Cognitive impairment is a global public health concern as the number of older population is rising. In 2014, 489,000 older Filipinos were estimated to have dementia.[1] It is also in the elderly where the prevalence of Type 2 diabetes mellitus peaks, and thus in the past decade, it has been implicated in the development of cognitive impairment. A meta-analysis by Cheng et al., showed that subjects with Type 2 diabetes, had a higher risk for Alzheimer’s disease, vascular dementia and mild cognitive impairment (MCI).[2] Using Montreal Cognitive Assessment (MoCA) tool, MCI was reported to have a prevalence of 31.5% and 32.7% in Polish and Korean patients with type 2 diabetes, respectively.[3],[4]
A range of vascular, metabolic and socio-demographic risk factors have been linked to the development of cognitive impairment among diabetics but these factors differed from one study to another. High HBA1c, high systolic blood pressure, high triglycerides, low high-density-lipoprotein (HDL),[5],[6] non-HDL cholesterol,[7] presence of diabetic retinopathy,[3],[8] peripheral neuropathy[6] and nephropathy,[9] age, educational background,[3],[4] increased total body fat mass and central adiposity[10] were associated with worse cognitive performance. In contrast, two studies showed that dyslipidemia, specifically total cholesterol was protective.[8],[11] Yaffe et al., showed that a hypoglycemic event had a two-fold increased risk for developing dementia.[12]
The spectrum of pathologic cognitive decline ranges from pre-clinical state to dementia with MCI as the intermediate clinical state. The International Working Group on Mild Cognitive Impairment defined the criteria of MCI as 1) cognitive decline as evidenced by self and/or informant and/or clinician report and impairment on objective cognitive tasks, and/or evidence of decline over time on objective tasks; 2) preserved activities of daily living (ADL); and 3) does not meet Diagnostic and Statistical Manual of Mental Disorders (DSM) IV, International Classification of Diseases (ICD) 10 criteria for a dementia syndrome.[13] In contrast to dementia, MCI does not interfere with ADL. Half of patients with MCI have an increased risk of developing dementia in 5 years with an estimated annual conversion rate of 10-15%.[14] On the other hand, up to 44% of patients with MCI at their first visit are estimated to return to normal after a year.[15]
Several screening tools are available for detecting cognitive impairment. The Montreal Cognitive Assessment (MoCA) was developed as a 30-point, 10-minute test that evaluates visuospatial and executive function, orientation, language, attention and recall. It is more sensitive (90% vs 18%) than MMSE in detecting mild cognitive impairment with a specificity of 87%.[16] Locally, Dominguez et al., have adapted and validated the Montreal Cognitive Assessment-Philippines (MoCA-P) version. The Filipino version has an excellent internal consistency (Cronbachs α = 0.938).[17] A cutoff score of ≤21 was shown to have better sensitivity (83.5%) in detecting probable mild Alzheimer’s disease without sacrificing specificity (72.3%). Two points are added to the total score if subjects have education less than 7 years.[18]
Cognitive performance can be affected by anxiety and depression, hence, it is important to exclude these disorders as confounders. The Hospital Anxiety and Depression Scale (HADS) is a 14-item self-assessment questionnaire designed to identify probable cases of anxiety and depressive disorders among medically-ill patients. The Hospital Anxiety and Depression Scale – Pilipino (HADSP) version has been validated locally. An optimal cut-off score of 11 is recommended for Filipinos with a sensitivity of 75%, specificity of 70%, and positive predictive value of 75%.Cognitive performance can be affected by anxiety and depression, hence, it is important to exclude these disorders as confounders. The Hospital Anxiety and Depression Scale (HADS) is a 14-item self-assessment questionnaire designed to identify probable cases of anxiety and depressive disorders among medically-ill patients. The Hospital Anxiety and Depression Scale – Pilipino (HADSP) version has been validated locally. An optimal cut-off score of 11 is recommended for Filipinos with a sensitivity of 75%, specificity of 70%, and positive predictive value of 75%.[19]
The critical element in differentiating MCI from dementia is determining independence in ADL. The Alzheimer’s Disease Association of the Philippines Guidelines 2014 recommends the use of Adapted Functional Activities Questionnaire (A-FAQ) to assess functional impairment with a Class IIB evidence. This scale has been translated and used in local studies. The optimal cut-off score of <6 has a sensitivity of 80.3%, specificity of 87.0%, and 84.7% classification accuracy in identifying patients with impairment in instrumental activities of daily living.[1]
Although diabetes control has been a mainstay in the prevention of other diabetic complications, it is difficult to apply in the prevention or delaying the progression of dementia because it is yet unknown which of the diabetes-related factors are associated with MCI. This study aims to identify factors associated with mild cognitive impairment among elderly Filipinos with Type 2 diabetes mellitus. In the lack of therapeutic options for cognitive impairment, identification of these potentially modifiable factors can help identify high-risk population that would benefit from early screening, referral to specialists and aggressive management, thus, preventing or delaying progression to dementia.
