Validity of Ankle Brachial Index using Palpation Method in Screening for Peripheral Arterial Disease in Type 2 Diabetes Mellitus Patients at a Tertiary Hospital in the Philippines
Jonathan Mercado, May Sison, Maria Princess Landicho-Kanapi, Lyza Camille Gadong
Jonathan P. Mercado, MD
Section of Endocrinology, Diabetes and Metabolism
Department of Internal Medicine, Makati Medical Center
No. 2 Amorsolo Street, Legaspi Village, Makati City, Philippines 1229
Tel. No.: +632-888-8999
E-mail: jmercado@cducm.edu.ph
ORCID: https://orcid.org/0000-0002-5785-6139
e-ISSN 2308-118x
Printed in the Philippines
Copyright © 2018 by the JAFES
Received May 25, 2018. Accepted July 30, 2018.
Published Online First: October 3, 2018.
Introduction. Peripheral Artery Disease (PAD) is a significant marker of cardiovascular disease and is prevalent but underdiagnosed. Ankle-Brachial Index (ABI) is the recommended screening test for PAD. However, not all clinics have a Doppler ultrasound. ABI by palpation offers a more feasible alternative.
Objective. This study aims to determine the validity of ABI measurement by palpation method in the screening of PAD.
Methodology. This prospective validation study utilized a cross-sectional analytic design. Three physicians performed the ABI by palpation method and their result was compared to the Doppler ABI. The accuracy indices for validation was computed per physician conducting the ABI by palpation and also as an average of all 3 palpation method readings. During the course of sampling, there were no patients with severe PAD found during the prospective period.
Results. The accuracy of Ankle Brachial Index using Palpation method yielded the following ranges, sensitivity between 63.16 % - 73.68%, specificity of 94.06% - 98.02%, PPV within 85.37% - 95.45%, and NPV within 80.73% - 86.84% in predicting PAD. The accuracy indices were clinically acceptable. Meanwhile, the raters’ usage of Ankle Brachial Index using Palpation method demonstrated a substantial agreement with ABI by Doppler Method performed by the angiologist (Cohen Kappa >0.60).
Conclusion. The ABI by palpation is a good screening tool for PAD, but the person performing it must be adequately trained to do the procedure. The procedure is affordable and convenient, and should be done routinely during clinic visits in the physical examination of patients with known risk factors for PAD.
Keywords: diabetes mellitus, ankle-brachial index, palpationBurden of Peripheral Arterial Disease
Peripheral Arterial Disease (PAD) in the lower extremities is the narrowing or blockage of the vessels that carry blood from the heart to the legs.[1] It is primarily caused by atherosclerosis, the buildup of fatty plaque in the arteries.[2] The third most prevalent form of atherosclerotic cardiovascular disease, PAD is a disease of high human and social impact.[3]
In a prevalence study conducted by Sang Youl Rhee et al., in several Asian countries, including the Philippines, the prevalence of PAD in high risk Asian type 2 diabetes patients is 17.7%.[4] The role of risk factors such as diabetes mellitus, tobacco use, older age, hypertension, and hypercholesterolemia, and others, with the development of PAD have been well-defined.[5],[6],[7]
In a 10-year prospective study by Criqui et al., PAD patients with and without a history of cardiovascular disease had a significantly increased risk of dying from any cause or as a result of cardiovascular disease or coronary artery disease than age-matched controls. All-cause mortality was 3.1 times greater and cardiovascular disease mortality was 5.9 times greater in patients with PAD than in those without PAD.[8]
Significance of the study
With the increased morbidity and mortality resulting from PAD, screening for high risk population like in patients with diabetes is recommended. Early identification of PAD will reduce the severity of the disease and the possibility of amputations.[3] Preventative measures, such as promoting risk factor reduction, are more cost-effective than the surgeries and rehabilitation required to treat advanced PAD.[3]
However, most physicians do not have a doppler ultrasound in the clinic. This makes it hard for patients to be tested, especially those in the underserved rural areas who have difficult access to diagnostic centers capable of doing the ABI. In our local setting, the latest 2010 Philippine Statistics Authority survey showed that of the 92.3 million population in the Philippines, more than half or 54.7% of the total population lived in the rural areas.[9]
ABI by palpation offers several advantages over the standard doppler ABI such that it is more affordable, can be done at any time in the clinic, and eliminates the need for specialized equipment. Most of these advantages over the standard doppler ABI eliminate the limitations of diabetic patients not being able to have the ABI screening done, especially those who live in the rural areas.
