Alistair Kashmir C. Dela Cruz, MD
Section of Endocrinology, Diabetes and Metabolism, Chong Hua Hospital
Tel. No.: +63 (32)-255-8000
Fax No.: +63 (32)-255-5639
E-mail: alistairdelacrzmd@yahoo.com
ORCiD: https://orcid.org/0000-0002-3951-1663
e-ISSN 2308-118x
Printed in the Philippines
Copyright © 2019 by the JAFES
Received April 6, 2019. Accepted July 18, 2019.
Published Online First: November 10, 2019.
Objective. To determine the beliefs and attitudes towards diabetes of rural health care providers in Aklan, Philippines using the Diabetes Attitude Scale 3 (DAS-3) and to determine factors associated with it.
Methodology. This is a cross-sectional analytic survey. A total of 339 health care providers were given self-administered DAS-3 questionnaires. Additional data gathered included their age, highest educational attainment, position, municipality class, diabetes as a co-morbidity, attendance to diabetes classes, and family history of diabetes.
Results. Rural health care providers showed an overall mean positive attitude score of 3.5 using the DAS-3 questionnaire. In decreasing order, mean scores of participants according to subscale is as follows: “Need for Special Training in Education” (4.13) >“Autonomy of diabetes for patients” (3.70) >“Psychosocial Impact of Diabetes” (3.60) >“Value of Tight Glucose Control” (3.14) and “Seriousness of Type 2 Diabetes” (3.09). Physicians have the highest mean scores consistently in all subscales compared to other health care providers. Among the different factors considered, educational attainment (p=0.005) and work position (p=<0.001) were found out to affect attitude score of health care providers.
Conclusion. This study has shown that the majority of the rural health care providers believe in the need for special training of healthcare providers, psychosocial impact of diabetes and patient autonomy in diabetes self-care. However, the majority still do not strongly believe in the seriousness of diabetes and the benefits of tight sugar control. Educational attainment and work position are the consistent factors that impact diabetes-related attitude; therefore, the need to strengthen continuous medical education among health care providers.
Keywords: DAS-3, type 2 diabetes, attitude, Rural Health CenterDiabetes and its complications impose a heavy burden to the individual, to the individual’s family and to the society in general. In the Philippines, it is estimated that there are 3.2 million cases of Type 2 Diabetes Mellitus with a 5.9% prevalence rate among adults between the ages of 20 and 79 years, of which only 20% have good glycemic control (Hba1c <7%).[1],[2] The high burden of diabetes and its complications in the country is somehow an indirect reflection of its health care delivery system.
The Philippine health care delivery system is a threetier system, similar to other countries, composed of both private and public facilities. Data from the 2008 National Demographic and Health Survey (NDHS) showed that about 50% percent of Filipino patients availed health services from public health facilities, 42% from private facilities and 7% from alternative or traditional medicine.[3] Rural Health Units (RHUs) and Barangay Health Centers, which represent the most basic unit, is the most visited public health care delivery facility across the country. This constitutes 33% of all visits mainly because of affordability and easy access.[3]
With the advent of healthcare decentralization from the national government to the local government unit, Rural Health Units (RHU) and Barangay Health Centers became the primary unit for the delivery of basic health services for patients belonging under the municipal and barangay level (local neighborhood).[4] These local facilities are managed by the municipal health officer (local physician) and supported by rural health nurses, midwives, and barangay health workers (BHWs). In relation to diabetes care, healthcare providers from both RHU and BHS are responsible for the basic screening and provision of lifestyle change, diabetes self-managed education (DSME) and provision of low-cost medications to the local community especially the indigent patients.[3],[5]
To ensure the proper delivery of these basic services to the grass root levels, it is imperative that these front liners of basic health units have the proper attitude and beliefs towards diabetes, since an individual’s attitude influences on how an individual responds to health promotion information and how an individual would educate his/ her patients. It has been reported that poor diabetic care of patients is due to the prevalent and misguided attitudes of both healthcare professionals and patients with diabetes.[6] Barangay Health Workers (BHWs) in particular, being the first line in the barangay level (local neighborhood) and constitute the largest number among rural health care professionals, are particularly vulnerable to having misguided attitudes toward diabetes due to inadequate diabetes education and training. There are currently no published data about that impact of diabetes-related attitudes on rural healthcare professionals, especially the BHWs. Therefore, it is essential to determine the diabetesrelated attitudes of healthcare professionals since the improvement of attitude toward diabetes also improves adherence to diabetes care.
