Prof. Olivia T. Sison, MSPH
Research Assistant Professor
Institute of Clinical Epidemiology, National Institutes of Health,
University of the Philippines Manila, 623 Pedro Gil Street, Ermita
Manila, Philippines 1000
Telefax: +632-8525-4098
E-mail: otsison@up.edu.ph
ORCiD: https://orcid.org/0000-0002-0929-3052
e-ISSN 2308-118x
Printed in the Philippines
Copyright © 2019 by the JAFES
Received May 13, 2019. Accepted August 14, 2019.
Published Online First: November 10, 2019.
Objective. This study aimed to estimate the prevalence of cardiovascular risk factors and metabolic syndrome among community health workers (CHWs) in selected villages in the Philippines. It also determined the association of urbanization and socio-demographic characteristics with hypertension, diabetes mellitus and metabolic syndrome among CHWs.
Methodology. A cross-sectional study was conducted among CHWs who were actively rendering service from selected communities at the time of the study. Standardized interviews were conducted and clinical measurements were collected.
Results. Of the total of 457 CHWs who participated, 96% were females with a median age of 50 years. The prevalence of hypertension in this population was 32.4%. Hypertension was found to be associated with older age [adjusted odds ratio (aOR) 5.3, 95% CI: 3.2 to 8.8, p<0.001], obesity (aOR 2.4, 95% CI: 1.4 to 4.0, p=0.002) and alcohol consumption (aOR 1.7, 95% CI: 1.0 to 3.0, p<0.040). The prevalence of diabetes mellitus (DM) was 13.6%. It was found to be more prevalent among CHWs who were at least 50 years old (aOR 2.7, 95% CI: 1.4 to 5.1, p=0.002), and those who spent at least 5 hours a day in sedentary activities (aOR 3.8, 95% CI: 1.1 to 12.7, p<0.033). Borderline to high total cholesterol, low density lipoprotein cholesterol (LDL-c) and triglycerides (TG) were seen in 41%, 37% and 20%, respectively. Sixty percent had low high density lipoprotein cholesterol (LDL-c). The overall prevalence of metabolic syndrome was 52.3%.
Conclusion. Metabolic syndrome is prevalent among CHW participants, with obesity, hypertension and low LDL-c as the most common components present. The prevalence of cardiovascular risk factors in this population was not found to be significantly different between rural and urban areas after adjusting for other factors.
Keywords: community health workers, hypertension, diabetes mellitus, metabolic syndrome, cardiovascular diseasesCommunity health workers, as in many other countries, are the front liners in the delivery of primary health care at the grassroots level, both in urban and rural communities in the Philippines. The term CHWs embraces a variety of community health aides who are selected, trained and are working in the communities from which they come. According to the World Health Organization (WHO), CHWs should be: (1) members of the communities where they work, (2) selected by the communities, (3) answerable to the communities for their activities, (4) supported by the health system but not necessarily as part of its organization, and (5) should have shorter training than professional workers.[1]
In the Philippines, CHWs refer mainly to Barangay Health Workers (BHWs) although CHWs can also include Barangay Nutrition Scholars (BNSs), Rural Health Midwives (RHMs) and Mother Leaders (MLs). In some areas of the country, there are MLs who perform the same roles as BHWs. Mostly females, BHWs are volunteers who are supposed to be accredited by the Local Health Board (LHB) and who have been trained to provide primary health care services in the community in accordance with the guidelines promulgated by the Department of Health (DOH).[2] The number of health workers in the community is set by the DOH. It is determined by the ideal ratio of BHWs relative to the number of households, provided that the total number of BHWs nationwide shall not exceed one percent (1%) of the total population.[2]
BHWs, usually of age 20 to 45 years, play significant roles in providing primary health care in the communities they serve.1 A study conducted in Camarines Sur in the Luzon island in the Philippines reported that majority of BHWs were women, age 45 and above. BHWs are considered competent as community organizers, health educators, and healthcare service providers, although continuing education may be warranted so that they will be more adept in their knowledge and skills.[3] Given that the BHWs are aging, it can be surmised that they also have medical conditions such as hypertension, diabetes and other cardiovascular diseases (CVD). A large body of epidemiologic studies likewise demonstrated associations between CVD and common lifestyle determinants including tobacco use, alcohol, physical inactivity, obesity, and diet. Urbanization was also believed as one of the key drivers of non-communicable diseases especially in lowand middle-income countries.[4]
The limited literature about CHWs were mainly about the definition of CHWs, their general functions, level of competence and existing CHW programs. CHWs are expected to take care of the health of their community members. Ironically, there is no existing program that has been cited in the literature that paid attention to the health of the aging CHWs. In the Philippines, to the best of our knowledge, the cardiovascular risk profile of CHWs has not been studied. Paradoxically, the CHWs are advocates for promoting health through education and dissemination of information. The CHWs must be in good health condition in order to perform better in the delivery of health services in the communities.
CHWs have been identified as one strategy in addressing the growing shortage of health workers, particularly in low-income countries.1 On average, each health worker is expected to work with approximately 20 families in their communities.[5] In the Philippines, BHWs are considered as volunteers under Republic Act (R.A.) No. 7833, known as The Barangay Health Workers’ Benefits and Incentives Act of 1995. Only a few BHWs in the barangay (village) receive a modest allowance from the Local Government Unit (LGU). Availability of allowance depends on factors such as LGU income and political considerations. Various bills have been proposed to improve the benefits and incentives of BHWs. The latest is the one filed by Senator Grace Poe, Senate Bill No. 2219, an act to improve and promote quality delivery of health services in barangays, enacting the BHWs and services reform act of 2014. This Senate Bill states that: (1) the entry pay level of a BHW shall be the prevailing rate equivalent to Salary Grade One (SG 1), (2) BHWs shall be entitled to the same incentives and benefits provided under the Magna Carta for Public Health workers, and (3) BHWs shall be covered by the existing statutory benefits from the Government Service Insurance System (GSIS), the Philippine Health Insurance Corporation (PhilHealth) and the affordable shelter financing program, Pagtutulungan sa Kinabukasan: Ikaw, Bangko, Industriya at Gobyerno (Pag-IBIG).[6]
CHWs, in general, perform a wide range of tasks including home visits, environmental sanitation, first aid and treatment of simple and common ailments, health education, nutrition and surveillance, maternal and child health and family planning activities, TB and HIV/ AIDS care (i.e. counselling, peer and treatment support, and palliative care), malaria control, treatment of acute respiratory infections, communicable disease control, community development activities, referrals, record keeping, and collection of data on vital events. These tasks are performed in many different combinations and with varied degrees of breadth and depth in diverse countries.[7]
Objectives
This study aimed to estimate the prevalence of cardiovascular risk factors and metabolic syndrome among CHWs in selected areas in the Philippines. It also determined the association of urbanization and other sociodemographic characteristics with hypertension, diabetes mellitus, and metabolic syndrome among CHWs.