ABI by doppler as a reference standard
Measurement of the ABI by using a doppler ultrasound is the first and primary method for establishing the diagnosis of PAD.[10] An ABI 0.90 using the doppler ultrasound has been demonstrated to have high sensitivity and specificity for the identification of PAD even compared with the gold standard of invasive arteriography.[10] In fact, the American Heart Association and American College of Cardiology (AHA/ACC) 2016 guidelines state that studies for anatomic imaging assessment such as computed tomography angiography, magnetic resonance angiography, or invasive arteriography are generally reserved for those in whom revascularization is being considered.[11] These procedures especially the invasive arteriography, are more expensive, require trained specialists who may not be readily available, and the dye used in the procedure confers additional risk for kidney damage in the already at-risk individuals for kidney disease. The resting doppler ABI is the initial diagnostic test for PAD and may be the only test required to establish the diagnosis and institute guideline-directed management and therapy.[11]
Review of related literature
At the time of this study, we found only 2 related articles in PubMed. In the study done by Borreros II et al., the ABI by palpation had a sensitivity of 90.4%, specificity of 86.1%, positive predictive value of 76.5%, and a negative predictive value of 94.7%.[12] The researcher did the screening of patients for risk factors and the palpation ABI. Majority of subjects, 85%, were hypertensive, while 23% were diabetic.
Another study in Italy done by Migliacci et al., utilized a more complex methodology by letting 24 physicians screen different sets of 10 patients by palpation against the standard doppler ABI.[13] Sensitivity of the palpation method was 88%, specificity 82%, positive predictive value 18%, negative predictive value 99%. There were no data regarding inter-reader agreement of findings.
General objective
To determine the validity of ABI measurement by palpation method in the screening of PAD.
Specific objectives
- To determine the validity of the ABI measurement by palpation using Doppler method as reference standard in the detection of the various degrees of PAD using the following measures:
- Sensitivity
- Specifity
- Positive predictive value
- Negative predictive value
- Accuracy
- To determine the degree of agreement of the 3 ABI results by palpation method.
Study design
This is a prospective validation study utilizing a Cross-Sectional Analytic study design. This was conducted at the outpatient department of Makati Medical Center from October 2017 to December 2017.
Sampling method
This study utilized a Convenience Sampling method to achieve the minimum sample size.
Sample size
The sample size was computed using the equation:
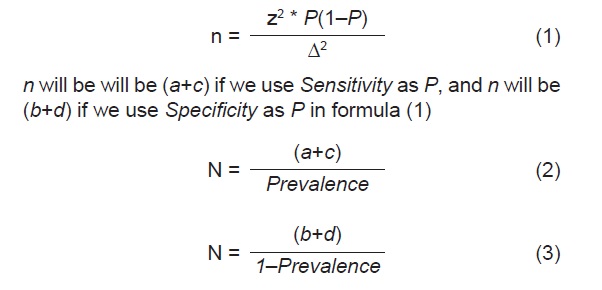
Specification on the sample size used for sensitivity and specificity study.[14]
The sample size in this study was computed as Total sample size = N
At first, the researcher managed to access the sensitivity and specificity indices from related literature as values in the equation for “P”, either sensitivity or specificity were expressed in symbol “P” as factor in the equation.
By using the usual single proportion sample size formula (Formula Step 1), the sample size is computed wherein the “P” was used, estimated at a certain precision CI at 95%, symbol Δ
After the initial sample size “n” was computed, the prevalence rate of disease was determined from the related literature. Then, using formula 2 or 3, the final Total sample size was computed “N”.
The total N was determined using either the sensitivity or specificity index.
The computed sample size, based on 95% confidence level, relative error of 10%, prevalence of PAD among at risk DM type 2 patients of 17.7% and assumed sensitivity of ABI was noted to be at 90.4% while the specificity of 86.1%. The assumed sensitivity of 90.4% and specificity of 86.1% were based on the result of the study done by Borreros & delos Santos in 2012.[12] On the other hand, the prevalence was based on the study done by Sang Youl Rhee, et al.[4]
Using the following values such as, sensitivity of 90.4%, CI at 95% precision of +/-17%, and PAD prevalence rate of 17.7%, then, the computed sample size was 68 cases. However, during the prospective sampling period, the researcher was able to collect 79 subjects, with a total of 158 ABI readings. However, the researcher made an analysis of 158 ABI readings for analysis to increase the power of the statistical inference which was above the computed minimum sample size.
