Prevalence of Sexual Dysfunction and its Associated Factors among Women with Diabetes Mellitus Type 2 at Makati Medical Center Outpatient Department
James Paningbatan, Jimmy Aragon, Maria Princess Landicho-Kanapi, Katrina Rodriguez-Asuncion
James C. Paningbatan, MD
Section of Endocrinology, Diabetes and Metabolism
Department of Medicine, Makati Medical Center
No. 2 Amorsolo Street, Legaspi Village, Makati City, Philippines 1229
E-mail: paningbatanmd@yahoo.com
ORCID: https://orcid.org/0000-0001-9586-1521
e-ISSN 2308-118x
Printed in the Philippines
Copyright © 2018 by the JAFES
Received June 1, 2018. Accepted August 20, 2018.
Published Online First: September 11, 2018.
Objective. This study aims to determine the prevalence of sexual dysfunction among premenopausal Filipino women with type 2 diabetes mellitus at the outpatient department of a tertiary hospital through the use of the Female Sexual Function Index (FSFI) and identify factors that could be associated with sexual dysfunction.
Methodology. Seventy-five women with type 2 diabetes mellitus, aged 38 to 49 years old, received the FSFI questionnaire. Their age, history of hypertension, smoking habit, alcohol intake, body mass index, waist circumference, fasting blood sugar, HbA1c, creatinine, lipid profile, albuminuria or proteinuria, presence of microvascular complications such as diabetic retinopathy, neuropathy and nephropathy and their association with sexual dysfunction was determined.
Results. Seventy-two percent of the participants have sexual dysfunction scoring lowest in the lubrication, orgasm and pain domains. Age (p=0.016), a high body mass index (p=0.001), a fasting blood sugar above 100 mg/dl (p=0.006) and the presence of microvascular complications of diabetes mellitus namely, retinopathy (p=0.046) nephropathy (p=0.004) and neuropathy (p=0.001) were associated with sexual dysfunction.
Conclusion. The prevalence of sexual dysfunction is high among premenopausal Filipino women with type 2 diabetes mellitus, and is associated with age, a high body mass index, an uncontrolled fasting blood sugar and the presence of microvascular complications of diabetes mellitus.
Keywords: sexual dysfunction, type 2 diabetes mellitus, premenopause, diabetic neuropathies, diabetic retinopathy, diabetic nephropathiesThe American Psychiatric Association defines sexual dysfunction as a heterogeneous group of disorders that are typically characterized by a clinically significant disturbance in a person’s ability to respond sexually or to experience sexual pleasure.[1] Sexual problems are common complications of individuals with diabetes in both men and women. Unfortunately, sexual health is an often neglected aspect in the management of diabetes mellitus.[2],[3],[4]
Most studies on sexual dysfunction involves men and erectile dysfunction which affects 60 to 86.1% of men with diabetes mellitus.[5] In contrast, sexual dysfunction among women mostly includes problems in sexual desire, sexual satisfaction, orgasmic, lubrication and arousal disorder.[2]-[4] Documented rates of sexual dysfunction among women with type 2 diabetes ranges from 25% to 88%.[2],[4],[6],[7],[8],[9]
Though studies on sexual dysfunction are gradually increasing, there are currently no data that shows the prevalence of sexual dysfunction and the risk factors associated with it among Filipino women with diabetes mellitus.
Objectives of the study
The objectives of this study are to determine the prevalence and characterize the sexual dysfunction among premenopausal Filipino women with type 2 diabetes mellitus seen at the outpatient department of Makati Medical Center. This study also aims to determine whether age, history of hypertension, smoking habit, history of alcohol intake, body mass index, waist circumference, certain metabolic factors such as FBS, HbA1c, creatinine, lipid profile, albuminuria or proteinuria and whether the presence of microvascular complications of diabetes mellitus such as diabetic neuropathy, retinopathy and nephropathy are associated with sexual dysfunction among premenopausal Filipino women with type 2 diabetes mellitus.
METHODOLOGYStudy design
This cross-sectional analytic study was conducted at the outpatient department of Makati Medical Center from October 2017 to January 2018.
Subjects included female Filipinos with type 2 diabetes mellitus, 30 to 50 years old, premenopausal, with a current heterosexual partner and has had at least 1 sexual contact in the past 4 weeks. They must have been able to read, comprehend and understand either Filipino or English and must have consented to join the study.
The diagnosis of diabetes mellitus is based on the Unite for Diabetes Philippines Clinical Practice Guidelines: Fasting blood sugar of >126 mg/dl; plasma glucose of >200 mg/dl 2 hours after an oral glucose tolerance test; random blood sugar >200 mg/dl with classic symptoms of hyperglycemia or hyperglycemic crisis.[10]
Premenopause, according to the World Health Organization (WHO) and International Menopause Society, is defined as the period that encompasses the entire female reproductive period up to the final menstrual period or prior to menopause.[11]
Subjects with the following were excluded: Type 1 diabetes mellitus, prediabetes (impaired fasting glucose, impaired glucose tolerance), gestational diabetes, menopause, presence of sexual disorder before getting diabetes mellitus, existence of sexual disorder in patient’s spouse, known history of psychiatric illness, a history of mastectomy, total hysterectomy or current pregnancy.