Study design and setting
This study was conducted in conjunction with the main LIFEcourse study in CARdiovascular disease Epidemiology (LIFECARE). The LIFECARE study is a community-based prospective cohort of apparently healthy individuals aged 20 to 50 years old that examined the effects of socioeconomic factors, psychosocial stress and lifestyle factors in the development of cardiovascular disease risk factors and CVD.[8] Unlike the main LIFECARE study, this sub-study on CHWs was cross-sectional in design with just one data collection point and no specific age range for enrolment in the study. This sub-study was conducted in 2 selected urban barangays in Metro Manila, and in 54 urban and rural barangays in Central and Southern Luzon (provinces of Batangas, Bulacan, Rizal, and Quezon). Participants were CHWs who were actively rendering service from the selected communities at the time of the study. Standardized interviews were conducted and clinical measurements were done. Informed written consent was obtained from participants prior to the interview. The study was approved by the University of the Philippines Manila Research Ethics Board (UPMREB 2008-027-01).
Trained research assistants interviewed and conducted clinical measurements. The clinical evaluation and collection of samples were carried out at screening centers set up at the barangay health centers of the selected barangays. The participants’ anthropometric data such as height, weight, waist and hip circumferences were taken. The weight was measured using the standardized bathroom scale (10 kg weight was used). The height was measured with a stadiometer. The waist circumference was determined at midway between the sub-costal margin and the iliac crest while the hip circumference was taken at the widest diameter. The blood pressure measurements were taken in the seated position 3 times in the upper arm using an Omron digital sphygmomanometer with appropriate cuff sizes and validated by the Philippine Society of Hypertension. One to 2 tablespoons (10 mL) of fasting blood was taken from each participant and transferred into a plain vial for blood chemistry. Analysis of fasting blood glucose was done in a central laboratory using Roche Cobas Mira blood analyzer. All samples were analyzed at the Department of Medicine’s Lipid Research Laboratory in the Philippine General Hospital. The total cholesterol and triglycerides were measured by enzymatic colorimetric method and high-density lipoproteincholesterol and low-density lipoprotein-cholesterol by differential precipitation enzymatic colorimetric using semi-autoanalyser Mitra Photometer. All parameters were expressed as mmol/L.
Hypertension was defined as systolic blood pressure (SBP) ≥140 mmHg or diastolic blood pressure (DBP) ≥90 mmHg or both, and/or concomitant use of antihypertensive medications according to the WHO/International Society of Hypertension (ISH) guidelines.[9]
The current WHO diagnostic criteria for diabetes was used, which included a fasting plasma glucose (FPG) ≥7.0 mmol/L (126 mg/dL) or a 2-hour plasma glucose ≥11.1 mmol/L (200 mg/dL), and/or concomitant use of antidiabetic medications.[10]
Cut-off values for lipid profile were adopted from the National Cholesterol Education Program Adult Treatment Panel 3 (NCEP ATP III) report. Dyslipidemia was defined as having one of the following: high TC (≥6.2 mmol/L), high TG (≥2.26 mmol/L), high LDL-c (≥4.1 mmol/L) and/or low LDL-c (<1.03 mmol/L for male and <1.29 for female).[11]
The diagnosis of metabolic syndrome was based on the interim statement of the International Diabetes Federation (IDF) Task Force composed of several major organizations. Three abnormal findings out of 5 would qualify a person for the metabolic syndrome, and that abdominal obesity will not be a prerequisite for diagnosis but will continue to be a useful tool for screening.[12] The harmonized criteria defined the following component risk factors: (1) elevated BP with SBP ≥130 mmHg or DBP ≥85 mmHg or on drug treatment, (2) elevated TG ≥1.7 mmol/L or on drug treatment, (3) elevated FBG ≥5.5 mmol/L or on drug treatment, (4) low HDL-c <1.0 mmol/L for men and <1.3 mmol/L for women or on drug treatment, and (5) abdominal obesity or increased waist circumference of ≥90 cm for men and ≥80 cm for women for Asians.
Rural and urban classification or geographic location of barangays was based on the Philippine Statistics Authority definition. This was determined in terms of population size, number of establishments and employees, and available facilities (e.g. town hall or provincial capitol, church, public plaza, market place, public buildings, etc.).
Body mass index (BMI) was calculated as weight in kilograms divided by squared height in meters (kg/m2). The current WHO BMI cut-off points were as follows: <18.5 kg/m2 (underweight), 18.5 to 24.9 (normal), 25 to 29.9 (overweight), and ≥30 (obese). For adult Asians, the proposed BMI categories were as follows: <18.5 kg/m2 (underweight), 18.5 to 22.9 (normal), 23 to 24.9 (overweight), and ≥25 (obese).[13]
Participants were also classified as current smoker if they answered “Yes” to the question, “Do you presently smoke cigarettes, cigars, pipes or any other tobacco products?”
Alcohol consumption was based on the question, “In your entire life, have you ever consumed one or more drinks of any type of alcoholic beverage?” Another question on the frequency of alcohol consumption in the past 12 months was also included.