The third version of Diabetes Attitude Scale (DAS-3) by Anderson et al. of the University of Michigan is one of the several questionnaires that was developed to measure general diabetes-related attitudes of both people with diabetes and health care professionals.[7]
This validated tool has already been used and adapted in different languages and has shown to be valid and reliable. Studies done on diabetes-related attitudes of healthcare professionals have different attitude patterns across different parts of the world, showing the influence of diverse cultural settings. In the Philippines, Yao et al., in 2004 have developed a validated Filipino version DAS-3 which was used to survey persons with diabetes in the outpatient department of the UP-Philippine General Hospital.[8] This questionnaire was likewise utilized by Ardeña et al., to evaluate the knowledge, attitudes and practices of a person with Type 2 diabetes in a rural community in the Philippines.[9] However, no study yet was conducted evaluating the diabetes-related attitude of healthcare professionals in the local setting, hence the purpose of this study.
Using the Filipino version of Diabetes Attitude Scale (DAS-3) questionnaire, it is the aim of this study to determine the beliefs and attitudes of rural healthcare professionals in Aklan, Philippines towards diabetes and its treatment which include the following aspects: 1) need for special training in education, 2) seriousness of type 2 diabetes, 3) value of tight glucose control, 4) psychosocial impact and 5) patient autonomy. Moreover, this study aims to determine the association of DAS-3 scores with factors such as age, highest educational attainment, health care provider’s position, municipality class, diabetes as a co-morbidity, attendance to diabetes classes and family history of diabetes.
The data that would be gathered from this study would be helpful for national policymakers to identify areas in which improvement can be implemented through policies and programs that would provide additional educational and technical support for rural HCPs to provide better diabetes care.
Study design/methodology
This is a cross-sectional analytical, multicenter survey among health care providers of rural health units in Aklan, Philippines.
Study population
This study included health care providers from different rural health centers from all municipalities of the province of Aklan, Philippines. This included the physicians, nurses, midwives, and the barangay health workers (BHW). They were provided with consent form prior to participating in the study.
Sample population size of healthcare providers from each municipality was determined using stratified random sampling, in which representatives of each healthcare provider position were included in the study. The number of subjects was computed based on a master list of employees obtained from each municipal health office of all 17 municipalities from the province of Aklan, Philippines. Computation of sample population size for each group of health care workers was set with the level confidence of 95%, response to distribution of 50% and a margin error of 5% based on previous DAS-3 survey. Because the population size of physicians, rural health nurses and midwives per municipality are small, almost all were included in the sample population (See Appendix 1). The target sample population number of barangay health workers were evenly distributed to every 17 municipalities.
Inclusion criteria
Participants who can read, write and comprehend either Filipino, Akeanon (local dialect) and English language.
Exclusion criteria
a) Health care providers who have difficulty reading and understanding questionnaires due to language barrier
b) Healthcare providers who will not consent to answer the questionnaires
Instrument
The diabetes attitude scale was adapted from the Third Version (DAS-3) developed by Anderson et al. and a Filipino version by Yao et al. The Filipino version was validated and translated by the University of the Philippines Manila Sentro ng Wikang Filipino which was used in the study of Yao et al in their study at University of the Philippines - Philippine General Hospital. The authors gave formal consent regarding the use of Filipino version of DAS-3 questionnaire in this study. The local version was translated to Akeanon dialect and underwent peer-review by the West Visayas State University Sentro ng Wikang Filipino (Center of Filipino Language).
The questionnaire contains 33 questions, composed of five subscales, namely:
1. The need for special training in education (Number of Items: 5)
– Assesses the respondent’s attitude about the need for health care providers who care for patients with diabetes to have special training in teaching, counseling and behavior change techniques.
2. Seriousness of Type 2 Diabetes (Number of Items: 7)
– Assesses the respondent’s attitude about the seriousness of Type 2 Diabetes
3. The overall value of tight glucose control in diabetes care (Number of items: 7)
– Assesses the respondent’s attitude about whether the potential benefit of tight glucose control is justified in terms of the cost to the patient
4. Psychosocial impact of diabetes on patients (Number of items: 6)
– Assesses the respondent’s attitude toward the psychosocial impact of diabetes on the lives of the people with the disease
5. Attitude toward patient autonomy (Number of items: 8)
– Assesses the respondent's attitude about whether patients should be the primary decision-makers regarding the daily self-care of their diabetes
Additional data that were gathered included the age of the participant, gender, healthcare provider position/role, educational attainment, history of diabetes, attendance in diabetes classes, presence of relatives with diabetes and the municipality class to which the participant’s rural health center belong. For the classification of municipality class, this is based on the municipality’s annual average income set by the Philippine Government’s Department of Finance.[10]
The survey proper was conducted under the supervision of the researchers. Clarifications regarding the questions/ items were allowed under the proper supervision of the researchers.