Sampling method
This study utilized a purposive sampling method to achieve the minimum sample size. Purposive sampling is a non probability method wherein patients who consult at the outpatient department and fit the inclusion criteria were selected and enrolled once they have signed an informed consent.
Sample size and power calculation
With 53.6% prevalence of female sexual dysfunction,2 5% margin of error, 90% confidence interval, and 10% prediction of non-response or drop out, the computed sample size was 75 subjects.
Data gathering
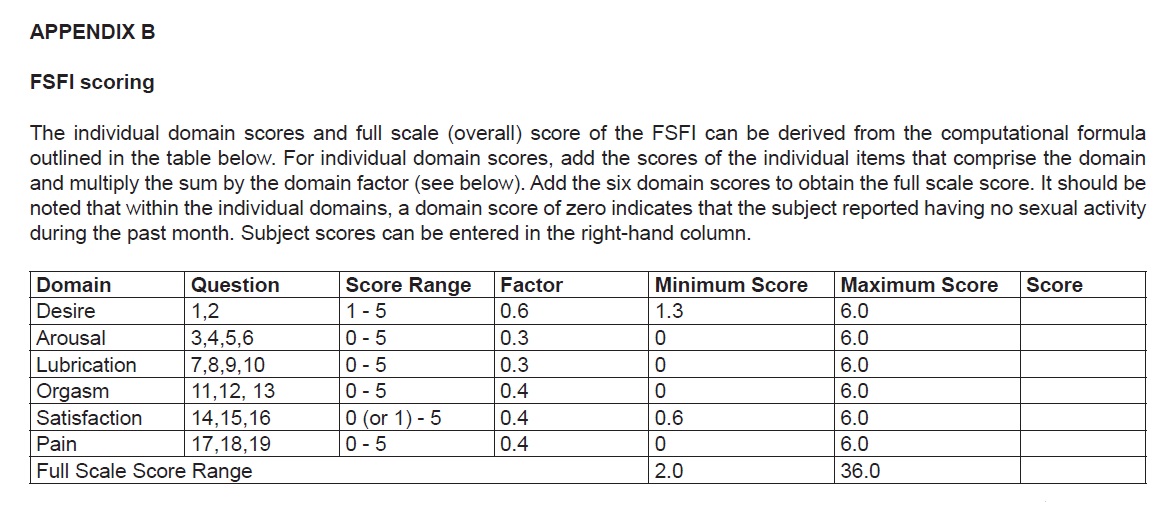
Data gathering commenced once the participant is able to meet the inclusion criteria and has signed an informed consent. The participant’s age, smoking habit, history of alcohol consumption were determined. The participant’s height, weight, waist circumference, blood pressure were measured using a standard measuring device. The Body Mass Index (BMI) was determined by dividing weight (kg) by the height in meter squared (m2). Based on the WHO criteria for BMI cut-off, participants were classified as either underweight (BMI<18.5), normal (BMI 18.5-24.9) overweight (25-29.9), or obese (BMI>30).
The participants’ most recent fasting blood sugar (FBS), HbA1c, lipid profile, creatinine, and urinalysis were retrieved from their records. Their estimated glomerular filtration rate (eGFR) was determined using the CKD-EPI formula with the use of Calculate by QxMD software.
Previous studies have shown that the presence of metabolic syndrome is associated with sexual dysfunction as compared with matched control without metabolic syndrome.[9],[12] Based on the National Cholesterol Education Program Adult Treatment Panel (NCEP ATP III 2005 revision) the presence of any three of the following criteria are considered for the diagnosis of metabolic syndrome for females; an FBS of greater than 100 mg/dl, triglyceride level of 150 mg/dl and above, high density lipoprotein (HDL) of less than 50 mg/dl, waist circumference greater than 35 inches, hypertension (systolic BP of above 130 mmHg or diastolic BP above 85 mmHg) or taking medications to control diabetes mellitus, dyslipidemia or hypertension.[13] Based on the 2018 American Diabetes Association Standards of Medical Care in diabetes, an HbA1c of above 7% is considered uncontrolled.[14]
Diabetic retinopathy was determined by reviewing patient’s chart for previous results of dilated fundoscopy. A dilated fundoscopy is the visualization of the patient’s retina done by an experienced ophthalmologist or optometrist which is standard of care and is recommended to be done at the time of diagnosis of type 2 diabetes mellitus.[14]
Diabetic neuropathy was assessed using the 10-g Semmes-Weinstein monofilament test which was performed by the primary investigator. Participants were examined lying down, with their eyes closed. Using a 10-g monofilament, four sites (1st, 3rd, and 5th metatarsal heads and plantar surface of distal hallux) were tested on each foot. Diabetic neuropathy is defined as the loss of the ability to detect the pressure at one or more site.[15]
Diabetic nephropathy was determined through the presence of albuminuria or proteinuria as determined by reviewing the participant’s record of urinalysis for proteinuria, a positive micral test, albumin to creatinine ratio of 30 and above, or a computed eGFR of less than 30 ml/min/1.73m2 based on the CKD-Epi formula.