Physical activity includes exercise as well as other activities which involve bodily movement and are done as part of playing, working, active transportation, house chores and recreational activities.[14] In adults aged 18 to 64, physical activity includes leisure time physical activity (e.g. walking, dancing, gardening, hiking, swimming), transportation (e.g. walking or cycling), occupational (i.e. work), household chores, play, games, sports or planned exercise, in the context of daily, family, and community activities. For this study, recreation-related activities such as sports and fitness that cause large increases in breathing or heart rate for at least 10 minutes continuously were estimated for each participant (both moderate and vigorous-intensity recreation-related). Moreover, average amount of hours per day spent for sedentary activities such as sitting or reclining were also calculated.
Statistical analysis
A total of 449 CHWs from the selected communities was required to estimate the prevalence of low HDL-c in this population within the interval (64±5%) with a 95% confidence level, adjusted to a 20% non-response. This was considered the final sample size and was deemed sufficient to cover estimation of prevalence of all other cardiovascular risk factors. Descriptive statistics such as mean, standard deviation, median and range were calculated for continuous variables while frequency and percentages were presented for categorical variables. Differences in demographic and clinical characteristics by geographical location and health status were analyzed using independent t-test, Mann-Whitney U test, and Chisquare test, where appropriate. Bivariate analysis and multivariate logistic regression determined the association of urbanization and other selected demographic and anthropometric measures with hypertension, diabetes and metabolic syndrome. Crude and adjusted odds ratios with 95% confidence intervals, and p values were derived. A p value of less than 0.05 was considered significant. All statistical analyses were performed using Stata© version 14.[15]
Ethical considerations
The study was approved by the institutional review board of the University of the Philippines Manila (UPMREB 2008- 027-01). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Written informed consent was obtained from all individual participants included in the study.
A total of 457 CHWs were interviewed in this study: 96% were females with a median age of 50 years and age range of 20 to 78 years (Table 1). Sixty percent of the CHWs were from urban barangays. Majority of the participants were married, and more than half reached at least high school level of education. Six out of 10 participants were BHWs, and another 20% were Mother Leaders who performed similar functions as BHWs. There were 3 CHWs who reported that they performed multiple roles in their barangay (e.g. serving as BHW and BNS at the same time). Twenty six percent said that they had ever consumed at least one drink of any type of alcoholic beverage in the past 12 months, and majority consumed alcoholic beverage less than once a month. There were 2 female CHWs who reported daily consumption of any type of alcoholic beverage in the past 12 months. No significant differences found in lifestyle activities between CHWs in rural and urban areas except for physical inactivity. Six percent of the participants were current smokers and the proportion of current smokers was higher among those in rural areas (9%) compared to those in urban areas (4%) although not statistically significant. In terms of physical activity, almost half of the CHWs reported to have done any recreation-related activity (moderate to vigorous-intensity sports, fitness and recreation activities) averaging to about 30 minutes per day. CHWs from urban areas had higher time spent for recreation activities than CHWs from rural areas (p=0.044). Moreover, the average amount of time spent for sedentary activities (sitting or reclining) reported by CHWs was estimated to be about 8 hours per day. This was higher among CHWs from urban areas compared to those from rural areas (p=0.012).
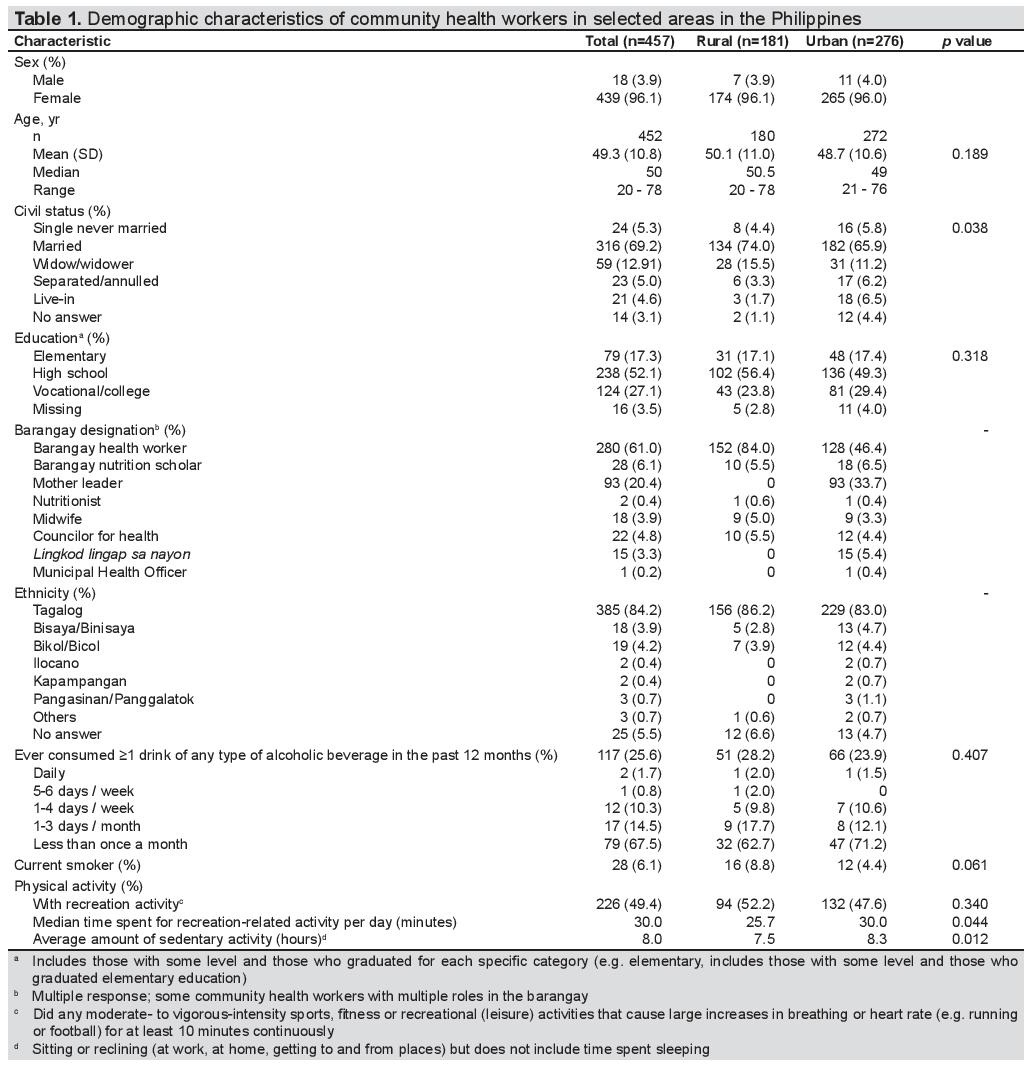
Table 1. Demographic characteristics of community health workers in selected areas in the Philippines
Table 2 shows the prevalence of cardiovascular risk factors by geographical location. The overall prevalence of overweight was 33% by WHO and 21% by Asia Pacific classification. Meanwhile, the overall prevalence of obesity was 11.2% by WHO and 43.8% by the Asia Pacific classification. There were more CHWs who were obese in urban areas using either criterion. The overall prevalence of hypertension was 32.4%, almost two-thirds of which were at stage 1. Three out of 10 CHWs were in the pre-hypertensive level. Furthermore, the overall prevalence of diabetes mellitus was at 13.6%, more commonly in CHWs in urban compared to rural areas. The percentage of CHWs with low HDL-c was higher in rural compared to those from urban areas (p=0.006). On the other hand, the percentage of CHWs with heart rate of at least 70 bpm was higher in urban compared to those in rural areas (<0.001).
