Osteonecrosis of the Jaw and Bilateral Atypical Femoral Fracture Both Occurring During Treatment for Osteoporosis: A Case Report
Edelissa Payumo, Beinjerinck Ivan Cudal, Thelma Crisostomo
Edelissa F. Payumo, MD
Section of Endocrinology, Diabetes and Metabolism,
Department of Medicine, Makati Medical Center,
No. 2 Amorsolo Street, Legaspi Village, Makati City, 1229, Philippines
Tel. No.: +632-888-8999
E-mail: edspayumo@gmail.com
ORCID: https://orcid.org/0000-0002-8384-6874
e-ISSN 2308-118x
Printed in the Philippines
Copyright © 2018 by the JAFES
Received May 4, 2018. Accepted July 31, 2018.
Published Online First: September 12, 2018.
Osteonecrosis of the jaw (ONJ) and atypical femoral fracture (AFF) are rare potential adverse effects of bisphosphonates and RANKL antibody therapy. The pathogenic mechanisms of both conditions are known to be independent of each other. Here, we report both conditions sequentially occurring in the same patient.
An 81-year-old, obese, diabetic, female was admitted due to hypertensive urgency and persistent jaw pain after tooth extraction. The patient has postmenopausal osteoporosis for fourteen years and was on intermittent, unsupervised treatment with alendronate, denosumab and ibandronate. Upon presentation, the patient was noted with tenderness intraorally of tooth number 35 periapical region. This was associated with elevated erythrocyte sedimentation rate and C-reactive protein. Imaging study showed presence of bony sclerosis which represent a sequestrum in the molar area of the left hemi-mandible. Antibiotic infusion and excision and debridement of left posterior mandible were done. Histopathologic finding was consistent with a diagnosis of osteonecrosis of the jaw. The same patient, upon review, had suffered sequential fracture of both femurs during the eighth and eleventh year of treatment with antiresorptive agents. The fractures were transverse, non-comminuted, at the proximal femoral shaft. Each occurred after a minor trauma and was managed with open reduction and internal fixation. Both fractures were consistent with atypical femoral fractures.
ONJ and AFF can occur both in the same patient during prolonged treatment with bisphosphonates and denosumab and may suggest a common pathogenic mechanism.
Keywords: osteonecrosis of the jaw, subtrochanteric fracture, osteoporosis
Osteoporosis is being recognized as a growing health problem due to the aging population. Oral nitrogen-containing bisphosphonates such as alendronate and ibandronate, and human monoclonal antibody to the receptor activator of nuclear kappa B ligand (RANKL), denosumab are pharmacologic therapies for osteoporosis. Both agents have been shown to reduce the incidence of vertebral and non-vertebral (except ibandronate) fracture in patients with osteoporosis.[1] These drugs affect osteoclast function and formation and therefore are powerful inhibitors of bone resorption. Clinical trials have shown favorable safety and benefit profile of these antiresorptive agents.[2],[3]The use of bisphosphonates and denosumab, however, has been linked to cases of osteonecrosis of the jaw (ONJ) and atypical femoral fracture (AFF).
AFF and ONJ are individually recognized as rare serious adverse complications of antiresorptive therapy. The incidence of ONJ in patients with osteoporosis is estimated to be between 1/10,000 and 1/100,000.[4] Atypical femoral fracture, on the other hand, occurs in 1.8/100,000 person- years in patients treated with bisphosphonates for two years and up to 113/100,000 years when treatment is extended to 8-9.9 years.[5] The pathogenic mechanisms of both conditions are known to be independent of each other. We report a case of postmenopausal osteoporosis treatment complicated by both bilateral AFF and ONJ.
CASEAn 81-year-old, Asian, female presented with persistent jaw pain after tooth extraction in 2016. The patient was a diagnosed case of postmenopausal osteoporosis since 2002, with a lumbar bone densitometry T score of -3.7. She had been on intermittent treatment with alendronate in 2002, 2007 and 2009-2013. Thereafter, she was given denosumab every 6 months from 2014-2016 and unknown to the primary physician, she also took ibandronic acid once a month for the past five months prior to presentation as prescribed by another physician.