Determination of sexual dysfunction
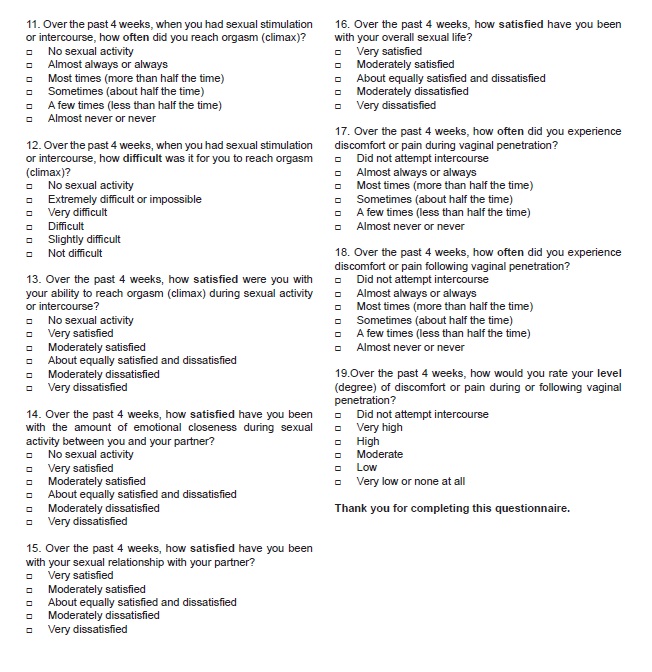
Sexual dysfunction was measured using the Female Sexual Function Index (FSFI) self-administered questionnaire (Appendix A). The FSFI is a brief, multidimensional self-report questionnaire measure of sexual functioning in women. It was developed for the specific purpose of assessing six domains of sexual functioning among females namely desire, arousal, lubrication, orgasm, satisfaction and pain during sexual intercourse.[2] The minimum and maximum scores are 2 and 36 respectively (Appendix B). Women with a score under 26.55 are classified as presenting with sexual dysfunction.[2]-[4],[16] A Filipino version of the Female Sexual Function Index was translated and validated by Rillon-Tabil et al.[17] Depending on the participant’s preference, either the English version or the Filipino version of the FSFI was used for this study (Figure 1). Participants were oriented that the questionnaire may contain delicate questions regarding sex. A pre-labeled FSFI questionnaire which corresponds to the participant’s identifier was handed to them and they were allowed to answer the questionnaire on their own and at their own pace.
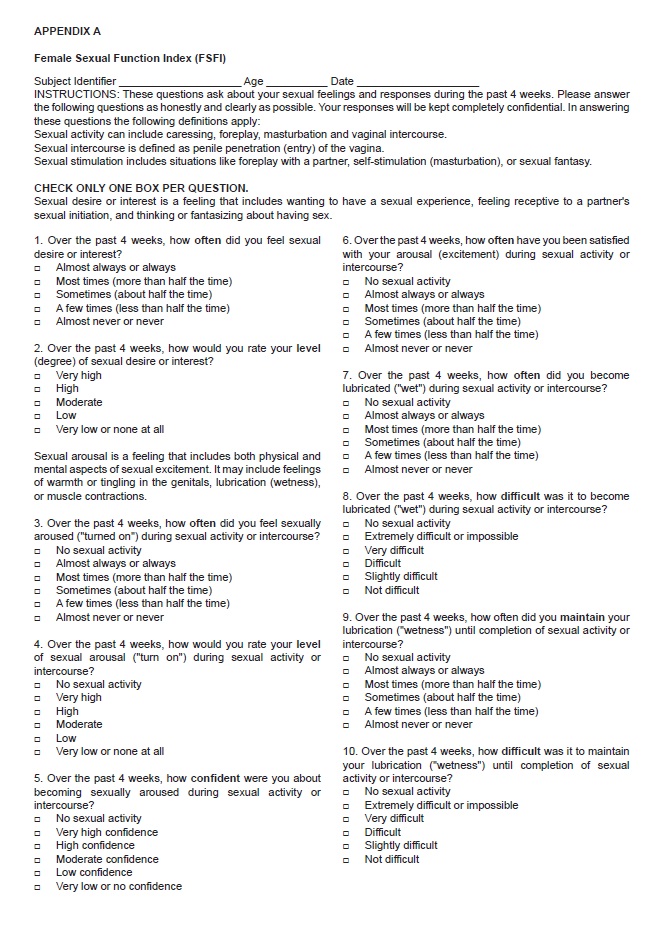
Appendix A. Female Sexual Function Index (FSFI)
Appendix B. FSFI Scoring
Figure 1. Flow chart.
Data processing and analysis
Descriptive statistics were used to summarize the demographics and clinical characteristics of the patients. Frequency and proportion were used for categorical variables and mean and standard deviation for interval/ratio variables. Unpaired sample T-test was used to determine the difference of means of those with sexual dysfunction against those without sexual dysfunction. Chi-square/ Fischer’s Exact Test, whichever is applicable, was used for categorical variable. Simple logistic regression was performed with the sexual dysfunction as the dependent variable and other variables as the independent variables to compute for the unadjusted odds ratio. Multiple logistic regression was also performed using all the independent variables that were used in simple logistic regression to obtain the adjusted odds ratio. Stepwise variable selection method was also used to determine the significant factors associated with sexual dysfunction. P-values that were less than 0.05 level of significance were considered significant. All valid data were included in the analysis performed using STATA 15.0.