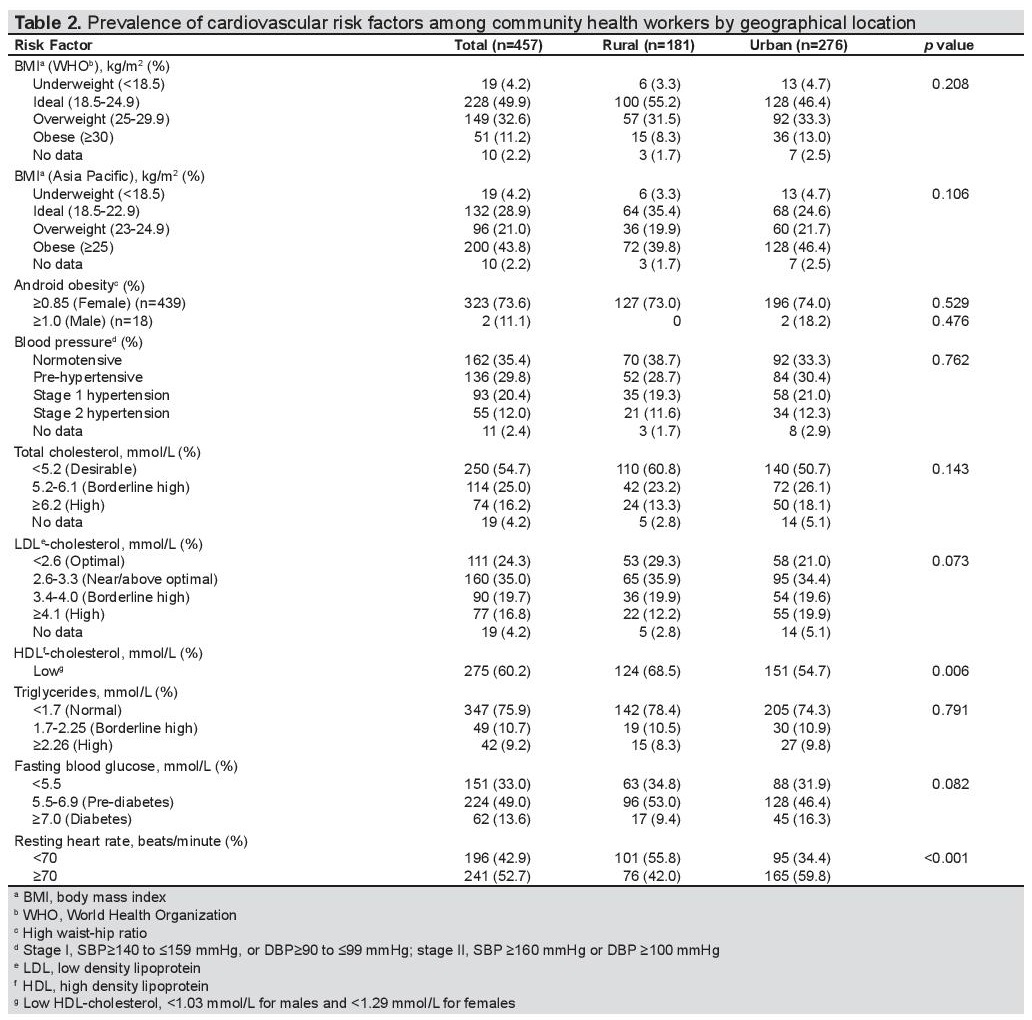
Table 2. Prevalence of cardiovascular risk factors among community health workers by geographical location
Table 3 presents the prevalence of hypertension and diabetes mellitus among CHWs by urbanization and other selected demographic and anthropometric characteristics. By bivariate analysis, hypertension was not found to be significantly different between rural and urban locations. Conversely, significant factors found to be associated with hypertension were age (at least 50 years old), civil status (without domestic partner), educational attainment (elementary level of education), and BMI (overweight/ obese). Multivariate logistic regression analysis showed that age (aOR 5.3, 95% CI: 3.2 to 8.8, p<0.001), obesity (aOR 2.4, 95% CI: 1.4 to 4.0, p=0.002), and alcohol consumption (aOR 1.7, 95% CI: 1.0 to 3.0, p<0.040) were strongly associated with hypertension. On the other hand, diabetes mellitus was found to be associated with geographical location, age and time spent in sedentary activities by bivariate analysis. The prevalence of diabetes was higher among CHWs at least 50 years old (aOR 2.7, 95% CI: 1.4 to 5.1, p=0.002), and those who spent at least 5 hours in sedentary activities (aOR 3.8, 95% CI: 1.1 to 12.7, p<0.033) by multivariate analysis.