For the past two years prior to her admission, the patient had intermittent toothache in the left inferior molar described as boring in character. She was previously advised to have tooth extraction by her dentist but did not consent and resolved with analgesics and antibiotics. Two weeks prior to admission, however, the patient had severe toothache prompting her to undergo tooth extraction. A week after, she developed more severe pain on the affected area now associated with swelling and lymphadenopathy.
The same patient suffered fracture of both femurs on two separate occasions. First femoral fracture occurred in 2010 after patient accidentally slipped. The fracture was closed complete displaced at the proximal, mid femoral shaft, left (Figure 1). The second fracture occurred three years after (2013), also after a similar trauma. This was described as complete, closed, displaced on the proximal third of the right (Figure 2). Both fractures were managed with open reduction and internal fixation with intramedullary nailing of the femur.

Figure 1. Radiograph of the first fracture of the patient on the left femur taken one year after open reduction and internal fixation.

Figure 2. Radiograph of right femoral fracture, the second fracture of the patient, showing transverse fracture of the proximal femoral shaft. Also shown is the “beaking” (arrow) of lateral cortex at the fracture site as well as cortical thickening.
Other comorbidities of the patient include hypertension for more than 10 years, type 2 diabetes mellitus for 10 years, fairly controlled with glycosylated hemoglobin of 7.1%, and chronic kidney disease stage 3B secondary to DM nephropathy. Review of other medication of the patients include: aliskerin, verapamil, carvedilol, valsartan/HTCZ, spirinolactone, epoetin Beta, voglibose, sitagliptin, and insulin glargine. The patient was also previously on rosiglitazone and pioglitazone for five years until 2007. The patient’s medications were prescribed by different physicians managing her comorbidities. The patient has no history of radiation therapy to the craniofacial region.
The patient was initially admitted due to hypertensive urgency with blood pressure of 200/100 mm Hg, triggered by the severe toothache. She was obese with a body mass index of 31.2 kg/m2. On examination, there was note of tenderness intraorally of tooth number 35 periapical region, palpable nodule periapical region tooth 35, no pus, no mandibular swelling (Figure 3). Other systemic findings were normal.

Figure 3. Preoperative photo of left mandibular area showing exposed bone, erythema and swelling of prior tooth extraction site.
On laboratory examination, the patient had normal complete blood count, elevated erythrocyte sedimentation rate (75 mm/hr, reference range: 0-30 mm/hr), high sensitivity C-reactive protein (14.4 mg/L, reference range: <5 mg/L ), creatinine (264.32 umol/L, reference range: 49-90 umol/L), blood urea nitrogen (23.75 mmol/L, reference range: 3.5-7.2 mmol/L), intact PTH (10.12 pmol/L, reference range: <7.2 pmol/L), serum calcium (2.71 mmol/L, reference range: 2.10-2.55 mmol/L), and phosphorous (1.63 mmol/L, reference range: 0.74-1.52 mmol/L); serum 25-hydroxyvitamin D (25-OHD) was sufficient at 38.6 ng/mL (reference range > >30 ng/mL).
Non-contrast computed tomography of the mandible showed presence of bony sclerosis seen in the molar area, medial to site of the recently extracted tooth in the left hemi-mandible, which represent a sequestrum (Figure 4).