Ethical considerations
The protocol was approved by the Institutional Review Board of the Makati Medical Center. Participants were enrolled in the study after obtaining a written informed consent. Data gathered from this study are entered in conformance with the principles of confidentiality. Participants are anonymized and assigned to consecutive case numbers. Age and control number were used as participant identifiers in case report forms to serve as reference to source documents. Participants were oriented that the questionnaire used in this study may contain delicate questions regarding sex. Participants were oriented that they can withdraw and their data can be excluded from the study anytime.
All of the 75 participants recruited for this study were able to complete the questionnaire and included in the final analysis. Two participants (2.7%) opted to use the Filipino version of the FSFI. Participants were aged 38 to 49 years old with a mean age of 45. Sixty percent of the participants are in the 45 to 50-year-old age group with a mean age of 47, while those that were below 45 years old had a mean age of 42. Seventy-six percent had a high BMI and 45% had a waist circumference above 35 inches. Eighty-eight percent had an elevated FBS and 60% had an uncontrolled HbA1c. Thirty-nine percent had an elevated triglyceride, 75% had a low HDL and 56% had an elevated low density lipoprotein (LDL). Forty-four percent were hypertensive, 20% were smokers and 24% were alcoholic beverage drinkers.
Seventy-two percent of the participants were found to have sexual dysfunction. Using Chi-square/Fischer's Exact Test, the variables that were associated with sexual dysfunction were age (p=0.016), a high body mass index (p=0.001) and FBS of more than 100 mg/dl (p=0.006) (Table 1).
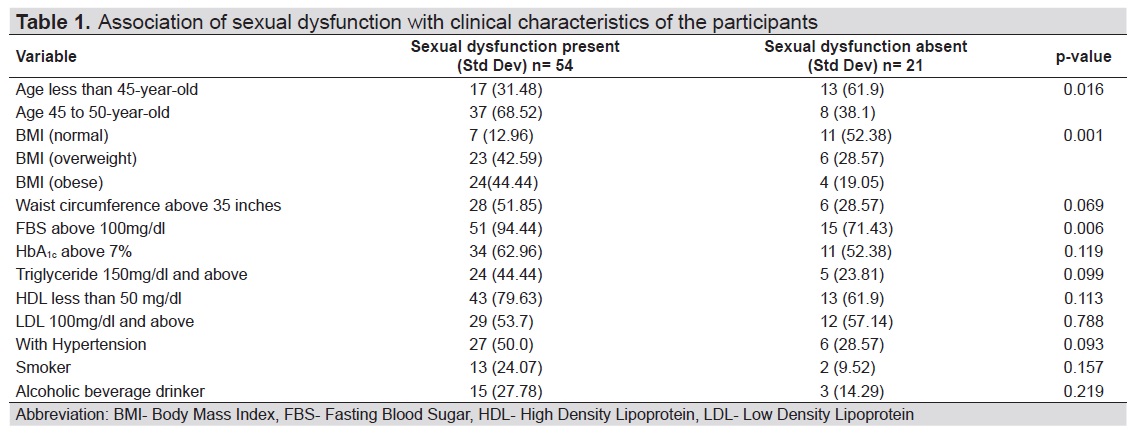
Table 1. Association of sexual dysfunction with clinical characteristics of the participants
Among those who were identified to have sexual dysfunction, the three domains that scored the lowest were lubrication, orgasm and pain (Table 2).
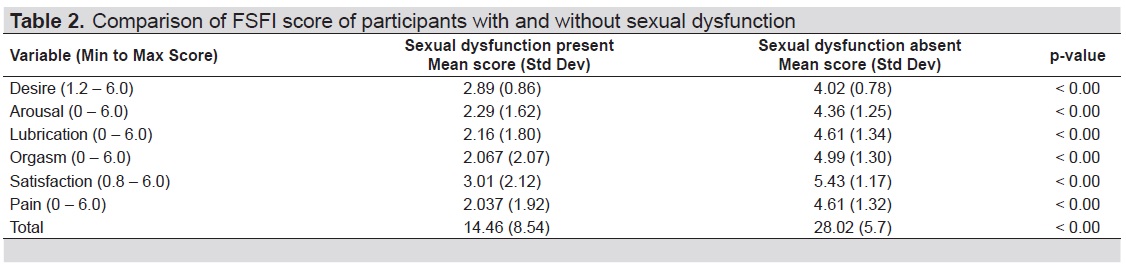
Table 2. Comparison of FSFI score of participants with and without sexual dysfunction
Using simple logistic regression to determine the individual effect of each variable and obtain the unadjusted odds ratio (OR), it was age (OR 3.53, 95% CI 1.23 – 10.12, p=0.019), an overweight BMI (OR 6.02, 95% CI 1.63 – 22.23, p=0.007), an obese BMI (OR 9.43, 95% CI 0.002 – 39.03, p=0.002), an elevated FBS (OR 6.8, 95% CI 1.51 – 30.49, p=0.012) and proteinuria (OR 12.73, 95% CI 1.51 – 30.49, p=0.017) that showed a possible association with sexual dysfunction (Table 3).