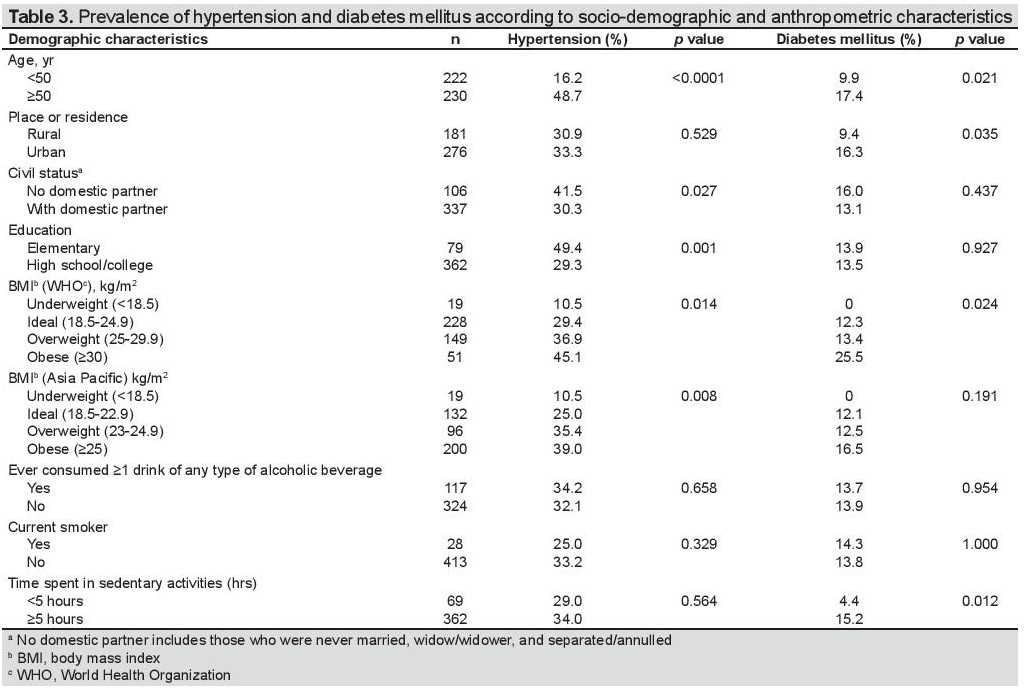
Table 3. Prevalence of hypertension and diabetes mellitus according to socio-demographic and anthropometric characteristics
Amount of physical activity was compared in those with and without hypertension (Table 4). The amount of time doing recreation-related activities and sedentary activities was not found to be significantly different between CHWs with or without hypertension. On the other hand, the average time doing sedentary activities such as sitting and reclining (excluding sleeping) was higher among CHWs with diabetes compared to those without diabetes (p=0.048) (Table 5).
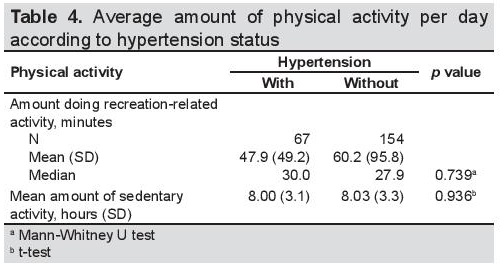
Table 4. Average amount of physical activity per day according to hypertension status
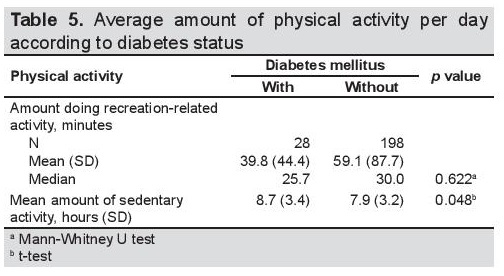
Table 5. Average amount of physical activity per day according to diabetes status
The prevalence of metabolic syndrome and component risk factors in this population are shown in Table 6. The overall prevalence of metabolic syndrome was 52.3%. Among the component risk factors of metabolic syndrome, the prevalence of low HDL-c among CHWs from rural areas was higher compared to those from urban areas (p=0.006). The prevalence of metabolic syndrome was higher with increasing age and among those with lower level of education (Table 7).