METHODOLOGYParticipants
One hundred thirty-three participants ≥60 years old with Type 2 diabetes mellitus of any duration, literate, independent in ADL, with no known neurocognitive, neurologic or psychiatric disorder, no intracranial neoplasm, infectious disease, constant alcohol or substance abuse, significant use of possible or known cognition-impairing drugs in the past 4 weeks and severe visual, hearing, mobility or motor coordination impairment were consecutively sampled from the General Medicine and Diabetes clinics of the Philippine General Hospital (PGH), a tertiary government hospital, from August 2016-May 2017. The sample size was estimated based on the percentage of MCI in patients with and without nephropathy, 24% and 6.5% respectively, and percentage of diabetic patients with nephropathy, that is 35%,6 with level of significance set at 5% and power of 80%. A written informed consent was obtained from each participant.
Assessment of Anxiety, Depression, Functional Independence and Mild Cognitive ImpairmentEligible participants answered the Hospital Anxiety and Depression Scale–Pilipino (HADS-P) and the interviewer-guided Adapted Functional Activities Questionnaire. A score of <11 and <6 respectively, were used to define absence of anxiety and depression and functional independence on instrumental activities of daily living. The Montreal Cognitive Assessment–Philippines (MoCA-P) test was administered to detect mild cognitive impairment using a cut-off score of ≤21.
Assessment of VariablesThe participants were interviewed for their age, civil status, highest level of education, duration of diabetes, smoking status, presence of hypoglycemic symptoms or capillary blood glucose (CBG) <70 mg/dl in the past 4 weeks. Comorbidities, medications used, blood pressure (BP) in the past 2 visits, HBA1c, lipid profile, creatinine, and urinalysis done in PGH in the past 30 days were obtained from the medical chart. Anthropometrics (height, weight, waist and hip circumference) and current blood pressure were taken during the second visit. Body mass index (BMI), waist-hip ratio (WHR) and mean BP were computed. For participants without recent laboratory tests, blood samples were taken after a 12-hour fast to assess lipid profile as well as HBA1c and serum creatinine. Urine samples were collected to assess proteinuria. Diabetic nephropathy was assessed by spot urine proteinuria in the absence of urinary tract infection, hematuria and exercise within 24 hours and estimated glomerular filtration rate (eGFR) as computed via the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation and was classified as no nephropathy (no proteinuria and eGFR ≥90) and with nephropathy (with proteinuria and/or decreased eGFR). Diabetic neuropathy was defined by loss of sensation in at least 2 sites on a 10-gram monofilament test. Diabetic retinopathy was assessed by funduscopic examination carried out through dilated pupils by an ophthalmologist and was classified according to the Early Treatment for Diabetic Retinopathy Study and International Clinical Diabetic Retinopathy Disease Severity Scales.[20]
Statistical AnalysisThe rate of MCI was computed as total of participants with MCI against total of participants who completed the study. Demographic and clinical data were reported through descriptive statistics using quantitative variables (mean, standard deviation, median, interquartile range) and qualitative variables (frequency, percentage). Student’s T test was used to compare normally distributed continuous variables between two groups while Chi square test was used to compare categorical variables. Prior to predictive modelling, test for collinearity and confounding were done. Multi-collinearity was assumed if the variable inflation factor was >10. Collinear variables identified were total cholesterol, low density lipoprotein (LDL) and high density lipoprotein (HDL), hence, the first two were not included in the logistic model. Confounding was considered if the change in odds ratio in the crude and adjusted logistic model was >10%. No significant confounders were identified. Univariate logistic regression analysis was done to estimate crude odds ratios. Variables were entered into an exploratory multivariate logistic regression model for mild cognitive impairment if with p-value <0.2. After stepwise backward elimination, the remaining significant variables formed the final predictive model. Hypothesis testing was done with a 95% level of significance. All data analyses were done using Stata SE version 13.
