabolic syndrome in relation to different BMI categories.
In the normal BMI subgroup, hypertension and elevated blood glucose have the highest prevalence rates at 12.9% and 13.5% respectively with central obesity being the least with 7.3% of individuals meeting the criterion for central obesity. In the overweight subgroup, high triglyceride level is the most common at 19.7% with almost equal prevalence of the other features of metabolic syndrome. In the pre-obese and obese subgroup, central obesity is the most common at 41.8% and 34.7% respectively. As the BMI increases, prevalence rates of the individual features of metabolic syndrome also increases and this was statistically significant
The mean ALT level in the Normal BMI subgroup with metabolic syndrome is 32.7 U/L (SD=18.7), 42.2 (SD=11.3) in the overweight subgroup, 47.9 U/L (SD=26.2) in the pre-obese, and 59 U/L (SD=22.4) in the obese subgroup (p<0.0001). There is an increasing trend in the mean ALT levels and there is a statistically significant difference in association with the different BMI categories.
The mean creatinine level in the Normal BMI subgroup with metabolic syndrome is 1.09 mg/dL (SD=0.65), 1.0 mg/dL (SD=0.20) in the overweight subgroup, 0.98 (SD=0.19) in the pre-obese and 1.01 mg/dL (SD=0.36) in the obese subgroup (p-value = 0.003 for the effect of interaction with BMI and metabolic syndrome).
The mean LDL level in the Normal BMI subgroup with metabolic syndrome is 128.8 mg/dL (SD=40.40), 133.7 mg/dl (SD=41.58) in the overweight subgroup, 125.5 mg/dl (SD=40.63) in the pre-obese and 128.6 mg/dl (SD=42.67) in the obese subgroup (p-value of effect of Metabolic syndrome and BMI on LDL 0.148). There is a statistically significant effect or interaction between metabolic syndrome, BMI category and LDL levels (Table 4).
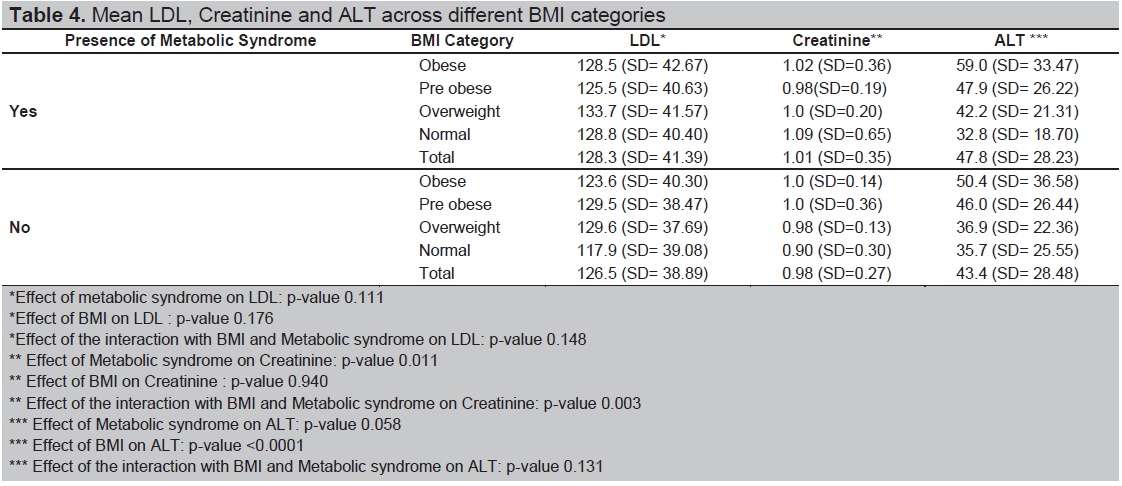
Table 4. Mean LDL, Creatinine and ALT across different BMI categories
Metabolic syndrome in this study has been defined as having 3 out of the 5 features of the disease based on cut-offs specified by the NCEP/ATP III-AHA/NHLBI (2005). Based on these criteria, the overall incidence of metabolic syndrome in this study was reported at 51% (697/1367). This prevalence is higher than reported in the previous local study of Punzalan et al., in 2004 with the reported overall prevalence of 14.2%. This wide difference in the prevalence may be explained by the different population used in the two studies, Punzalan et al., was based on a national survey and the present study was hospital-based. This prevalence is also higher than the rates reported in previous published literature which varies widely depending on the population studied which consist mainly of whites but with a considerable percentage of Asians as well.