Survey proper
The study protocol and informed consent forms were submitted to and approved by the Institutional Research Ethics Review Board (IRB). Letter of intention to conduct the study was also sent to each of the department heads of rural health centers involved in the study.
Each subject was given a printed explanation of the study including its purpose, type of information sought and the confidentiality of their response. Participants were given the choice of which version of the DAS-3 questionnaire they will answer in accordance to which language they are more adept with. This is to minimize errors in comprehending questions due to language barrier. They were then requested to complete the selfadministered DAS 3 questionnaire. Patients at the onset of the survey are requested to indicate if he/she has difficulty of understanding majority of the questions as to exclude them from the study. No further revisions were made on the translated Filipino version of the questionnaire.
Survey proper and data collection was done from May 2018 to July 2018 in all municipal
One-way Analysis of Variance (ANOVA) and a Tukey HSD post hoc test was used for data analysis to compare score among the healthcare professionals. A univariate and multivariate regression analysis was also used to determine the relationship of attitude scores (both in nominal and ordinal form) and socio-demographic characteristics such as municipality class to which the participant’s rural health center belong, age of the participant, gender, healthcare provider position/role, educational attainment, diabetes as co-morbid, attendance in diabetes classes and presence of family history with diabetes. The statistical software package Microtab statistical software and Raosoft sample size calculator was used for this analysis.
Out of 487 participants that were invited in this study, only 339 participants were able to participate with an overall response rate of 69.60%. There were 19 doctors, 27 nurses, 122 midwives, and 171 barangay health workers who participated with response rates of 95%, 84.38%, 129.79%, and 50.15% respectively.
The majority of participants are females (N=287, 84.6%) and have a mean age of 49.66±11.33 years with most respondents coming from the 50-59 years old bracket (N=144, 52.8%).
Majority of the responders are barangay health workers comprising 50.44% of the total population (N=177). Most of the subjects were college graduates (N=186, 54.6%). More than half (N=194, 57.23%) have in any way attended some form of DM class. A third of the respondents have diabetes themselves (N=107,31.56%), and more than half of the respondents have 1 or more relatives who have diabetes (N=192,56.64%) (Table 1).
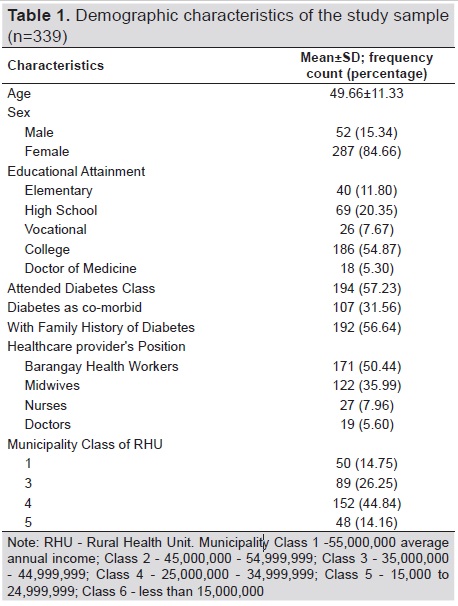
Table 1. Demographic characteristics of the study sample (n=339)
The overall Diabetes Awareness Score among all the participants shows a mean positive score of 3.5, or a positive score, according to the DAS-3 questionnaire scoring system. (Table 2) Among the given subscales, “The Need for Special Training in Education” garnered a positive response with a score 4.13 of the total population, while “Seriousness of Type 2 Diabetes” garnered the lowest score of 3.09, which is a neutral response. In decreasing order, the overall response score is as follows: “Need for Special Training in Education”>“Autonomy of diabetes for patients”>“Psychosocial Impact of Diabetes”>“Value of Tight Glucose Control and lastly seriousness of Type 2 Diabetes.”
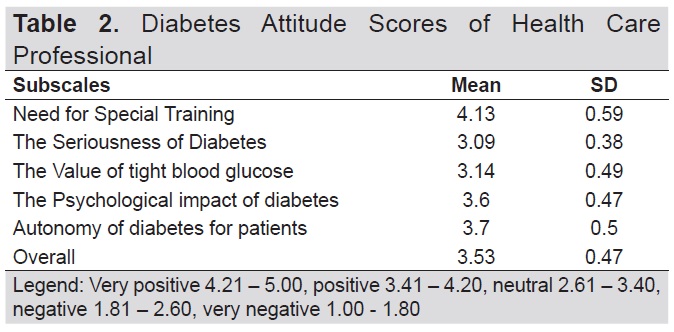
Table 2. Diabetes Attitude Scores of Health Care Professional
Using one-way analysis of variance (ANOVA), the mean scores for each subscale were compared among the healthcare professionals. In the subscale of 'need for special training,’ rural health physicians have greater mean scores statistically compared to nurses, midwives, and barangay health workers, who have comparable mean scores. This is also true in the other subscales such as 'seriousness of diabetes' and 'psychosocial impact of diabetes.'