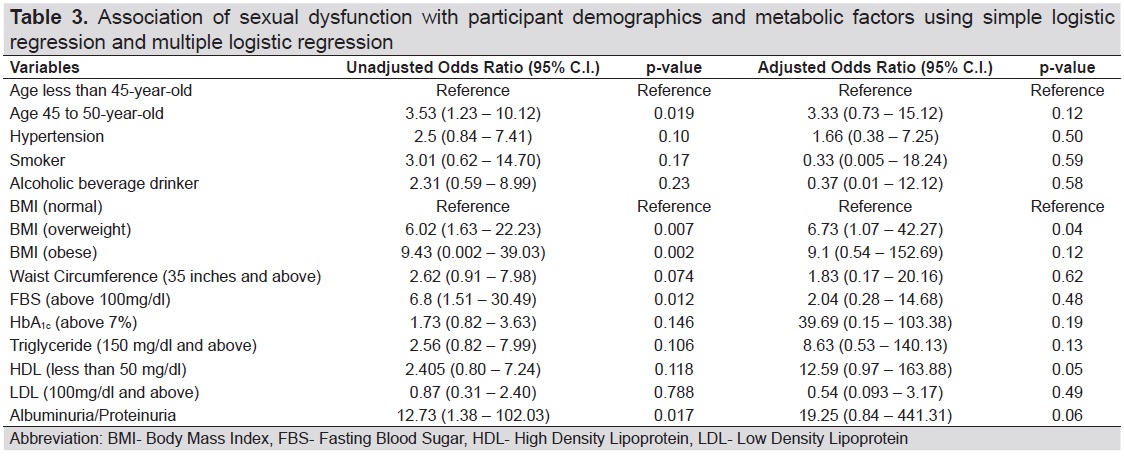
Table 3. Association of sexual dysfunction with participant demographics and metabolic factors using simple logistic regression and multiple regression
Using multiple logistic regression, which accounts for the effect due to all the additional variables and determines the adjusted OR, it was having an overweight BMI (OR 6.73, 95% CI 1.07 – 42.27, p=0.04) that showed a possible association with sexual dysfunction (Table 3).
Finally, using stepwise variable selection method to determine the significant factors associated with sexual dysfunction, it was a high BMI (OR 3.07, 95% CI 1.40 – 6.71, p=0.005), and albuminuria or proteinuria (OR11.65, 95% CI 1.38 – 98.13, p=0.024) that showed a possible association with sexual dysfunction (Table 4).
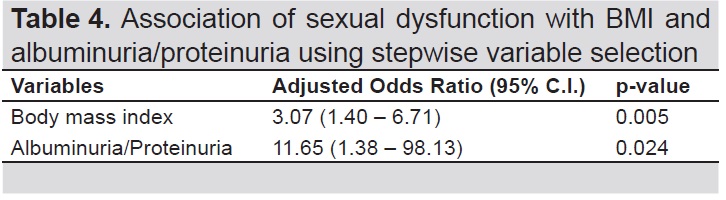
Table 4. Association of sexual dysfunction with BMI and albuminuria/proteinuria using stepwise variable selection
Using Chi-square/ Fischer’s Exact Test, the presence of microvascular complications of type 2 diabetes mellitus such as retinopathy (p=0.046) nephropathy (p=0.004) and neuropathy (p=0.001) was associated with sexual dysfunction (Table 5).
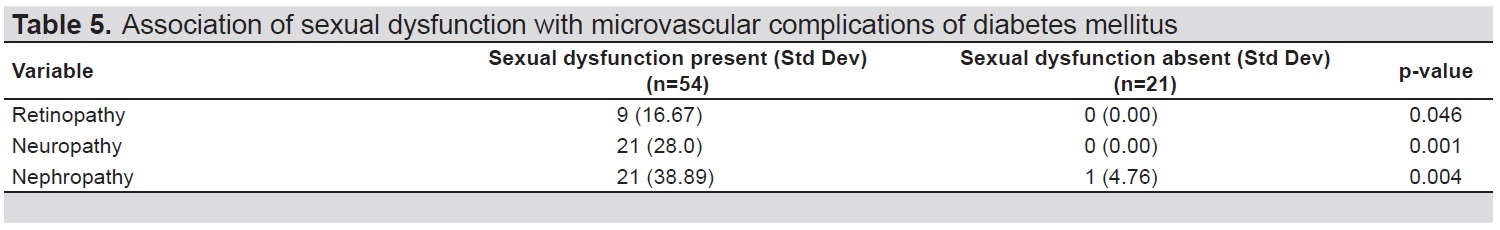
Table 5. Association of sexual dysfunction with microvascular complications of diabetes mellitus
Sexual dysfunction is a common problem worldwide.[18] In the Philippines where the prevailing attitude toward sex is mostly conservative, sexual dysfunction is not routinely discussed between patient and physician and is often neglected. A study done by Lewis in 2012 showed that more Filipino women have difficulties in lubrication (50%) and achieving orgasm (56%) as compared with women from other Asian countries.[19]
Studies have shown that sexual dysfunction is more frequent in women with diabetes mellitus compared with control.[9] However, data on sexual dysfunction among women with diabetes mellitus are conflicting. A major problem with published clinical studies assessing the effect of diabetes mellitus on sexuality in women is the inconsistency between study designs, making it difficult to directly compare across studies and draw firm conclusions.[9],[20] Unlike research done on male sexual dysfunction, the lack of a measurable physical parameter to measure sexual dysfunction among females is a common, inevitable limitation of studies done on female sexual health, making interviews and questionnaires of different versions the only available approaches to this issue.[21] In recent studies, the FSFI questionnaire has been widely used to establish the presence of sexual dysfunction.[9]
The meta-analysis by Pontiroli et al., showed that the risk for sexual dysfunction is higher among women with type 2 diabetes mellitus as compared with women with type 1 diabetes mellitus.[9] Celik et al., stated that the high frequency of sexual dysfunction and the lower sexual quality of life in women with type 2 diabetes mellitus are considered to be resulting from the fact that most women with type 2 diabetes were in the older age group and most of them were in menopause. Moreover, the development and diagnosis of type 2 diabetes mellitus, in contrast to type 1 diabetes mellitus, occurs later in life when relationships and sexual expectations are already established. This new diagnosis may require adaptive changes in behavior and relationship patterns, potentially creating marital tension and intimacy conflict, which ultimately leads to or exacerbates sexual problems.[20]
Studies also showed that the risk of having sexual dysfunction among premenopausal women with either type 1 or type 2 diabetes mellitus were significant as compared with women with diabetes mellitus in their menopause.[20],[21] The relatively less significant difference in the menopause groups might be the result of the overwhelming senescence and the natural worsening of sexual functions in both diabetic and control groups with aging.[21]