Subjects
Inclusion criteria
- 18-49 years old with Diabetes Mellitus Type 2 plus at least 1 other risk factor for atherosclerosis
- 50 years old and above with Diabetes Mellitus Type 2 alone or with other risk factors for atherosclerosis
Exclusion criteria
- Single or double leg amputee
- Patients on with AV fistula or on lifetime hemodialysis
Disclosure on support from Otsuka pharmaceuticals
The Angiologist and his doppler ultrasound equipment were provided for free by Otsuka pharmaceuticals. Although the standard ABI is available in Makati Medical Center, our experience with the patients at the outpatient department is that they are mostly unable to have the test done on follow up due to financial constraints. Hence, the procedure was provided free of charge for the patients who participated in the study. No monetary compensation was given to Otsuka pharmaceuticals for the services rendered. No medications were prescribed to any patient in the course of the study since the scope of the study was purely diagnostic. If a patient was found to have PAD, the procedure result was forwarded to his attending physician so he can be started on appropriate management. All patients received a copy of their ABI results.
The physicians performing the palpation ABI
In this study, the requirement qualification for the physicians recruited to do the ABI by palpation is at a minimum general physician level, since the study application is geared towards rural area practice. The investigators, however, take into account the possibility of getting low inter-rater agreement score if levels of training significantly differ. As of this writing, the investigators did not find a similar study to use as reference for physician training levels to do the ABI by palpation since literature on the topic is very limited. We recruited 3 endocrinology fellows-in-training in Makati Medical Center to do the ABI by palpation since they underwent the same level of training on how to do the ABI. They all had ABI lectures with return demonstrations in their 3-day intensive training course for diabetes educators. Immediately prior to testing, they also had an hour review on how to do the procedure with the angiologist in this study.
Data collection
The study was started only after the approval of the Institutional Review Board. All diabetic patients at increased risk of PAD according to the 2016 AHA/ACC guidelines were invited to participate in the study. The researcher explained the study rationale, procedures and subjects’ extent of participation to the patients. They voluntarily signed consent forms prior to participating in the study.
The primary investigator screened patients for risk factors and past medical histories but was not involved in testing patients. Evident signs of vascular disease such as presence of AV fistula or a previous leg amputee were excluded to prevent testing bias. All raters of the ABI, 3 by palpation and 1 by doppler ultrasound were blinded of all patient data such as risk factors or previous vascular events like stroke or myocardial infarction. They were also blinded of the other party’s findings.
Upon arrival at the testing site, the patients were instructed to rest for 10 minutes. The cuff is inflated progressively to 20 mmHg above the level of flow signal disappearance and then slowly deflated to detect signal reappearance. The first detected pulse by palpation or doppler is recorded as the systolic pressure. Systolic pressures were recorded on both brachial arteries first then the dorsalis pedis and posterior popliteal arteries of both lower extremities. The ABI’s were calculated from the average of two determinations as the ratio between the highest systolic blood pressure of the ankle and the highest systolic blood pressure of the upper limbs. If there was a discrepancy in the pressure between the bilateral arms, the higher of the two systolic pressures was used.
Screening by palpation was done by 3 physicians successively, with 3-minute rest in between, then followed by the ABI by doppler ultrasound by the angiologist. Each step in all 4 assessments, was done in a separate patient cubicle to maintain privacy. The physicians and the angiologist were blinded about patient data and risk factors such as previous stroke or myocardial infarction. Only the primary investigator had access to the data. All testing physicians and the angiologist were blinded of the findings of the other party.
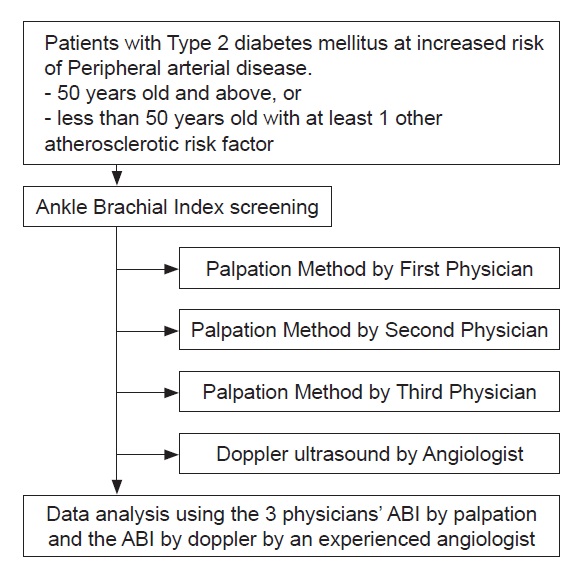
Figure 1. Study design flow.