In the subscale of 'value of tight glucose control,' both medical doctors and rural health nurses have no significant difference in their attitude scores but are significantly higher compared to midwives and barangay health workers (BHWs).
For the subscale of 'autonomy of diabetes for patients’ showed that the mean scores of the doctors, nurses and barangay health workers are comparable and are statistically higher than that of the midwives (Table 3).
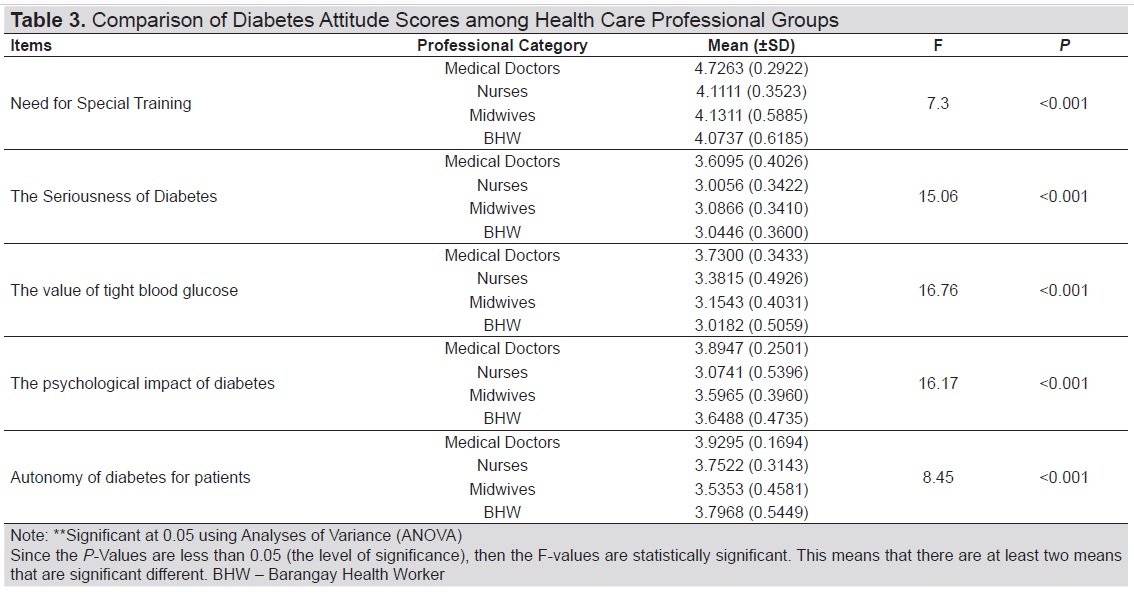
Table 3. Comparison of Diabetes Attitude Scores among Health Care Professional Groups
A univariate and multivariate regression analysis done showed that highest educational attainment and position of health care providers are statistically significant (p 0.005, <0.001). The coefficients suggest that education and position are positively related to diabetes attitude scores. These imply that professionals with higher educational attainment and those with higher work position tend to have high scores. However, in the multivariate regression analysis, only position was statistically significant. The coefficient suggests that position is positively associated with diabetes attitude scores (Table 4).
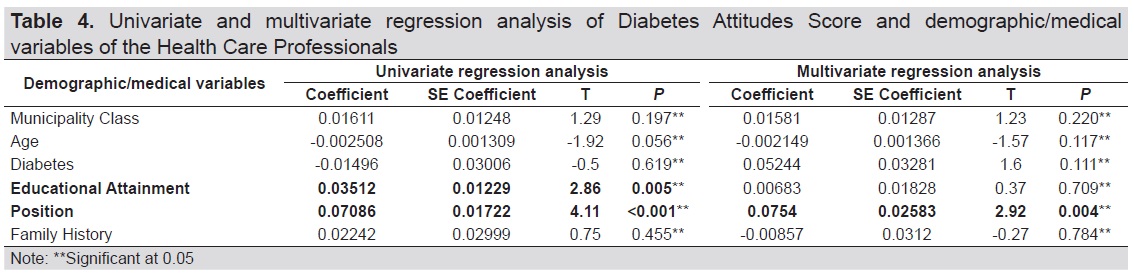
Table 4. Univariate and multivariate regression analysis of Diabetes Attitudes Score and demographic/medical variables of the Health Care Professionals
A univariate and multivariate ordinal regression analysis was also done for attitude scores that were classified as very positive, positive, neutral, very negative, and negative according to the DAS-3 questionnaire scoring system. Results showed that third class municipality, age, medical doctor degree, and municipal health officer position are statistically significant. The coefficients and odds ratios indicate that medical doctor degree, medical health officer position and health care professionals who belong from third class municipalities are more likely to respond "very positive" than other factors that were examined (Table 5).