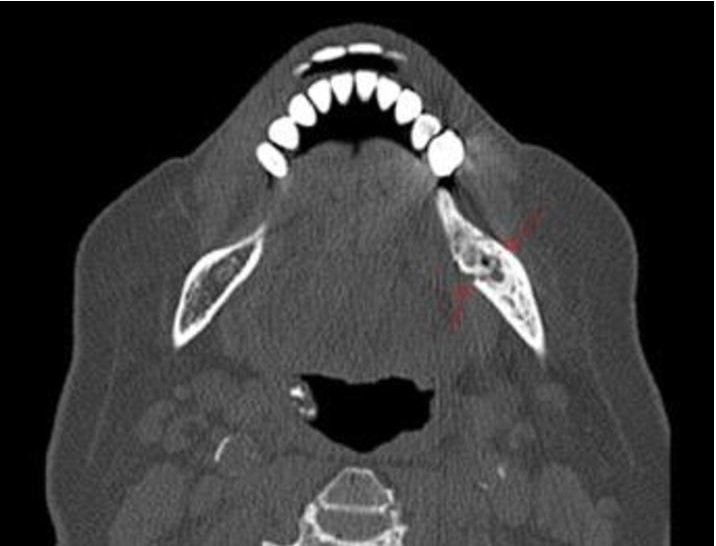
Figure 4. Non-contrast computed tomography scan (axial view) of the mandible. Bony sclerosis is seen in the molar area, medial to the site of the recently extracted tooth in the left hemimandible. Within the sclerosis, there is a lytic area (arrows) containing a focal osseous structure which may represent a sequestrum.
A multidisciplinary team including Oral and Maxillofacial Surgeon, Otorhinolaryngology and Head and Neck Surgeon, Endocrinologist, Cardiologist, Anesthesiologist, Infectious Disease Specialist and Nephrologist managed the patient. The blood pressure, blood glucose and pain of the patient were controlled medically. The patient was also given intravenous antibiotics. Excision and debridement of left posterior mandible were done with a finding of necrotic bone, described as dark in color. Histopathology reported acute and chronic inflammatory cells around necrotic bone fragments mixed with colonies of bacteria. The patient tolerated the procedure well and was discharged on the fourth post-operative day. She was placed on a drug holiday.
The American Society of Bone and Mineral Research (ASBMR) revised the diagnostic criteria for AFF in a published report in 2014.[5] AFF can be recognized if the fracture is located at femoral diaphysis between distal part of the lesser trochanter and proximal part of the supracondylar flare and satisfies at least four of five major features (Table 1). AFFs appear to be more common in patients who have been exposed to long-term bisphosphonates, usually more than three years, while risk for AFFs decline with cessation of bisphosphonate treatment.[5] Additional risk factors recognized but not consistent in studies were prior low-energy fracture, glucocorticoid therapy for more than six months, active rheumatoid arthritis, serum 25-hydroxyvitamin D (25-OHD) concentration below 16 ng/mL, female gender, younger age, diabetes and use of proton-pump inhibitor.[5],[6] The pathogenesis of AFF is also still not fully understood but is also thought to be related to altered bone remodeling by antiresorptive agents which is supposed to repair microcracks formed by mechanical stresses. Long-term decrease in bone turnover also leads to deterioration of mechanical properties of bone tissue.

Table 1. American Society for Bone and Mineral Research (ASBMR) Task Force 2013 Revised Case Definition of Atypical Femoral Fractures (AFFs)
The femoral fractures reported in the case satisfied all the major criteria for AFF by ASBMR (Table 1) and most of the minor criteria including generalized increase in cortical thickness of the femoral diaphysis, bilateral complete femoral diaphysis fractures and delayed fracture healing. The first AFF of the patient occurred after intermittent use of alendronate for five years. Given the high-risk for occurrence of osteoporosis-related fracture, bisphosphonate treatment was continued until the second fracture being now recognized as AFF and a complication of bisphosphonate. The earliest atypical femoral fracture reported with bisphosphonate use for osteoporosis was after 1.5 years with risk increases with longer duration of treatment.[7] Aside from bisphosphonate use, additional risk factors for AFF present in the patient are female gender and diabetes. There is also note of increase incidence of AFF among Asians.[7] Treatment recommendation by ASBMR for AFF includes discontinuation of bisphosphonates, adequate calcium and vitamin D supplementation, limitation of weight-bearing through the use of crutches or a walker for patients with minimal pain, prophylactic nail fixation and therapy with teriparatide.[6]
ONJ is characterized by an exposed necrotic bone in the maxillofacial region persisting for at least eight weeks despite appropriate therapy in a patient with exposure to potent antiresorptive or anti-angiogenic agents with no history of radiation therapy to craniofacial region.[4] Although the pathogenesis of ONJ is still unclear, it is thought that the antiresorptive agents by altering bone remodeling as well as by their antiangiogenic property, in combination with trauma such as a tooth extraction or inflammation/infection from periodontal or periapical disease can lead to bone necrosis.[4]
The risk of ONJ among osteoporotic patients exposed to bisphosphonates or denosumab is very low, but significantly increases over time to 0.21% from a baseline of 0.1% after four years or more of exposure to bisphosphonates.[4] Dentoalveolar surgery is a major risk factor for developing medication-related ONJ. Other risk factors include dentures, preexisting dental disease, corticosteroid use and co-morbidities such as anemia and diabetes.[4] Risk factors for the development of ONJ in the patient include at least nine years of treatment with antiresorptive agents as well as dental extraction.