Data management and statistical tools
Categorical data such as gender and risk factors were expressed in frequency and percentage while the continuous variables, namely, age, BMI, and length of DM, with normal distribution were described in mean and standard deviation. Also, PAD rates were computed. In testing associations between physician assessment vs gold standard, Chi square test of independence was used with p-value >0.05α were considered significant. Cohen Kappa (unweighted) with matrices of 2x2 and 5x5 were used in testing agreement between physician’s palpation method and Doppler. SPSS ver 21 was used as statistical software package.
We tested 79 subjects, with a total of 158 ABI readings. Majority, 67%, of subjects were females (Table 1). The average age of the study population was 63.51±10.53 years old. The average body mass index (BMI) was 24.42±2.29 kg/m2. The estimated years from first diagnosis of DM from recall is 7.60±5.89 years. Only 16.5% of the study population had a smoking history. The most common comorbidity was chronic kidney disease (67.09%), and the least common comorbidity in this study population were both Coronary Artery Disease and Cerebrovascular Disease.
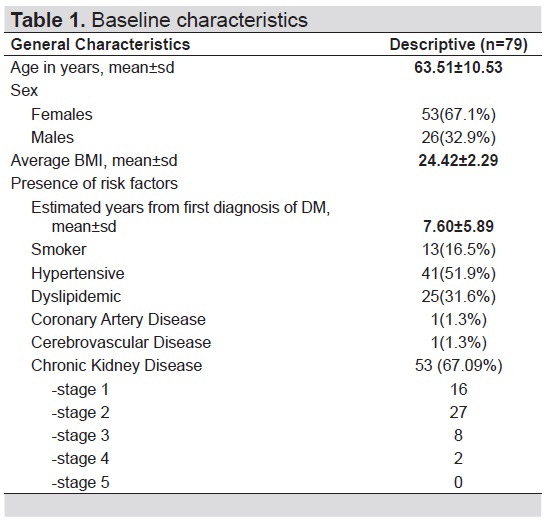
Table 1. Baseline characteristics
In this study, the prevalence of PAD in reference to the (gold) standard Doppler ABI was 24.05% Meanwhile, using the Palpation technique, the ABI PAD rates such as 20%, 20.89%, and 24.05% were based on the assessment by physicians’ 1, 2 and 3 respectively (Table 2). The test of differences in the detection rates of PAD based on the assessment by Physicians 1, 2 and 3 did not show significant independence (p=0.200), thus, implying that the three (3) physicians’ assessment of PAD using the palpation ABI were significantly consistent.
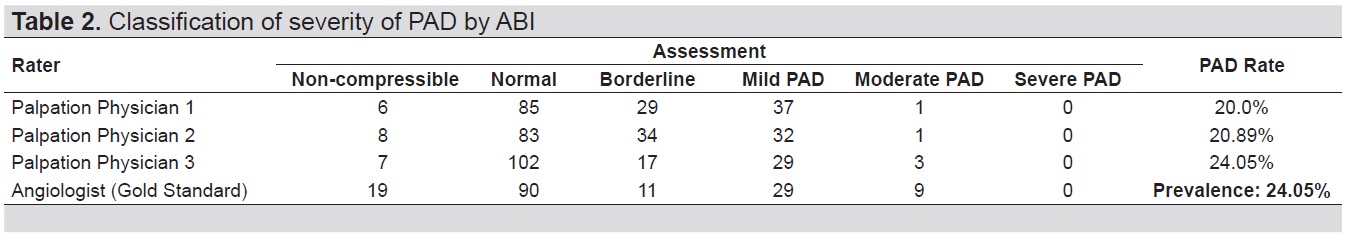
Table 2. Classification of severity of PAD by ABI
Using the palpation method (Table 3), of the 44 PAD cases detected by physician 1, 42/44 (95%) were PAD on the gold standard, 35/41 (85%) PAD detected by physician 2 which was consistent with gold standard, and 36/39 (92%) PD as detected by physician 3 were consistent with gold standard. The ranges of precision by the 3 physicians in detecting PAD when matched with the gold standard were within 85%-95%. Further analysis of PAD assessment between the physicians vs gold standard revealed that physician 1 vs gold standard yielded a Cohen kappa index of 0.755, Cohen kappa of 0.647 between physician 2 vs gold standard, and Cohen kappa of 0.636 achieved between physician 3 vs gold standard. The Cohen kappa indices between the 3 physicians and gold standard indicated that there is a good consistency or agreement between the physicians’ assessment and PAD outcome based on ABI by Doppler method angiologist.