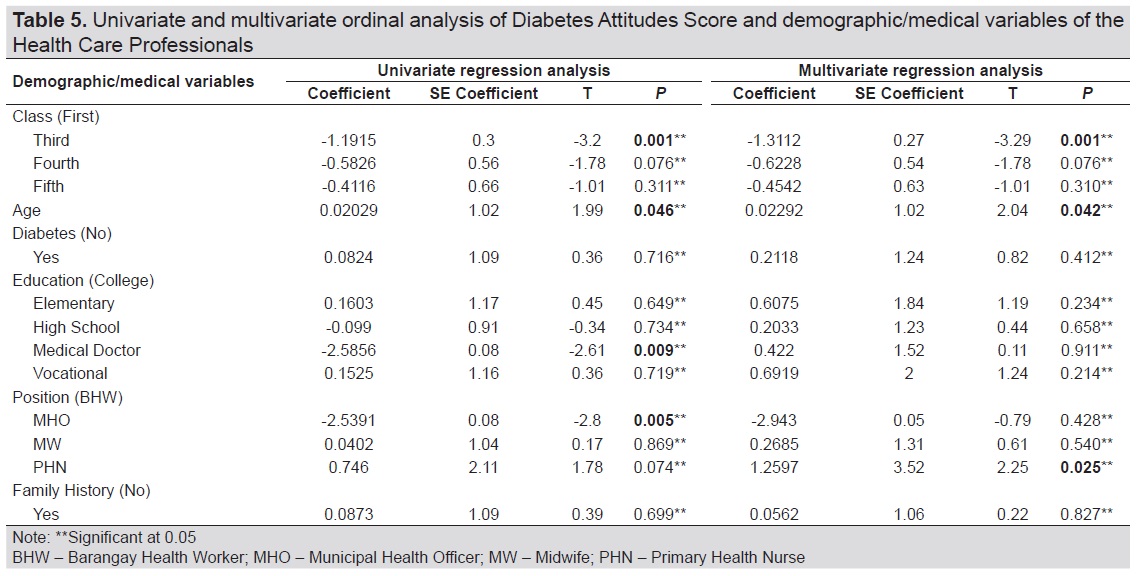
Table 5. Univariate and multivariate ordinal analysis of Diabetes Attitudes Score and demographic/medical variables of the Health Care Professionals
In the multivariate logistic regression analysis, third class municipality, age, and primary health nurses (PHN) are also statistically significant. The coefficients and odds ratios indicate that the health care professionals from third class municipalities are more likely to respond “very positive” than those from first class municipalities; the older the health care professional is, the more likely he/she is to respond “neutral;" and primary health nurses (PHN) is more likely to respond "neutral” than the BHW.
This study shows that rural health center healthcare professionals generally have neutral diabetes-attitude scale. Health care professionals showed the most positive response towards the issue of “Need for Special training in education” and least responsive towards “Seriousness of Type 2 Diabetes,” which is a neutral response. Factors that consistently affect the attitude scores of healthcare professionals include highest educational attainment and the health care professional’s position.
The subscale “Need for Special Training in Education” assesses the respondent’s attitude about the need for health care professionals who care for patients with diabetes to have special training in teaching, counseling, and behavior change techniques. In this study, health care professionals scored positively (4.13) in this subscale, reflecting the importance of training in improving effective communication to patients regarding daily diabetes care. In this subscale, medical doctors scored a very positive attitude score as compared to other health care professionals.
The importance of being adept in proper counseling among health care professionals is that this will allow them to be effective in communicating the basics of diabetes education and care to their patients. This will also enable them to confidently clarify frequently asked questions and correct the patient's misconceptions.[11]
The subscale of 'Psychological Impact of Diabetes’ and 'Autonomy of Diabetes for Patients’ have mean scores that are generally positive. This shows that healthcare professionals, in general, have a positive attitude towards issues concerning on how diabetes affects patient’s daily lives and empowering the role of patients for selfautonomy in management of their problems. Attitude towards these subscales could be further improved with continuous medical education and training of the healthcare professionals.