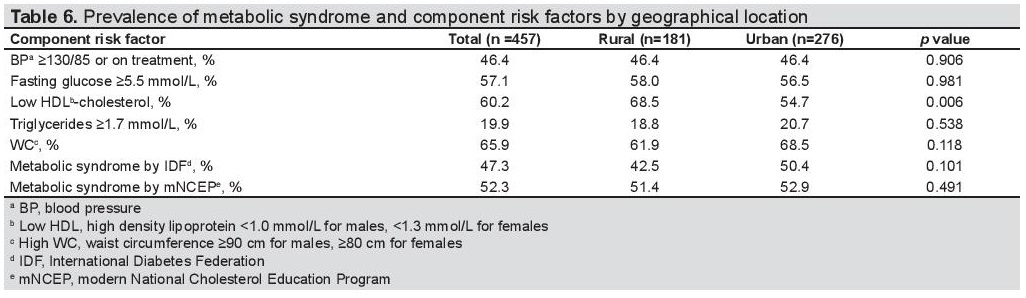
Table 6. Prevalence of metabolic syndrome and component risk factors by geographical location
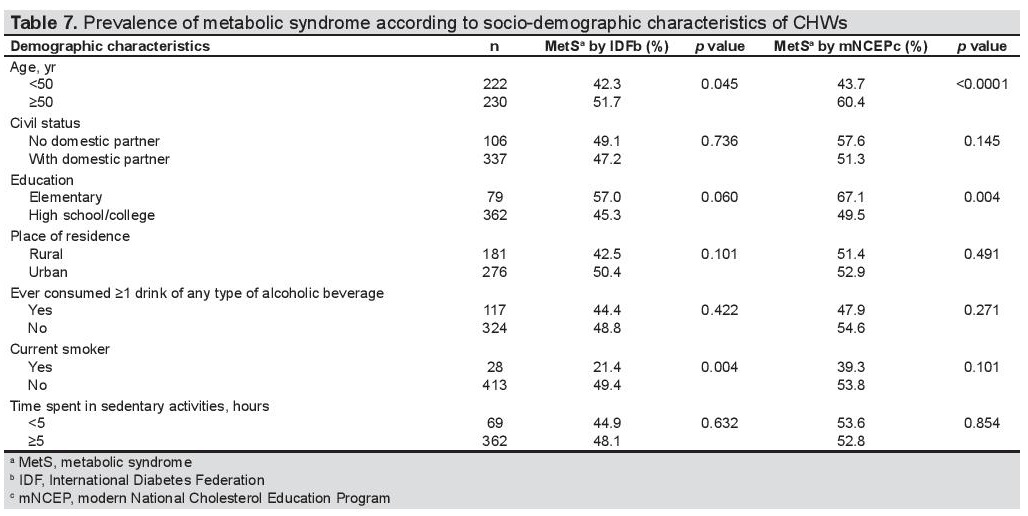
Table 7. Prevalence of metabolic syndrome according to socio-demographic characteristics of CHWs
To the best of our knowledge, this is the first study in the Philippines about cardiovascular risk profile and metabolic syndrome in CHWs. It is significant to note that the prevalence of cardiovascular risk factors was common among CHWs who participated in this study.
The results of the 8th National Nutrition Survey (NNS) done in 2013 by the Food and Nutrition Research Institute of the Department of Science and Technology (FNRIDOST) showed that more Filipinos have hypertension, high fasting blood sugar (FBS) and high cholesterol and triglyceride levels, which are risk factors for cardiovascular diseases, diabetes and other lifestyle-related diseases.[16] One in every 4 Filipino adults has hypertension or a blood pressure (BP) reading equal to or higher than 140/90. In the Asia-Pacific Region, the prevalence of hypertension ranges from 5 to 47% in men and 7 to 38% in women.[17] In other developing countries like Nigeria, the prevalence of hypertension is even higher at 35.4% in the semi-urban community as against 25.1% in rural community.[18]
The prevalence of high fasting blood sugar, an indicator of diabetes mellitus, is 5 in every 100 Filipinos, based on the 8th NNS. The prevalence of high FBS or hyperglycemia peaks at age 50 to 59 years. The NNS also showed that almost half of Filipino adults had borderline to high TC level. More than one-third of Filipinos have borderline to high TG level. The prevalences of low HDL-c and borderline to high LDL-c levels were 71% and 47%, respectively.[16]
Compared to the health profile of in this study of CHWs, the 8th NNS showed a higher overall prevalence of current smokers, borderline to high TC, TG, LDL-c, and low HDL-c. On the other hand, this study showed a higher prevalence of obesity (11.2% by WHO and 43.8% by the Asia Pacific classification), hypertension (32.4%) and diabetes (13.6%) compared to the national data. These two populations may not be comparable since majority of the CHWs in this study were females and older with a median age of 50 years, compared with the NNS adult population which was randomly selected nationwide.
The current policy under R. A. 7833 considers BHWs as merely volunteers. CHWs, in general, were mostly females. One usual explanation for this is the cultural expectations and social norms that men are supposed to be breadwinners while women are homemakers, which includes the role of taking care of the sick. Majority of Filipino males have full-time jobs, and more women are out of the workforce. The 2016 Labor Force Survey showed that 78% of Filipino men are in the labor force compared to just 49% among women.[19] It was also observed by Najafizada in Afghanistan that female CHWs accomplished their tasks vis-à-vis maternal and child health with greater ease compared to their male counterparts. Female CHWs may be more helpful in the realm of maternal health because female patients are more comfortable sharing problems related to reproductive health to a female CHW.[20]
Six percent of the CHWs in the present study were current smokers, lower than the overall national prevalence (25%) in the 8th NNS.[16] It was expected that the prevalence of current smokers among CHWs was lower since 96% of the participants were females, and the national prevalence of current smokers among women was only 7.8%. However, the prevalence of current smokers was higher among rural CHWs compared to their urban counterparts. Rural residency has long been associated with higher rates of smoking. Based on a study in the United States, compared to their urban counterparts, rural communities have higher rates of risky behaviors such as smoking.[21]
Older age, alcohol consumption and higher BMI were independently associated with hypertension in the study population. This finding was consistent with other studies in Malaysia, India, and Kenya.[22],[23],[24],[25] Similarly, bivariate analysis showed that civil status was found to be associated with hypertension, as observed in other studies.[26],[27]7 It was hypothesized that social integration, such as marital state and cohabitation, can influence health status, specifically blood pressure level.[27] It can partly be explained that when cohabiting, there may be a social support system which is protective from having hypertension. On the other hand, the economic aspects of living alone may also be considered as a factor contributing to higher blood pressure, since married individuals potentially have higher financial resources that could promote healthy lifestyles.[26] In this study, hypertension was higher among CHWs with lower educational attainment, consistent with other studies in Malaysia and rural Delhi.[22],[25] Many researchers prefer education as an indicator of lifetime socio-economic status and it has been shown to be positively associated with better health.[28]
The prevalence of diabetes was higher among CHWs compared to the national estimate of the 8th NNS among the general adult population. Older age, those living in urban areas and those who spent at least 5 hours a day in sedentary activities were more likely to have diabetes. These findings were similar with previous studies conducted in Vietnam and South Asia. [29],[30] The cause of diabetes has been attributed to a variety of social and lifestyle factors that can be modified. Higher rate of obesity in this population may explain the high prevalence of diabetes, as it is a major contributory factor to the current diabetes epidemic.[31] The lifestyle of CHWs living in the rural areas is relatively more active as compared to those in the urban areas as indicated by the higher percentage of physical inactivity. Most people in the rural areas live and work on farms or fisheries which require physical activities such as walking, swimming, gardening, planting or fishing. The higher prevalence of diabetes in urban areas may partly be explained by the sedentary lifestyle observed in urban areas. Sedentary lifestyle is characterized by sitting or lying down while engaged in activities like reading, watching television or using mobile phones, to name a few. Environmental factors associated with cardiovascular risk factors differ widely across populations. This may be due to culture and stage of urbanization. Specific populations in different locations may adopt diverse lifestyles, and one of the most marked societal and environmental changes has been linked with urbanization.[32]