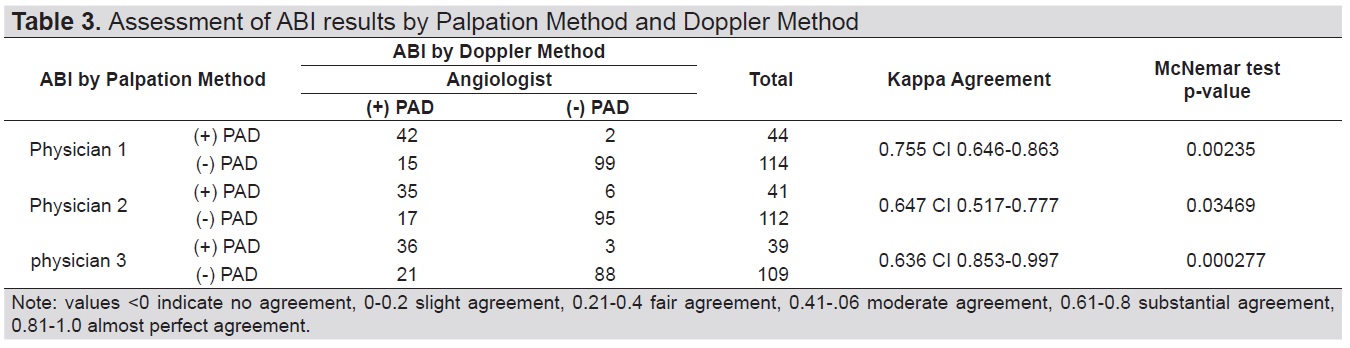
Table 3. Assessment of ABI results by Palpation Method and Doppler Method
In this study, all 3 physicians using the ABI by palpation method to screen for PAD had sensitivity, 73.68%, 67.3% and 63.16% respectively (Table 4). Specificity was at 98.02%, 94.06% and 96.7% respectively. Positive predictive value was at 95.45%, 85.37% and 92.31% respectively. And negative predictive value was higher at 86.84%, 84.82% and 80.73% respectively. Overall accuracy was at 89.24%, 84.97% and 83.78% respectively, with an average of 86.0%.
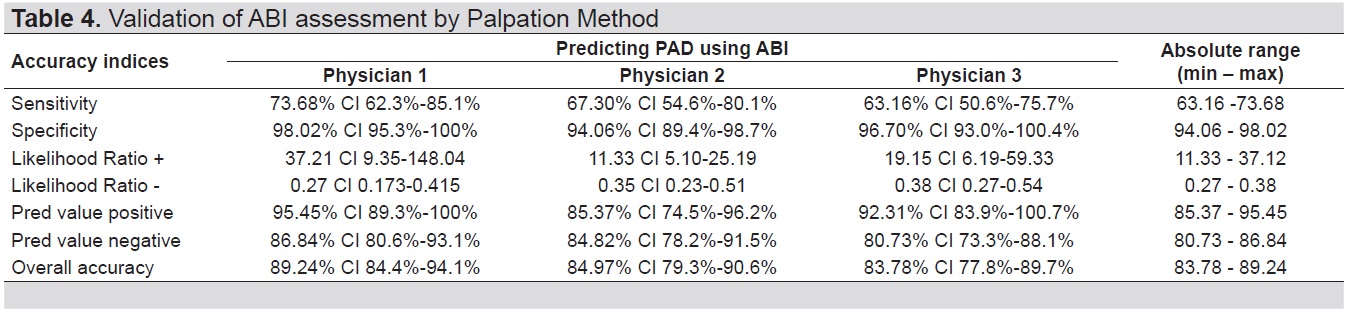
Table 4. Validation of ABI assessment by Palpation Method
Secondary analysis in Table 5 showed that physician 1’s assessment had weak correlation with angiologist findings when it comes to normal, non-compressible, and borderline (rho=0.206 (weak), p=0.068). Physician 2’s assessment has also weak association with angiologist’s assessment (rho=0.105 (weak), p=0.357). Meanwhile, physician 3’s judgement, yielded significant correlation with (rho=0.302** (weak), p=0.007) angiologist when it comes to the variations with normal, non-compressible, and borderline. Despite the effect of weak ordinal correlation on the assessment such as normal, non-compressible, and borderline, it was still noted that when it comes to presence of PAD, as shown in Table 3, there were substantial agreement between the physicians’ assessment of PAD and angiologist s gold standard. These results implied that palpation method has limitation in detecting normal, non-compressible, and borderline status of patients yet palpation method is accurate when a clear presence of PAD is detected.