Diabetes was also reported to be 58% prevalent among patients with medication-related ONJ with presence of diabetic nephropathy even increasing the risk further.[8] The presence of pain, swelling, presence of sequestrum on radiograph further strengthen the diagnosis of ONJ. Surgical resection of necrotic bone, antibiotic therapy and pain control were in congruence with the recommended stage-specific treatment strategies by the American Association of Oral and Maxillofacial Surgeons.[4] Hyperbaric oxygen as adjunct to treatment of ONJ has been shown to improve healing but there is not enough evidence to recommend this treatment modality.[4] Discontinuation of antiresorptive therapy until soft tissue closure has occurred should also be considered, though there is limited data to support this. Preventive measures against ONJ in patients on antiresorptive therapy involves maintenance of excellent oral hygiene and cessation of smoking and should be emphasized.[4] Invasive dental procedures such as dental extractions or implants should be avoided, if possible.
Although the pathogenic mechanisms of ONJ and AFF differ, a common pathogenesis for both explains that the jaw bone and lateral cortex of subtrochanteric area of femur endure more mechanical stress compared to other bones and therefore may be prone to damage and demand repair through bone remodeling. Bisphosphonates and denosumab by inhibiting osteoclast function and bone resorption, impair this bone remodeling process.[7] Occurrence of one of the two serious complications of antiresorptive therapy should prompt reconsideration of the risks and benefits of further antiresorptive treatment. Drug holiday should also be observed to minimize side effects in long-term treatments. Most experts and guidelines recommend a drug holiday after 4-5 years of treatment with bisphosphonates in patients at moderate risk of fracture, and after 10 years for high-risk patients.[1] Bisphosphonates accumulate in bone with some persistent anti-fracture efficacy after therapy is stopped. In contrast, the anti-resorptive effect of denosumab wears off rapidly after it is stopped, hence, drug holiday for this agent has not been defined.
The occurrence of both ONJ and AFF in one patient is very rare. In our literature search, this is only the fifth published report of ONJ and AFF occurring in the same patient. Of the previous four cases reported, three were Oriental women[9],[10],[11] and one a Caucasian woman.[12]
Another important lesson learned from this case is that all doctors must do regular review of medications. Our patient was prescribed with two antiresorptive medications at the same time, which could have increased the risk for the side effect of the treatment particularly the ONJ. Open and complete communication among health care professionals and between the patient and health care professionals must be maintained. The patient should be warned about the possible side effects of treatment but be assured that proper screening and follow up can minimize his/her risk. Early dental consultation and dental preventive measures prior to initiation of antiresorptive therapy is recommended.[4]
ONJ and AFF can both occur in the same patient during prolonged treatment with bisphosphonates and RANK-L inhibitor and may suggest a common pathogenic mechanism. Occurrence of any of these two complications should prompt reconsideration of the risks and benefits of further antiresorptive therapy. Patient education and vigilance on the occurrence of symptoms and risk factors such as thigh pain, trauma, dental extraction as well as emphasis on follow up care should be observed in all patients receiving long-term antiresorptive drugs. This case further emphasized that bisphosphonates should be given for a limited period to avoid these consequences, particularly in patients with additional risk factors.
Ethical ConsiderationThe authors submitted a letter of permission from the Makati Medical Center Institutional Review Board (MMCIRB) to publish the case.