It is alarming that the majority of the respondents are least responsive towards 'seriousness of type 2 diabetes' and 'value of tight glucose control'. 'Seriousness of type 2 diabetes’ scale assesses the respondents’ attitude towards the belief that type 2 diabetes is a serious disease. On the other hand, the 'overall value of tight glucose control’ scale assesses the respondent’s attitude about whether the potential benefit of tight glucose control is justified in terms of the cost to the patients. The attitude toward both of these subscales is vital because it influences the health care provider's aggressiveness in patient management and prevention of complications. The results show that the majority of the health care providers, except for medical doctors, still take type 2 diabetes and its complications lightly. The measly attitude score reflects the seeming lack of awareness regarding the nature of type 2 diabetes and its chronic complications among health care providers.
This poor awareness is also true regarding the overall benefits of good sugar control in the prevention of longterm complications brought about uncontrolled diabetes. The need to address the prevention of microvascular and macrovascular complications in both Type 1 and Type 2 Diabetes has been emphasized in both Diabetes Control and Complications Trial (DCCT) and United Kingdom Prospective Diabetes Study (UKPDS).[12],[13] Both these landmark studies and their respective follow-up studies, have shown that tight glycemic control significantly lowers the occurrence of both microvascular and macrovascular complications.
The reason in which attitude towards 'value of tight glucose control' might have garnered a low score by health care providers is the misconception that complications brought about by diabetes are inherent to the disease and are not related to glucose control.[8] Another factor is the fear of overtreatment and the risk of hypoglycemia. This fear of hypoglycemia might be attributed to overall poor basic knowledge of diabetes care among healthcare workers, thus the fear of hypoglycemia limit the goal for intensive glucose control. This is seen in the previous study by Nakar et al., in which it showed that the fear of hypoglycemia is the most common reason for not starting insulin therapy on both physicians and patients.[14]
The overall mean scores of this study are comparable to previous studies done in Argentina, Yemen, and United Arab Emirates (UAE) (See Table 6).[6],[15],[16] It showed a similar trend in which high scores are garnered in 'need for special training in education and autonomy for patients,’ while subscales that consistently fared the lowest are the 'seriousness of diabetes' and 'the value of tight glucose control'. Using analysis of variance to compare attitude scores among health care professionals from different countries, it showed that Argentina and United Arab Emirates (UAE) have significantly higher scores in the subscales of 'need special training,' 'seriousness of diabetes' and 'value of tight glucose control' as compared to this local study. This could be explained by the sample population included in the Argentina and UAE studies. Both the Argentina and UAE studies included only professional and licensed health care providers who got certifying exams, while in this local study, more than half of the population are barangay health workers (BHW), of which 50% are only high school graduates and did not undergo certifying exams.
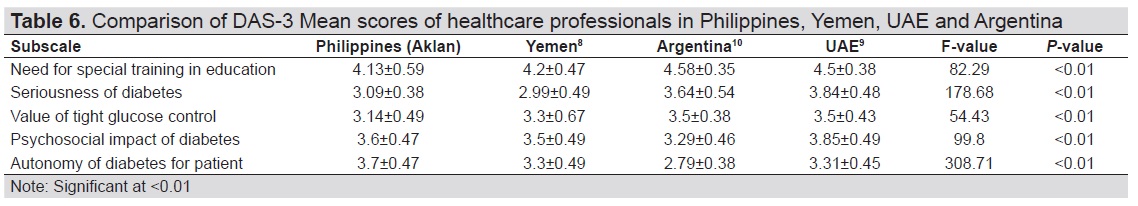
Table 6. Comparison of DAS-3 Mean scores of healthcare professionals in Philippines, Yemen, UAE and Argentina
Barangay health workers (BHWs), or known internationally as Community Health Workers (CHW), play a huge and essential role in terms of the scope of the population served, being the first line in the health care delivery system. The Philippine law, by Republic Act 7883, refers to a Barangay Health Worker as a person who voluntarily renders primary health care services in the community after undergoing accredited training under the guidelines set by the Department of Health (DOH). Their primary function is to provide information, education, and motivation services for primary health care, maternal and child health, family planning, and nutrition in the communities they live in. Unfortunately, the majority of the BHWs lack competency and basic training in effectively performing their duties which was seen in a local study by Dagangon et al. The results of that study showed that BHWs lack sufficient knowledge and skills in areas of BHW orientations, safer motherhood, women’s health, children’s health and interpersonal health.[17] Moreover, their functions go beyond what was mentioned earlier, because, in reality, they are also utilized as an adjunct to physicians and nurses in national programs such vaccination, deworming, tuberculosis program and non-communicative diseases such as diabetes. The imbalance between the BHW’s level of training and the programs thrust to them leads to inadequate and ineffective health care delivery. This same pattern of the inadequacy of training is evident in this present study as reflected by their poor diabetes-related attitude scores as compared to other members of the rural health center, who are professionally certified.