Prevalence of metabolic syndrome in normal BMI is higher at 29.6% as compared to the study in South American Hispanics which was reported at 19% in the year 2015. Overall prevalence of the syndrome is higher in males but when it broken down to different categories there is a female predominance in the normal BMI subgroup. Central obesity is the most common feature with overall 82.9% prevalence. However, it is notable that even in patients with normal BMI, 83 subjects (7.3%) met the criteria for central obesity and this reaches as high as 41.8 % in patients with BMI of 25-29.9 kg/m2. This result is in contrast to the previous local study which showed that the most common feature in metabolic syndrome was low HDL. In terms of presence of low HDL levels based on gender specific cut-offs, 10.1% of patients in the normal BMI group met the criteria and this reaches as high as 35.6% in patients in the obese subgroup. In the normal BMI group, hypertension is the most prevalent feature of metabolic syndrome at 13.5% followed by elevated blood sugar at 12.9% and low HDL at 10.1% which is not congruent with the previous study. This may be the case since the patients in our study are mostly in the middle age and are, therefore, at higher risk to develop hypertension. Also, a significant percentage are already on medication for their dyslipidemia.
Comparing the profile of the different BMI subgroups, individuals with normal BMI presented most commonly with elevated blood pressure/presence of hypertension followed by elevated FBS/presence of DM with lesser prevalence of low HDL, elevated triglycerides and as expected, lowest prevalence of central obesity. This is in contrast to the obese population who presented with highest prevalence of low HDL and central obesity which is congruent with the result in the general population in the previous study done by Punzalan et.al. In the overweight and pre-obese subgroup, there was an almost equal prevalence of the individual features.
Among the 3 other metabolic parameters, there was a significant difference in the ALT levels in relation to the different BMI categories wherein there is an increasing trend in ALT as BMI increases (Table 5). This present data support previous studies showing an increase in liver enzymes among those with metabolic syndrome. One of such study was done by Perera et al., in Thai adults[10] and one possible explanation that they offered for this association was presence of increased visceral adiposity, Non Alcoholic Fatty Liver disease (NAFLD) in association with hepatic insulin resistance contributing to elevation of liver markers.
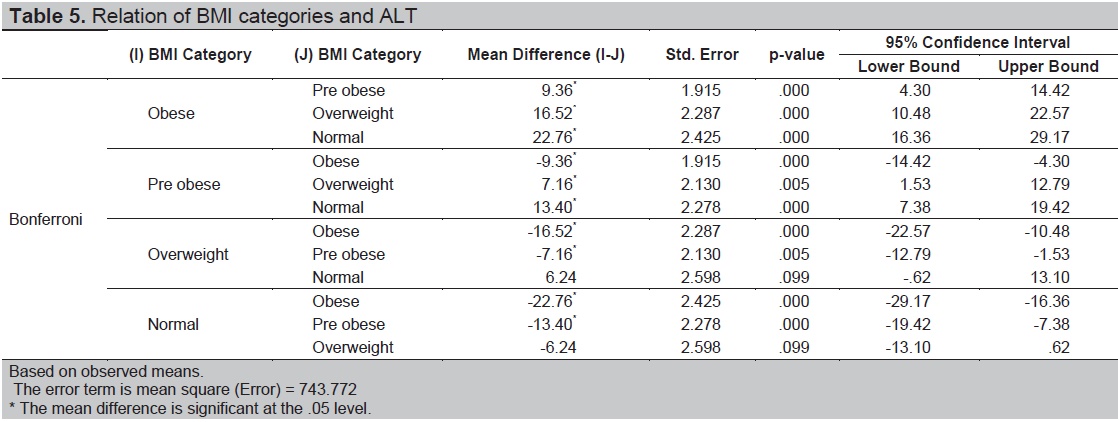
Table 5. Relation of BMI categories and ALT
In a study done by Wang et al., in 2015, they have stated that there is a positive association between higher serum creatinine levels even if within normal ranges.[11] Interaction between creatinine, presence of metabolic syndrome and BMI categories was also statistically significant in the present study however this association cannot be concluded whether it is positive or negative.
For the limitation, majority of the subjects included in this present study are at risk for metabolic abnormalities which may account for the higher prevalence rate of metabolic syndrome as compared to previous Philippine data. Subjects included and reviewed in the present study were limited only to those individuals who have access to health care facilities and only those with complete anthropometric measurements and the results of the study may not be reflective of the characteristics of the general Filipino population.
In this study, we have shown that in Filipino adults, individual components of the metabolic syndrome as defined by NCEP/ATP III-AHA/NHLBI (2005) and using the Asian cut-offs for abdominal obesity are present even in individuals with low BMI of 18.5-22.9 kg/m2 and 23-24.9 kg/m2. The presence of abnormal metabolic features such as central obesity, high triglycerides and low HDL levels even in patients with normal to slightly elevated BMI should prompt health care providers to consider nutrition counselling and weight management programs to these groups of individuals and not just be focus on individuals with higher BMI.
AcknowledgmentThe authors extend their appreciation to the staff of the Wellness Center and Obesity and Weight Management Center at St. Luke’s Medical Center Quezon City (SLMC-QC) for their assistance in the retrieval of patient records and Dr. Reandelar and Mr. Philip Salvador for their assistance and valuable inputs in the statistical analysis.
Statement of AuthorshipAll authors certified fulfillment of ICMJE authorship criteria.
Author DisclosureThe authors declared no conflict of interest.
Funding SourceNone.
[1] Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey, 1999-2016. https://www.cdc.gov/nchs/data/nhanes/survey_content_99_16.pdf.