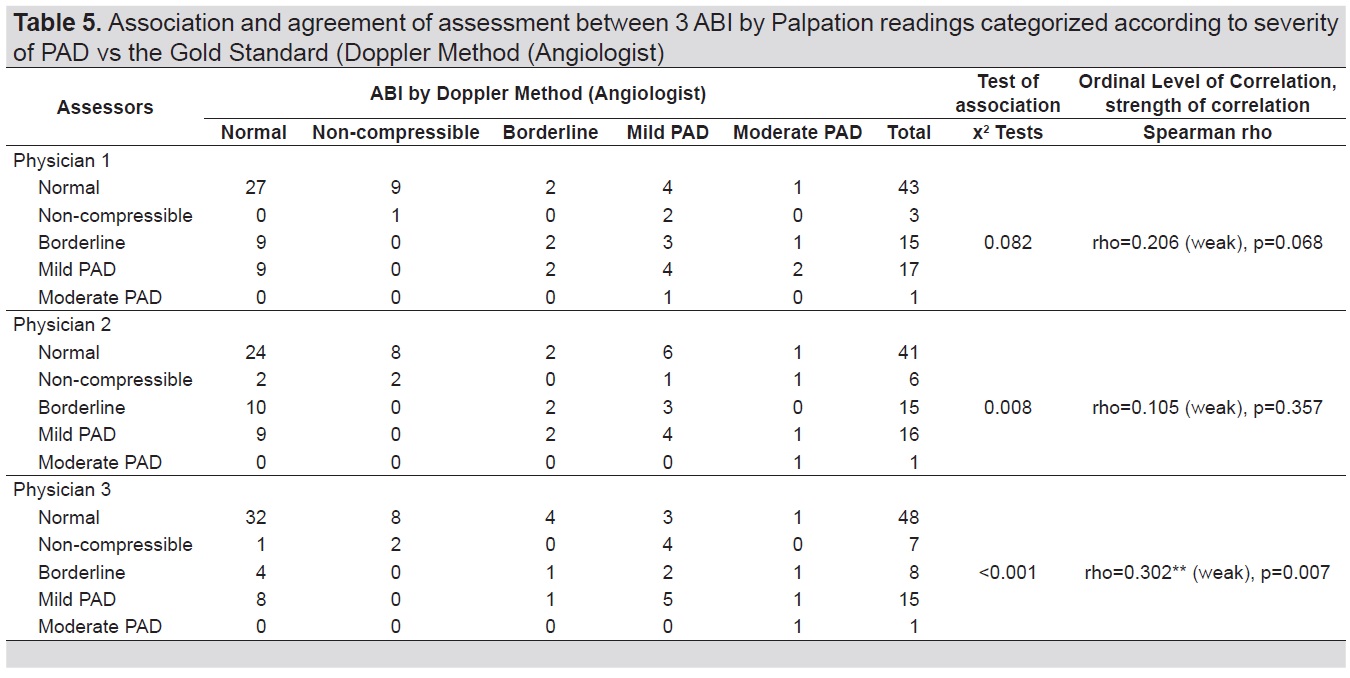
Table 5. Association and agreement of assessment between 3 ABI by Palpation readings categorized according to severity of PAD vs the Gold Standard (Doppler Method (Angiologist)
The accuracy of Ankle Brachial Index using Palpation method yielded the following ranges, sensitivity between 63.16 % - 73.68%, specificity of 94.06% - 98.02%, PPV within 85.37% - 95.45%, and NPV within 80.73% - 86.84% in predicting PAD. There is a significant difference in sensitivity of ABI by palpation amongst the 3 physicians. A possible factor is that the first physician with the highest sensitivity in testing is a second-year senior endocrine fellow while the other 2 physicians with sensitivity less than 70% are both first-year fellows. More experience and mastery of the procedure might have played a significant difference in complicated cases like in the presence of bipedal edema. Also, although the Cohen kappa indices between the 3 physicians and angiologist indicated that there is a good consistency or agreement of assessment and PAD outcome between physician and angiologist in general, note that there is a significant increase in degree of agreement between physician rater and angiologist with the first physician or the senior endocrine fellow as compared to the other two first-year endocrine fellows. Otherwise the testing conditions were the same for all 3 physicians which makes the difference largely subjective to the operator. In a previous study done by Borreros et al., where the researcher was the unblinded physician rater compared to the doppler ABI,[11] the sensitivity of palpation ABI was 90% and the specificity was 86.1%. Another similar study by Migliacci in Italy also had a sensitivity 88% and a specificity of 82%. On the other hand, the doppler ABI has a sensitivity of 79-90% and a specificity of 81-98% in various studies.[15],[16],[17]
The prevalence of PAD in this study was 24.05%. This was higher in comparison to the PAD-SEARCH Study by Rhee et al, a multi-Asian country study which included the Philippines, where the prevalence of PAD in that study was 17.7%.[4] This might be due to the population difference which is purely Filipino in this study versus a mix of different Asian populations. The higher prevalence in purely Filipino population is also reflected in the study by Borreros et al.,[11] where the prevalence of PAD was at 33.2%.
Limitations and Recommendations