In contrast, this local study has the highest score in “autonomy of patients” and garnered second only to UAE in issues concerning 'psychosocial impact of diabetes'. This data showed that each country differs in attitudes toward a particular subscale, possibly because of cultural differences.
In analyzing factors that might be associated with the attitude scores of this local study, results of univariate and multivariate regression analysis and univariate and multivariate ordinal regression analyses showed that degree of educational attainment and work position has consistently shown a positive correlation to mean attitude scores. This association is consistent with an earlier study by Steele et al., in which it showed that the lowest educated individuals have a higher risk of developing Type 2 Diabetes and its complication during the follow-up period as compared to patients who are highly educated.[18] It is expected that the municipal health physicians have superior knowledge as compared to other members of the health unit because of their rigorous training and regular attendance in continuous medical education (CME). Therefore, there is a need to improve the knowledge gap between the physicians and other members of healthcare providers, by supporting them to undergo regular continuous medical education, especially in diabetes care.
Other factors that significantly affect mean attitude score are age and health care professionals coming from the third class municipalities. The coefficients and odds ratios indicate that the health care providers from the third class municipalities are more likely to respond “very positive” than those from first-class municipalities. The result is counter-intuitive since it is expected that those coming from first class municipalities should have better diabetes-related attitudes since they have easier access to CME and have more well-equipped health facilities. This goes to show that belonging to rural health center of a lower class municipality is not a hindrance in improving diabetes-related attitude through CMEs. The other factor is age, in which older health care providers are more likely to respond with a “neutral” attitude score. This can be explained by the accumulation of training and experience dealing with patients with diabetes through years of service.
Other factors did not show a significant association with mean attitude scores. Factors such as attendance of diabetes classes, presence of diabetes in the family, and diabetes as a co-morbid did not show a positive relationship with the DAS-3 scores. This underscores the need to improve the quality and adequacy of diabetes education given by diabetes educators to health care providers to affect their diabetes-related attitude significantly.
Limitations of the study
The limitation of this study is the small sample size and poor response rate, especially from the barangay health workers. The problem arose because the study covered the whole province of Aklan, Philippines which brings geographic and logistic limitations in reaching all barangay health workers, especially those assigned in far-flung health stations within a specific study time frame.
Using DAS-3 questionnaires, this study has shown that rural health care professionals garnered an overall positive attitude towards diabetes. Notably, they are most responsive to the need for special training among health care professionals, the psychosocial impact of diabetes and patient autonomy in caring for their condition. However, the majority of HCPs have neutral responses in “value of tight glucose control” and “seriousness of type 2 diabetes” suggesting that most of them do not believe in the benefits of controlling sugar to prevent diabetes complications and the seriousness of the disease. Among the factors considered, educational attainment and work position was found out to be the consistent factors that affect the diabetes-related attitude of HCPs. This suggests that education and training impacts in improving the diabetes-related attitude of HCPs. Therefore, there is a need to strengthen continuous medical education among the first line of health care providers, especially the midwives and the Barangay health care workers.
Recommendations
This study recommends increasing the scope of the population of this study to include rural health centers across the country. In this way, it could provide baseline data which could accurately determine the attitudes towards diabetes of health care providers in the country. A posttest can be done after an intervention is given, such as formal diabetes classes and workshops using DAS-3 used in this study to assess the effectivity of the intervention given. Furthermore, assessment can be done not only to the health care providers of rural health centers but also those belonging to the urban City Health Centers as well.
Acknowledgments
The authors thank the Association of Municipal Health Officer of the Philippines (AMHOP) – Aklan Chapter and the Section of Endocrinology, Diabetes, and Metabolism of the Chong Hua Hospital for its invaluable support for this research.
Statement of AuthorshipAll authors certified fulfillment of ICMJE authorship criteria.
Author DisclosureThe authors declared no conflict of interest
Funding SourceNone.
[1] World Health Organization. Philippines - Diabetes country profiles. Accessed July 4, 2017.
http://www.who.int/diabetes/country-profiles/phl_en.pdf?ua=1
[2] Fojas MC, Lantion-Ang FL, Jimeno CA, et al. Complications and
cardiovascular risk factors among newly-diagnosed type 2 diabetics in
Manila. Philipp J Intern Med. 2009 May;47(3):99-105.