The study protocol was approved by the Technical Review Board and the University of the Philippines Manila Research Ethics Board.
A total of 226 elderly diabetics were consecutively enrolled, 53 (23%) were excluded due to probable anxiety and depression, 1 due to dependence in ADL and 2 due to past history of cerebrovascular disease. Thirty seven patients did not come back for second visit, and only 133 were included in this analysis. Table 1 summarizes the demographic and clinical characteristics of the participants. They had a mean age of 67 (4.8) years and were mostly females, married, and overweight or obese. Forty percent reached college level education. The median duration of diabetes was 12 years. The participants had relatively well-controlled diabetes, blood pressure and serum lipids.
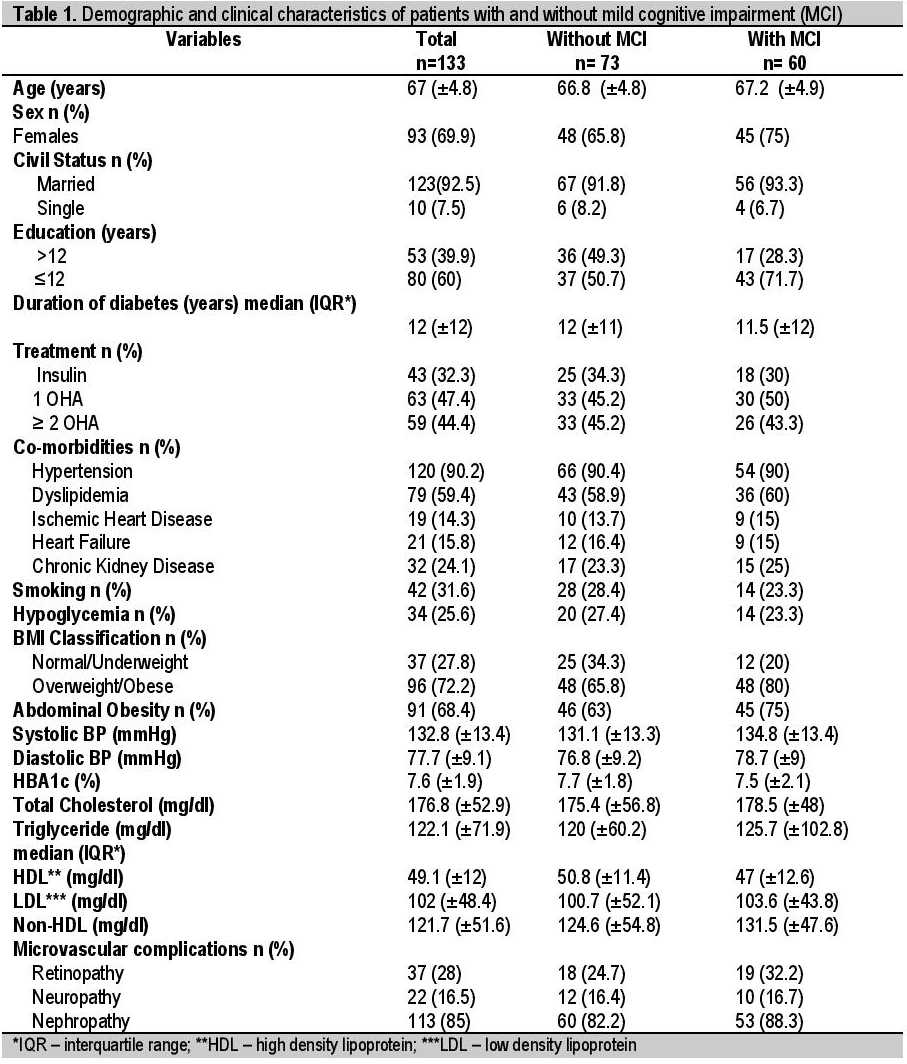
Table 1. Demographic and clinical characteristics of patients with and without mild cognitive impairment (MCI)
Using MoCA-P tool, sixty of 133 participants (45%) had MCI. Patients with MCI had significantly lower educational attainment. Other variables did not vary between the groups. The mean scores of patients with MCI reached at least 50% of perfect scores in visuo-spatial/executive function, attention and orientation. They scored poorly in language and recall.