There are no subjects that were found to have severe PAD and not many subjects found to have mild and moderate PAD in this study. Computing individual validation per category would result in underpowered analysis. A bigger sample population would have overcome these limitations. A bigger sample population would also possibly include patients with more severe risk factors such as a history of CAD or stroke.
There are several other limitations in this study that should be taken into consideration. One, palpation is largely subjective and is dependent on the technique and senses of the one performing the ABI. Two, the physicians performing the ABI by palpation noted that patients with pedal edema were hard to assess which might have affected their results while, on the other hand, this would less likely affect the soundwave measurement of the doppler ultrasound. Third, all patients in this study have diabetes mellitus type 2. This patient population is more likely to have arterial calcifications depending on the duration and control of the condition and this might have also affected the ABI by palpation results.
The ABI by palpation is a good screening tool for PAD but the one performing the procedure must be adequately trained to do the procedure. The procedure is inexpensive and convenient and should be incorporated into the physical examination of every clinic visit of patients at risk of PAD. This will significantly improve the specificity and negative predictive value of physical exam assessment.
This is an important clinical assessment tool especially in the developing countries like the Philippines. With the rising incidence of diabetes mellitus worldwide, the need to screen for PAD increases as well.
AcknowledgmentsThe authors would like to thank Mr. Jesse L. Batara who did all the statistical computations in the study.
Statement of AuthorshipAll authors certified fulfillment of ICMJE authorship criteria.
Author DisclosureThe authors declared no conflict of interest.
Funding SourceNone.
[1] Argyriou C, Saleptsis V, Koutsias S, Giannoukas AD. Peripheral arterial disease is prevalent but underdiagnosed and undertreated in the primary care setting in central Greece. Angiology. 2013;64(2):119-24. PubMed CrossRef
[2] Peripheral arterial disease (PAD) fact sheet. https://www.cdc.gov/dhdsp/data_statistics/fact_sheets/fs_pad.htm. Accessed July 19, 2017.
[3] Peripheral arterial disease (PAD): European population-based action plan for early diagnosis. http://www.euro.who.int/en/health-topics/Life-stages/healthy-ageing/news/news/2014/03/peripheral-arterial-disease-pad-european-population-based-action-plan-for-early-diagnosis. Accessed July 19, 2017.