[3] Department of Health. The Philippine health system at a glance. Accessed August 9, 2017.
https://www.doh.gov.ph/sites/default/files/basic-page/chapter-one.
pdf
[4] Paz-Pacheco E, Jimeno C. Diabetes care in the Philippines. J ASEAN Fed
Endocr Soc. 2015;30(2):118-25.
[5] Grundy J, Healy V, Gorgolon L, Sandig E. Overview of devolution of
health services in the Philippines. Rural Remote Health. 2003;3(2):220.
[6] Gagliardino JJ, González C, Caporale JE; Diabetes Education Study
Group of Argentina. The diabetes-related attitudes of health care
professionals and persons with diabetes in Argentina. Rev Panam
Salud Pública. 2007;22(5):304-7.
[7] Anderson RM, Fitzgerald JT, Funnell MM, Gruppen LD. The third
version of the Diabetes Attitude Scale. Diabetes Care. 1998;21(9):1403-
7.
[8] Yao, CS, Jimeno, CA, Trajano-Acampado, L. A survey of diabetesrelated
attitudes among patients at the UP-PGH patient department
using the Filipino version of the Diabetes Attitude Scale (DAS-
3). Philipp J Intern Med. 2004; 42:261–74.
[9] Ardeña GJ, Paz-Pacheco E, Jimeno CA, Lantion-Ang FL, Paterno E,
Juban N. Knowledge, attitudes and practices of persons with type
2 diabetes in a rural community: Phase I of the community-based
Diabetes Self-Management Education (DSME) Program in San Juan,
Batangas, Philippines. Diabetes Res Clin Pract. 2010;90(2):160-6.
[10] Department of Finance. Department Order No.23-08: Prescribing
the new income brackets for the re-classification of provinces, cities
and municipalities and amending for the purpose Department Order
No. 20-05, dated July 29, 2005. July 29, 2008. Accessed July 4, 2017.
[11] Toledo MM, Rodrigues Costa JS, da Silva E. Diabetes educator:
Current perspectives on their importance (editorial). JSM Diabetol
Manag. 2016;1(1):1001.
[12] Lifetime benefits and costs of intensive therapy as practiced in the
diabetes control and complications trial. The Diabetes Control and
Complications Trial Research Group JAMA. 1996;276(17):1409-15.
[13] Intensive blood-glucose control with sulphonylureas or insulin
compared with conventional treatment and risk of complications in
patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes
Study (UKPDS) Group. Lancet. 1998;352(9131):837-53.
[14] Nakar S, Yitzhaki G, Rosenberg R, Vinker S. Transition to insulin
in Type 2 diabetes: Family physicians' misconception of patients'
fears contributes to existing barriers. J Diabetes Complications.
2007;21(4):220-6.
[15] Babelgaith SD, Alfadly S, Baidi M. Assessment of the attitude of health
care professionals towards diabetes care in Mukalla, Yemen. Int J
Public Health Sciences. 2013;2(4):159-64.
[16] Bani-issa W, Eldeirawi K, Al Tawil H. Perspectives on the attitudes
of healthcare professionals toward diabetes in community health
settings in United Arab Emirates. JDM. 2014;5(1):1-11.
[17] Dagangon LH, Perez GG, Tupas MS. Training needs analysis of
barangay health workers of Davao City. UIC Research Journal.
2018;20(1):207-29.
[18] Steele CJ, Schöttker B, Marshall AH, et al. Education achievement
and type 2 diabetes—what mediates the relationship in older adults?
Data from the ESTHER study: A population-based cohort study. BMJ
Open. 2017;7(4):e013569.
PubMed PubMed Central
CrossRef
Authors are required to accomplish, sign and submit scanned copies of the JAFES Author Form consisting of: (1) Authorship Certification, that all the requirements for authorship have been met by each author, and that the final version of the manuscript has been read and approved by all authors; (2) the Author Declaration, that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere; (3) the Statement of Copyright Transfer [accepted manuscripts become the permanent property of the JAFES and are licensed with an Attribution-Share Alike-Non-Commercial Creative Commons License. Articles may be shared and adapted for non-commercial purposes as long as they are properly cited]; and the ICMJE form for Disclosure of Potential Conflicts of Interest. For original articles, authors are required to submit a scanned copy of the Ethics Review Approval of their research as well as registration in trial registries as appropriate. For manuscripts reporting data from studies involving animals, authors are required to submit a scanned copy of the Institutional Animal Care and Use Committee approval. For Case Reports or Series, and Images in Endocrinology, consent forms, are required for the publication of information about patients; otherwise, appropriate ethical clearance has been obtained from the institutional review board. Articles and any other material published in the JAFES represent the work of the author(s) and should not be construed to reflect the opinions of the Editors or the Publisher.