CHWs are the significant link between communities or families and the formal health systems. They are known to be effective community organizers, health educators, and health care providers. With the recent passage of R.A. No. 11223, the Universal Health Care Act, for the DOH to effectively implement their strategic thrust to attain universal health care for all, the contribution of CHWs cannot be overlooked. However, based on the results of this study, CHWs are aging and have higher rates of obesity, hypertension and diabetes compared to the general population. Their credibility as health workers is linked to their health status. Modelling healthy behaviour is a vital function of CHWs, and unhealthy behaviours and conditions among them render their ability to promote health and provide health messages less effective. Full implementation of R.A. 7883 is essential to look into the welfare of the CHWs and provide them due benefits and incentives under the Magna Carta for Public Health workers. CHWs can be considered as among the priority in appropriating budgetary allocation using the “Special Health Fund” of the Universal Health Care Act. The local authorities hiring community health workers must establish well-defined selection criteria and adopt occupational health programs to ensure effectiveness of services given by the health workers. The provision of patient support programs, such as free medicines, laboratory exams and lifestyle advice, would also improve the present health condition of CHWs in the communities. The health status of CHWs must be addressed for them to perform better in the delivery of health services in their respective communities.
The results of this study gave us an overview of the cardiovascular risk profile among CHWs from selected villages in the Philippines. These findings may be validated in a greater scale that would be representative of the CHWs nationwide. This can be made possible once the Universal Health Care law is fully implemented.
Metabolic syndrome is prevalent among CHW participants, with obesity, hypertension and low-HDL-c as the most common components of metabolic syndrome present. Older CHWs, those who consumed alcoholic drinks and those with higher BMI were more likely to have hypertension. Moreover, older CHWs and those who spent at least 5 hours of sedentary activities tended to have diabetes. The prevalence of cardiovascular risk factors in this population was not found to be significantly different between rural and urban areas after adjusting for other factors.
Acknowledgments
The authors gratefully acknowledge and thank their support team, Ms. Alma Amparo and Ms. Rona May de Vera; field interviewers, local government officials and barangay health workers who helped them in this study.
Statement of AuthorshipAll authors certified fulfillment of ICMJE authorship criteria.
Author DisclosureThe authors declared no conflict of interest
Funding SourceThis study was a sub-study of the LIFECARE Philippines and all laboratory costs were funded by the LIFECARE Philippines. Fieldwork activities for the sub-study were funded by a grant from the National Institutes of Health, University of the Philippines Manila. The main study of the LIFECARE Philippines team was supported through an investigator-initiated grant from Pfizer, Inc. Government agencies (Department of Health, Philippine Council for Health Research and Development) and professional medical associations in the Philippines (Diabetes Philippines, Philippine Society of Hypertension, Philippines Lipid and Atherosclerosis Society and Philippine Heart Association) also provided funding. Sponsors had no access to individual level data. Publication of the study results was not contingent upon sponsor’s approval
[1] World Health Organization. Strengthening the Performance of
Community Health Workers in Primary Health Care. Report of a
WHO Study Group. Geneva, Switzerland: World Health Organization,
1989.
https://apps.who.int/iris/bitstream/handle/10665/39568/WHO_
TRS_780.pdf?sequence=1&isAllowed=y>
[2] Republic Act No. 7883: Barangay Health Workers’ Benefit and
Incentives Act of 1995.
[3] Taburnal MV. Barangay health workers’ level of competence. Asia
Pac High Educ Res J. 2017;4(1):1-15.
http://po.pnuresearchportal.org/
ejournal/index.php/apherj/article/view/437/241
[4] Boutayeb A, Boutayeb S. The burden of non communicable diseases in
developing countries. Int J Equity Health. 2005;4(1):2.
[5] Barangay Health Volunteers.
[6] Senate Bill 2219: An Act to Improve and to Promote Quality Delivery of
Health Services in Barangays, Enacting the Barangay Health Workers
and Services Reform Act of 2014.
https://www.senate.gov.ph/lis/bill_
res.aspx?congress=16&q=SBN-2219
[7] Lehmann U, Sanders D. Community health workers: What do we know
about them?The state of the evidence on programmes, activities, costs
and impact on health outcomes of using community health workers.
Geneva: World Health Organization, 2007.
https://www.who.int/hrh/
documents/community_health_workers.pdf
[8] Tai ES, Poulton R, Thumboo J et al. An update on cardiovascular
disease epidemiology in South East Asia. Rationale and design of
the LIFE course study in CARdiovascular disease Epidemiology
(LIFECARE). CVD Prev Control. 2009;4:93-102.
[9] Whitworth JA, World Health Organization, International Society
of Hypertension Writing Group. 2003 World Health Organization
(WHO)/International Society of Hypertension (ISH) statement on
management of hypertension. J Hypertens. 2003;21(11):1983-92.