[4] Rhee SY, Guan H, Liu ZM, et al. Multi-country study on the prevalence and clinical features of peripheral arterial disease in Asian type 2 diabetes patients at high risk of atherosclerosis. Diabetes Res Clin Pract. 2007;76(1):82-92. PubMed CrossRef
[5] Gallino A, Aboyans V, Diehm C, et al. Non-coronary atherosclerosis. Eur Heart J. 2014;35(17):1112-9. PubMed CrossRef
[6] Berger JS, Hochman J, Lobach I, Adelman MA, Riles TS, Rockman CB. Modifiable risk factor burden and the prevalence of peripheral artery disease in different vascular territories. J Vasc Surg 2013;58(3):673-81. PubMed CrossRef
[7] Joosten MM, Pai JK, Bertoia ML, et al. Associations between conventional cardiovascular risk factors and risk of peripheral artery disease in men. JAMA 2012;308(16):1660-7. PubMed PubMed Central CrossRef
[8] Criqui MH, Langer RD, Fronek A, et al. Mortality over a period of 10 years in patients with peripheral arterial disease. N Engl J Med. 1992;326(6):381-6. PubMed CrossRef
[9] Urban-Rural Classification. https://psa.gov.ph/tags/urban-rural-classification. Accessed July 19, 2017.
[10] Society for Vascular Surgery Lower Extremity Guidelines Writing Group, Conte MS, Pomposelli FB, et al. Society for Vascular Surgery practice guidelines for atherosclerotic occlusive disease of the lower extremities: Management of asymptomatic disease and claudication. J Vasc Surg. 2015;61(3 Suppl):2S-41S. PubMed CrossRef
[11] Gerhard-Herman MD, Gornik HL, Barrett C, et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: Executive summary. 2017;135(12):e686-725. PubMed PubMed Central NIHMSID: NIHMS867245. CrossRef
[12] Borreros CB, Delos Santos M. Peripheral arterial disease in general practice: Ankle-brachial index by palpation in the diagnosis of peripheral arterial disease. Phil Heart Center J. 2012;16(2):12-8. https://www.phc.gov.ph/about-phc/journals/pdf/may-aug2012/Peripheral%20Arterial%20Disease%20in%20General%20Practice.pdf.
[13] Migliacci R, Nasorri R, Ricciarini P, Gresele P. Ankle-brachial index measured by palpation for the diagnosis of peripheral arterial disease. Fam Pract. 2008:25(4):228-32. PubMed CrossRef
[14] Jones SR, Carley and Harrison M. An Introduction to power and sample size estimation. Emerg Med J. 2003; 20(5): 453-8. PubMed PubMed Central https://www.slideshare.net/drtamil/9-calculate-samplesize-for-diagnostic-study
[15] Lewis JEA, Williams P, Davies JH. Non-invasive assessment of peripheral arterial disease: Automated ankle brachial index measurement and pulse volume analysis compared to duplex scan. SAGE Open Med. 2016;4:2050312116659088. PubMed PubMed Central CrossRef
[16] Ouriel K, McDonnell AE, Metz CE, Zarins CK. Critical evaluation of stress testing in the diagnosis of peripheral vascular disease. Surgery 1982;91(6):686–93. PubMed
[17] Palmes PP, Obligacion MA. Ankle-brachial index by palpation method in the diagnosis of peripheral artery disease. Philipp J Cardiol. 2004; 32(2):45-50. http://www.herdin.ph/index.php/component/herdin/?view=research&cid=36719
Authors are required to accomplish, sign and submit scanned copies of the JAFES Author Form consisting of: (1) Authorship Certification, that all the requirements for authorship have been met by each author, and that the final version of the manuscript has been read and approved by all authors; (2) the Author Declaration, that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere; (3) the Statement of Copyright Transfer [accepted manuscripts become the permanent property of the JAFES and are licensed with an Attribution-Share Alike-Non-Commercial Creative Commons License. Articles may be shared and adapted for non-commercial purposes as long as they are properly cited]; and the ICMJE form for Disclosure of Potential Conflicts of Interest. For original articles, authors are required to submit a scanned copy of the Ethics Review Approval of their research as well as registration in trial registries as appropriate. For manuscripts reporting data from studies involving animals, authors are required to submit a scanned copy of the Institutional Animal Care and Use Committee approval. For Case Reports or Series, and Images in Endocrinology, consent forms, are required for the publication of information about patients; otherwise, appropriate ethical clearance has been obtained from the institutional review board. Articles and any other material published in the JAFES represent the work of the author(s) and should not be construed to reflect the opinions of the Editors or the Publisher.