In this study, we decided to include only women with type 2 diabetes mellitus who are in their reproductive years. Seventy two percent of the participants were found to have sexual dysfunction as compared with documented rates of sexual dysfunction among women with diabetes mellitus that ranged from 25% to 88%.[2],[4],[6]-[9] By using Chi-square/ Fischer’s Exact Test, it was shown that age was significantly associated with sexual dysfunction (p=0.016). Using simple logistic regression, the 45 to 50-year-old age group showed a possible association with sexual dysfunction (p=0.019), however this was no longer shown in the subsequent multiple logistic regression and stepwise variable selection analysis. The computed odds ratio in the simple logistic regression (OR 3.53, 95% CI 1.23 – 10.12) suggests that the odds of having sexual dysfunction among Filipino, female type 2 diabetics in the 45-50 age group is 3.5 times higher as compared with those aged less than 45 years old.
Among the participants who were identified to have sexual dysfunction, the three domains that scored the lowest were lubrication, orgasm and pain. In comparison with the study done in China in 2012, where premenopausal participants with type 2 diabetes mellitus scored lowest in the satisfaction, arousal and desire domain, these results are consistent with the study by Lewis, that showed more Filipino women have difficulties in lubrication and achieving orgasm as compared with women from other Asian countries.[19],[21]
Previous studies showed sexual dysfunction is associated with a high BMI and the metabolic syndrome, while other independent variables consistent with the clinical and metabolic correlates reported in several studies showed no statistically significant correlation with sexual dysfunction.9,12,18,22 In this study, by using Chi-square/ Fischer’s Exact Test, it was shown that BMI was significantly associated with sexual dysfunction (p=0.001). By using simple logistic regression to determine the individual effect of each variables, having an overweight (p=0.007), and an obese BMI (p=0.002) showed a possible association with sexual dysfunction. When accounting for the effects due to all the additional variables through multiple logistic regression, it was only having an overweight BMI (p=0.04) that showed a possible association with sexual dysfunction. On further analysis using the stepwise variable selection, a high BMI (p=0.005) showed a possible association with sexual dysfunction. The calculated adjusted odds ratio in the stepwise variable selection (OR 3.07, 95% CI 1.40 – 6.71) suggests that among premenopausal Filipino females with type 2 diabetes mellitus and a high BMI, the odds of having sexual dysfunction is three times higher as compared to those with a normal BMI.
Of the five criteria that defines the metabolic syndrome, only an elevated FBS of more than 100mg/dl was noted to be significantly associated with sexual dysfunction based on Chi-square/ Fischer’s Exact Test (p=0.006) and is also suggested in the simple logistic regression (p=0.012). The computed odds ratio in the simple logistics regression (OR 6.8, 95% CI 1.51 – 30.49) suggests that the odds of sexual dysfunction among Filipino, female type 2 diabetics with an elevated FBS of more than 100 mg/dl is 6.8 times higher as compared to those without an elevated FBS. One must be cautious in interpreting this data since FBS measurement can be varied depending on multiple factors and does not reflect a long term picture of a patient’s diabetes status. Moreover, the wide confidence interval suggests that the sample size in this study is small and that conclusions should be replicated with a study that involves a larger sample size.
Diabetic end-organ complications may play a role in female sexual dysfunction, however the relationship of complications and sexual dysfunction was indicated only by few articles and was excluded by most studies.[9],[21] In our study, based on Chi-square/ Fischer’s Exact Test, all of the three microvascular complications of diabetes mellitus namely diabetic retinopathy, nephropathy and neuropathy were associated with sexual dysfunction or a low FSFI score. The microvascular complications of diabetes mellitus were no longer included in the logistic regression analysis due to null participants with no sexual dysfunction in the diabetic retinopathy and diabetic neuropathy subgroup (Table 5).