[10] World Health Organization. Definition and Diagnosis of Diabetes
Mellitus and Intermediate Hyperglycemia: Report of a WHO/IDF
Consultation. Geneva: World Health Organization, 2006.
https://www.who.int/diabetes/publications/Definition%20and%20diagnosis%20of%20diabetes_new.pdf
[11] National Cholesterol Education Program (NCEP) Expert Panel on
Detection, Evaluation and Treatment of High Blood Cholesterol in
Adults (Adult Treatment Panel III). Third report of the National
Cholesterol Education Program (NCEP) Expert Panel on Detection,
Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult
Treatment Panel III) final report. Circulation. 2002;106(25):3143-421.
[12] Alberti KG, Eckel RH, Grundy SM et al. Harmonizing the metabolic
syndrome: A joint interim statement of the International Diabetes
Federation Task Force on Epidemiology and Prevention; National
Heart, Lung and Blood Institute; American Heart Association;
World Heart Federation; International Atherosclerosis Society; and
International Association for the Study of Obesity. Circulation.
2009;120(16):1640-5.
[13] World Health Organization. The Asia-Pacific Perspective: Redefining
Obesity and Its Treatment. Sydney: Health Communications Australia
Pty Limited, 2000.
http://www.wpro.who.int/nutrition/documents/
docs/Redefiningobesity.pdf
[14] World Health Organization. Global Recommendations on Physical
Activity for Health. Geneva: World Health Organization, 2010. Accessed
April 20, 2005.
https://
www.who.int/dietphysicalactivity/global-PA-recs-2010.pdf
[15] StataCorp. Stata© Statistical Software: Release 14. 2015
[16] Food and Nutrition Research Institute. 8th National Nutrition Survey:
“Juan Mission for a Well-Nourished Nation.” In: 2nd National
Nutrition Summit, 2014.
[17] Martniuk AL, Lee CM, Lawes CM et al. Hypertension: its prevalence
and population-attributable fraction for mortality from cardiovascular
disease in the Asia-Pacific region. J Hypertens. 2007;25(1):73-9.
[18] Ulasi II, Ijoma CK, Onodugo OD. A community-based study of
hypertension and cardio-metabolic syndrome in semi-urban and rural
communities in Nigeria. BMC Health Serv Res. 2010;10:71.
[19] Philippine Commission on Women. Factsheets on Filipino WoMen.
2017.
[20] Najafizada SA, Labonté R, Bourgeault IL. Community health
workers of Afghanistan: a qualitative study of a national program.
Confl Health. 2014;8(26).
[21] Eberhardt MS, Pamuk ER. The importance of place of residence:
examining health in rural and nonrural areas. Am J Public Health.
2004;94(10):1682-6.
[22] Abdul-Razak S, Daher AM, Ramli AS et al. Prevalence, awareness,
treatment, control and socio demographic determinants of
hypertension in Malaysian adults. BMC Public Health. 2016;16(1):351.
[23] Bansal SK, Saxena V, Kandpal SD, Gray WK, Walker RW, Goel D. The
prevalence of hypertension and hypertension risk factors in a rural
Indian community: A prospective door-to-door study. J Cardiovasc
Dis Res. 2012;3(2):117-23.
[24] Joshi MD, Ayah R, Njau EK et al. Prevalence of hypertension
and associated cardiovascular risk factors in an urban slum in
Nairobi, Kenya: A population-based survey. BMC Public Health.
2014;14:1177.
[25] Kishore J, Gupta N, Kohli C, Kumar N. Prevalence of hypertension
and determination of its risk factors in Rural Delhi. Int J Hypertens.
2016;Article ID 78962595.
CrossRef
[26] Lipowicz A, Lopuszanska M. Marital differences in blood pressure
and the risk of hypertension among Polish men. Eur J Epidemiol.
2005;20(5):421-7.
[27] Redondo-Sendino Á, Guallar-Castillón P, Banegas JR, Rodríguez-
Artalejo F. Relationship between social network and hypertension in
older people in Spain. Rev Española Cardiol. 2005;58(11):1294-301.
[28] Kollia N, Panagiotakos DB, Georgousopoulou E et al. Exploring the
association between low socioeconomic status and cardiovascular
disease risk in healthy Greeks, in the years of financial crisis (2002-
2012): The ATTICA study. Int J Cardiol. 2016;223:758-63.
[29] Nguyen CT, Pham NM, Lee AH, Binns CW. Prevalence of and
risk factors for type 2 diabetes mellitus in Vietnam. Asia Pac J
Public Health. 2015;27(6):588-600.
[30] Kakar ZA, Siddiqui MA, Amin RA. Prevalence and risk factors of
diabetes in adult population of South Asia. Clinical Medicine and
Diagnostics. 2013;3(2):18-28.
CrossRef
[31] Nguyen HN, Fujiyoshi A, Abbott RD, Miura K. Epidemiology of
cardiovascular risk factors in Asian countries. Circ J. 2013;77(12):2851-
9.
CrossRef
[32] Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular
diseases: Part I: General considerations, the epidemiologic transition,
risk factors, and impact of urbanization. Circulation. 2001;104(22):2746-
53.
Authors are required to accomplish, sign and submit scanned copies of the JAFES Author Form consisting of: (1) Authorship Certification, that all the requirements for authorship have been met by each author, and that the final version of the manuscript has been read and approved by all authors; (2) the Author Declaration, that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere; (3) the Statement of Copyright Transfer [accepted manuscripts become the permanent property of the JAFES and are licensed with an Attribution-Share Alike-Non-Commercial Creative Commons License. Articles may be shared and adapted for non-commercial purposes as long as they are properly cited]; and the ICMJE form for Disclosure of Potential Conflicts of Interest. For original articles, authors are required to submit a scanned copy of the Ethics Review Approval of their research as well as registration in trial registries as appropriate. For manuscripts reporting data from studies involving animals, authors are required to submit a scanned copy of the Institutional Animal Care and Use Committee approval. For Case Reports or Series, and Images in Endocrinology, consent forms, are required for the publication of information about patients; otherwise, appropriate ethical clearance has been obtained from the institutional review board. Articles and any other material published in the JAFES represent the work of the author(s) and should not be construed to reflect the opinions of the Editors or the Publisher.