Table 2 summarizes the results of univariate logistic regression analysis. Without correcting for other factors, increasing age, obesity, and high blood pressure appear to increase the odds of having MCI, while high HDL suggests protection although these were not significant. Having more than 12 years of education (OR 0.41, CI 0.20, 0.84, p-value 0.015) is significantly associated with lower risk of MCI. Years of education, smoking, overweight/obesity, abdominal obesity, systolic BP and triglyceride reached statistical significance (p<0.2) to be included in the multivariate logistic regression modelling.
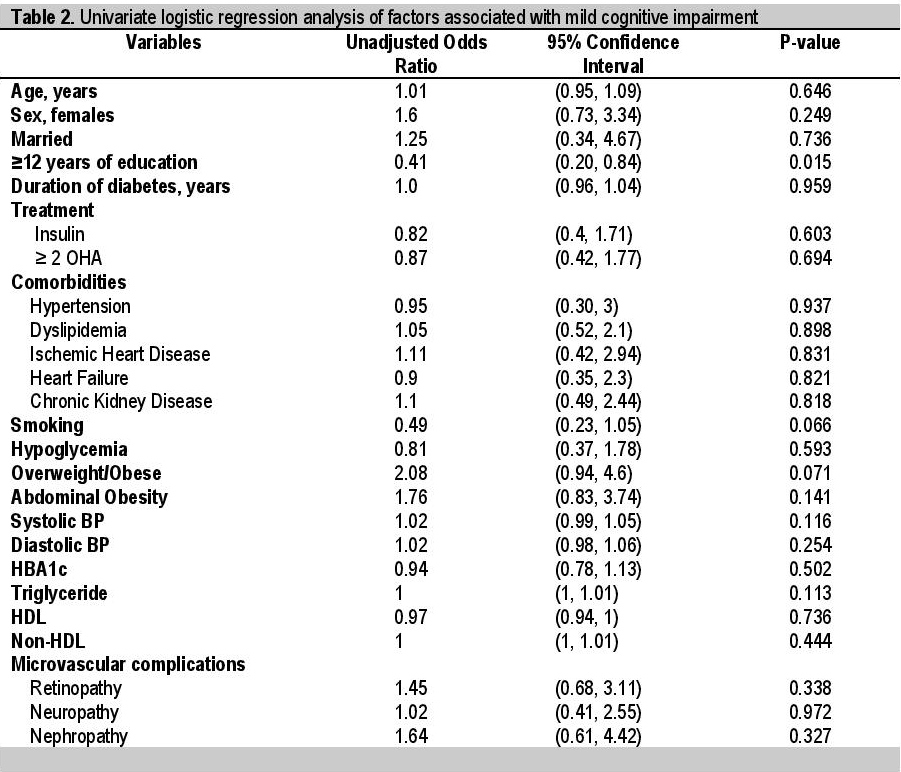
Table 2. Univariate logistic regression analysis of factors associated with mild cognitive impairment
After multivariate logistic regression analysis using stepwise backward elimination and removal of non-significant confounders and collinear variables, having more than 12 years of education (OR 0.38 CI 0.18, 0.80, p value 0.010) was the only factor left to be significantly associated with MCI.
The results of this study revealed a higher rate (45%) of MCI among elderly Filipinos compared to the 31.5%[3] and 32.7%[4] reported prevalence among Korean and Polish population respectively. Prevalence rates of MCI vary among studies due to different tools and cut-offs used or in the characteristics of the study participants involved. All these three studies used the same MCI assessment tool with locally validated cut-offs used to define MCI.