Similar to the cross sectional study done by Vafaeimanesh et al.,[2] our study also showed that there is significant correlation between diabetic retinopathy and the presence of sexual dysfunction (p=0.046).
Previous studies reported diabetic neuropathy and sexual dysfunction in different ways.[9] Among women with diabetes mellitus, psychological morbidity may be a possible determinant.[8] A study by Elyasi stated that depression is common in women with Type 2 DM and sexual dysfunction is highly prevalent among those with depression.[23] Among men, peripheral neuropathy is a common cause of erectile dysfunction, however, there is little relevant literature among women to associate peripheral neuropathy with sexual dysfunction.[24] In this study the presence of diabetic neuropathy as documented by the inability to identify at least one out of 4 test points in the 10-g Semmes-Weinstein monofilament test was significantly associated with the presence of sexual dysfunction (p=0.001).
The presence of albuminuria or proteinuria showed possible association with sexual dysfunction in the simple logistic regression (p=0.017) and stepwise variable selection (p=0.024). Although the computed adjusted odds ratio in the stepwise variable selection (OR 11.65, 95% CI 1.38 – 98.13) suggests that the odds of having sexual dysfunction is twelve times higher in the presence of albuminuria or proteinuria, the wide confidence interval suggests that the sample size in this study is small and that conclusions should be replicated with a study that involves a larger sample size.
In our institution, it was identified that the prevalence of sexual dysfunction is high among premenopausal Filipino females with type 2 diabetes mellitus. It is therefore recommended to screen for sexual dysfunction among this group. Clinicians can opt to use the FSFI as an objective tool to assess for the presence of sexual dysfunction and identify specific domains that could be of particular concern for the patient. Since among women, sexual dysfunction mostly includes problems in sexual desire, satisfaction, orgasmic, lubrication and arousal[2]-[4] the management of sexual dysfunction may require a multidisciplinary approach for optimal management, and referral to an OB-Gynecologist or a psychiatrist should be considered whenever necessary. In this study, women scored lowest on lubrication, orgasm and pain domains and based on these findings, clinicians can advise patients on methods to achieve adequate lubrication such as proper hydration, proper stimulation, or the use of artificial lubricants in order to lessen pain and hopefully achieve improvement in orgasm. Other possible causes of pain such as infection, vaginismus, or genital skin conditions should also be identified and addressed properly. Patients should also be advised to maintain or achieve a normal BMI which has been an identified risk factor associated with sexual dysfunction.[9],[12],[18],[22] This study was able to identify that the microvascular complications of diabetes mellitus may be associated with sexual dysfunction. Diabetes is a complex, chronic illness requiring continuous medical care with multifactorial risk-reduction strategies beyond glycemic control. Ongoing patient self-management education and support are critical to preventing acute complications and reducing the risk of long-term complications.[14]
Limitations of the study and recommendations
As in many studies about sexual dysfunction, a small population size is a limitation in the interpretation of data. In this study, some variables have very wide confidence interval (e.g. confidence interval for FBS and albuminuria). This is due to a bias called sparse data bias low event per variable, categorical covariates with very low or high prevalence, and narrowly distributed continuous predictors. Moreover, due to the small sample size, the regression analyses done in our study is not valid and at best provides only an estimate and should be validated in future studies with a larger sample size.
It is therefore recommended that a prospective study that involves a larger number of participants that may involve multiple centers be done as follow-up. It is also suggested that studies be done on whether an improvement in body mass index or treatment of diabetic retinopathy, neuropathy or nephropathy would result in an improvement of FSFI score or overall sexual health.
Seventy-two percent of premenopausal Filipino women with type 2 diabetes mellitus seen at the outpatient of Makati Medical Center were found to have sexual dysfunction. Among the participants who were identified to have sexual dysfunction, the three domains that scored the lowest were lubrication, orgasm and pain. Age, a high body mass index, an uncontrolled fasting blood sugar and presence of diabetic retinopathy, neuropathy or nephropathy is associated with sexual dysfunction.
Statement of AuthorshipAll authors certified fulfillment of ICMJE authorship criteria.
Author DisclosureThe authors declared no conflict of interest.
Funding SourceNone.