Statement of AuthorshipAll authors certified fulfillment of ICMJE authorship criteria.
Author DisclosureThe authors declared no conflict of interest.
Funding SourceNone.
[1] Cosman F, De Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporosis Int. 2014;25(10):2359-81. PubMed PubMed Central CrossRef
[2] Black DM, Schwartz AV, Ensrud KE, et al. Effects of continuing or stopping alendronate after 5 years of treatment. The Fracture Intervention Trial Long-term Extension (FLEX): A randomized trial. JAMA. 2006;296(24):2927-38. PubMed CrossRef
[3] Cummings SR, San Martin J, McClung MR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361(8):756-65. PubMed CrossRef
[4] Ruggiero SL, Dodson TB, Fantasia J, et al. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw – 2014 update. J Oral Maxillofac Surg. 2014;72(10):1938-56. PubMed CrossRef
[5] Shane E, Burr D, Abrahamsen B, Adler R, et al. Atypical subtrochanteric and diaphyseal femoral fractures: Second report of a Task Force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014; 29(1):1–23. PubMed CrossRef
[6] Hu CJ, Renn JH, Yang SW, Lin KC. Atypical femoral fractures in a patient with continuous decreasing BMD after only 1.5 Years of bisphosphonate treatment. Open Journal of Rheumatology and Autoimmune Diseases. 2014;4(1), Article ID: 42344 CrossRef
[7] Wąsowski M and Tałałaj M. Osteonecrosis of the jaw and atypical femoral fractures as complications of antiresorptive therapy. Post N Med 2017;XXX(1):43-8. http://www.pnmedycznych.pl/wp-content/uploads/2017/02/pnm_2017_043_048.pdf
[8] Peer A, Khamaisi M. Diabetes as a risk factor for medication-related osteonecrosis of the jaw. J Dent Res. 2015;94(2): 252-60. PubMed PubMed Central CrossRef
[9] Chiu WY, Lee JJ, Tsai KS. Atypical femoral fractures shortly after osteonecrosis of the jaw in a postmenopausal woman taking alendronate for osteoporosis. J Clin Endocrinol Metab 2013;98(4):E723-6. PubMed CrossRef
[10] Won Y, Lim JR, Kim YH, Song HK, Yang KH. Atypical femoral fracture combined with osteonecrosis of jaw during osteoporosis treatment with bisphosphonate. J Bone Metab. 2014;21(2):155-9. PubMed PubMed Central CrossRef
[11] Kim JE, Yun M, Lim SK, Rhee Y. Concurrent bisphosphonate-related bilateral atypical subtrochanteric fractures and osteonecrosis of the jaw on bone scintigraphy. Clin Nucl Med. 2015;40:450-2. PubMed CrossRef
[12] Sánchez A, Blanco R. Osteonecrosis of the jaw (ONJ) and atypical femoral fracture (AFF) in an osteoporotic patient chronically treated with bisphosphonates. Osteoporos Int. 2017;28(3):1145-7. PubMed CrossRef
Authors are required to accomplish, sign and submit scanned copies of the JAFES Author Form consisting of: (1) Authorship Certification, that all the requirements for authorship have been met by each author, and that the final version of the manuscript has been read and approved by all authors; (2) the Author Declaration, that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere; (3) the Statement of Copyright Transfer [accepted manuscripts become the permanent property of the JAFES and are licensed with an Attribution-Share Alike-Non-Commercial Creative Commons License. Articles may be shared and adapted for non-commercial purposes as long as they are properly cited]; and the ICMJE form for Disclosure of Potential Conflicts of Interest. For original articles, authors are required to submit a scanned copy of the Ethics Review Approval of their research as well as registration in trial registries as appropriate. For manuscripts reporting data from studies involving animals, authors are required to submit a scanned copy of the Institutional Animal Care and Use Committee approval. For Case Reports or Series, and Images in Endocrinology, consent forms, are required for the publication of information about patients; otherwise, appropriate ethical clearance has been obtained from the institutional review board. Articles and any other material published in the JAFES represent the work of the author(s) and should not be construed to reflect the opinions of the Editors or the Publisher.