The population in the foreign studies were even older (mean age of ≥70 years) and have almost the same duration of diabetes (8-12 years) and HBA1c (7.5%) as the participants in this study. The Polish study reported even lower years of education (mean duration of 9.7 years). Considering the inherent characteristics of our population, it is also important to note that this study was conducted in a public hospital where most of the patients belong to the lower socioeconomic status, which would explain the lower educational attainment. This can possibly overestimate the rate of MCI. Although a baseline rate of MCI among the general population should be sought, this high rate among diabetics suggests that greater efforts on prevention, early detection and delaying progression to dementia are warranted.
It is interesting that during the screening process in this study, we found a rate of 23% of possible anxiety and depression among elderly Filipinos with type 2 diabetes. This post hoc data approximates 29.7% recorded in the Polish study.[4] As these can also affect patients’ adherence to treatment of diabetes, this aspect must also be looked into by the physicians and caregivers.
The domains in which our participants with MCI scored poorly include language and recall. This is inconsistent with the report from the Shanghai Aging Study and Mayo Clinic Study of Aging that diabetes is associated with worse executive function.[21] Although this could be due to the difference in the tools used, this can be seen as an advantage since effective self-care in diabetes requires a complex behavioral regimen involving executive function. An intact executive function among our patients would translate to the ability to make sustained efforts in overriding habits like dietary indiscretion and sedentary lifestyle that are challenges in the management of diabetes.
The results of the univariate logistic regression analysis showed that increasing age, high blood pressure and obesity appear to increase the likelihood of having MCI although they were not significant. These findings are consistent with other studies that showed association of these factors with worse cognitive performance.[3]-[5],[7],[19] The relation of hypertension to cognitive impairment is attributed to vascular dysfunction compromising blood and glucose supply to the brain as well as reduced clearance of substances causing oxidative stress and eventually neuronal degeneration. On the other hand, high HDL showed a trend towards decreased likelihood of MCI although, again, it was not significant. Several studies have reported the association of lower HDL and cognitive impairment.[7],[22],[23],[24] Proposed mechanisms of HDL as a negative risk factor to cognitive impairment include its anti-inflammatory properties and prevention of aggregation and polymerization of β-amyloid.[25]
After the multivariate logistic regression analysis, we have demonstrated that having more than 12 years of education is significantly associated with lower odds of having MCI. A study among Chinese elderly showed the same association. It is postulated in the cognitive reserve hypothesis that higher level of education increases neuronal plasticity and connectivity.[26] Increasing educational opportunities then can be regarded as a potential strategy in decreasing the odds of having cognitive impairment in later life.
The single result of this analysis suggests that factors associated with development of MCI could be non-diabetes related. There are several limitations in this study though. The participants in this study showed relatively well-controlled glucose, BP and serum lipids. This is a cross-sectional study in which only one HBA1c value was used and previous glycemic control measures were not considered. This could possibly explain the lack of association between HBA1c and several parameters to MCI. The stringent inclusion and exclusion criteria also prevented us from including patients who were too sick, with unstable comorbidities and worse complications, hence, our results can underestimate associations.
In conclusion, our results show that there is a high rate of MCI among elderly Filipinos with type 2 diabetes despite having relatively well-controlled disease and comorbidities. Attainment of higher years of education is significantly associated with lower odds of having MCI. Larger studies involving non-diabetic population are suggested to estimate baseline rate of MCI among Filipino elderly and investigate further association of factors.
AcknowledgmentsThe authors are grateful to all patients who participated in this study, Dr. Cecilia Jimeno, Dr. Myrna Buenaluz-Sedurante, Dr. Anna Angelica Macalalad-Josue and other physicians and the biostatistician who gave their comments throughout the study, and to the staff of the Medicine Research Laboratory who processed our laboratory specimens.
Statement of AuthorshipAll authors certified fulfillment of ICMJE authorship criteria.
Author DisclosureThe authors declared no conflict of interest.
Funding SourceThis study was a recipient of a diabetes research grant from the Philippine Society of Endocrinology, Diabetes and Metabolism.
[1] De la Vega S, Orteza G, Ledesma L. Recommendations on the diagnosis, prevention and management of Alzheimer’s disease, 2nd ed. Philippines: Alzheimer’s Disease Association of the Philippines, 2014.