[1] American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 5th ed. USA: Washington, DC, 2013. CrossRef
[2] Vafaeimanesh J, Raei M, Hosseizaddeh F, Farham M. Evaluation of sexual dysfunction in women with type 2 diabetes. Indian J Endocrinol Metab. 2014;18(2):175-9. PubMed PubMed Central CrossRef
[3] Rosen RC, Brown C, Heiman J, et al. The Female Sexual Function Index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26(2):191-208. PubMed CrossRef
[4] Fatemi SS, Taghavi SM. Evaluation of sexual function in women with type 2 diabetes mellitus. Diab Vasc Dis Res. 2009;6(1):38-9. PubMed CrossRef
[5] Binmoammar TA, Hassounah D, Alsaad S, Rawaf S, Majeed A. The impact of poor glycemic control on the prevalence of erectile dysfunction in men with type 2 diabetes mellitus: A systemic review. JRSM Open. 2016;7(3):2054270415622602. PubMed PubMed Central CrossRef
[6] Cortelazzi D, Marconi A, Guazzi M. Sexual dysfunction in pre-menopausal diabetic women: Clinical, metabolic, psychological, cardiovascular, and neurophysiologic correlates. Acta Diabetol. 2013;50(6):911-7. PubMed CrossRef
[7] Bargiota A, Dimitropoulos K, Tzortzis V, Koukoulis GN. Sexual dysfunction in diabetic women. Hormones (Athens). 2011;10(3):196-206. PubMed
[8] Ogbera AO, Chinenye S, Akinlade A, Eregie A, Awobusuyi J. Frequency and correlates of sexual dysfunction in women with diabetes mellitus. J Sex Med. 2009;6(12):3401-6. PubMed CrossRef
[9] Pontiroli AE, Cortellazi D, Morabito A, Female sexual dysfunction and Diabetes: A systemic review and meta-analysis. J Sex Med. 2013;10(4):1044-51. PubMed CrossRef
[10] Unite for Diabetes Philippines 2011: Philippine practice guidelines for the diagnosis and management of diabetes. https://www.diabetesphil.org/html/files/clinical_practice_guidelines_draft.pdf
[11] Menopause terminology. http://www.imsociety.org/menopause_terminology.php. Accessed July 25, 2018.
[12] Esposito K, Ciotola M, Marfella R, Di Tommaso D, Cobellis L, Giugliano D. Sexual dysfunction in women with metabolic syndrome. Diabetes Care. 2005;28(3):756. PubMed
[13] Huang PL. A comprehensive definition for metabolic syndrome. Dis Model Mech. 2009;2(5-6): 231-7. PubMed PubMed Central CrossRef
[14] American Diabetes Association. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes - 2018. Diabetes Care. 2018;41(Suppl 1):S12-27. PubMed CrossRef
[15] Boulton A, Armstrong D, Albert S, et al. Comprehensive foot examination and risk assessment: A report of the task force of the foot care interest group of the American Diabetes Association, with endorsement by the American Association of Clinical Endocrinologists. Phys Ther. 2008;88(11):1436-43. PubMed
[16] Wiegel M, Meston C, Rosen R. The female sexual function Index (FSFI) cross-validation and development of clinical cut-off scores. J Sex Marital Ther. 2005;31(1):1-20. PubMed CrossRef
[17] Rillon-Tabil N, Malong CLP, Vicere JJB, Gomez MHS. Translation and validity of the Female Sexual Function Index Filipino Version (FSFI-Fil). Philipp J Intern Med. 2013; 51(4):1-11.
[18] Esposito K, Maiorino MI, Bellastella G, Giugliano F, Romano M, Giugliano D. Determinants of female sexual dysfunction in type 2 diabetes. Int J Impot Res. 2010;22(3):179-84. PubMed CrossRef
[19] Lewis RW. Epidemiology of sexual dysfunction in Asia compared to the rest of the world. Asian J Androl. 2011;13(1):152-8. PubMed PubMed Central CrossRef
[20] Celik S, Golbasi Z, Kelleci M, Satman I. Sexual dysfunction and sexual quality of life in women with diabetes: The study based on a diabetic center. Sex Disabil. 2015;33(2):233-41. CrossRef
[21] Shi YF, Shao XY, Lou QQ, Chen YJ, Zhou HJ, Zou JY. Study on female sexual dysfunction in type 2 diabetic Chinese women. Biomed Environ Sci. 2012;25(5):557-61. PubMed CrossRef
[22] Doruk H, Akbay E, Cayan S, Akbay E, Bozlu M, Acar D. Effect of diabetes mellitus on female sexual function and risk factors. Arch Androl. 2005;51(1):1-6. PubMed CrossRef
[23] Elyasi F, Kashi Z, Tasfieh B, Bahar A, Khademloo M. Sexual dysfunction in women with type 2 diabetes mellitus. Iran J Med Sci. 2015;40(3):206-13. PubMed PubMed Central
[24] Azadzoi KM, Siroky MB. Neurologic factors in female sexual function and dysfunction. Korean J Urol. 2010;51(7):443-9. PubMed PubMed Central CrossRef
Authors are required to accomplish, sign and submit scanned copies of the JAFES Author Form consisting of: (1) Authorship Certification, that all the requirements for authorship have been met by each author, and that the final version of the manuscript has been read and approved by all authors; (2) the Author Declaration, that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere; (3) the Statement of Copyright Transfer [accepted manuscripts become the permanent property of the JAFES and are licensed with an Attribution-Share Alike-Non-Commercial Creative Commons License. Articles may be shared and adapted for non-commercial purposes as long as they are properly cited]; and the ICMJE form for Disclosure of Potential Conflicts of Interest. For original articles, authors are required to submit a scanned copy of the Ethics Review Approval of their research as well as registration in trial registries as appropriate. For manuscripts reporting data from studies involving animals, authors are required to submit a scanned copy of the Institutional Animal Care and Use Committee approval. For Case Reports or Series, and Images in Endocrinology, consent forms, are required for the publication of information about patients; otherwise, appropriate ethical clearance has been obtained from the institutional review board. Articles and any other material published in the JAFES represent the work of the author(s) and should not be construed to reflect the opinions of the Editors or the Publisher.