Gene Margaret Bernabe-Dela Victoria, MD
Section of Endocrinology, Diabetes and Metabolism
Department of Medicine, St. Luke’s Medical Center, Quezon City
279 E. Rodriguez Sr. Avenue, Quezon City, Philippines 1112
Telefax: +632-8723-0101 local 5210
E-mail: gene_bernabe@yahoo.com
ORCiD: https://orcid.org/0000-0001-6235-403X
e-ISSN 2308-118x
Printed in the Philippines
Copyright © 2019 by the JAFES
Received June 21, 2019. Accepted August 2, 2019.
Published Online First: November 10, 2019.
Introduction. Type 2 diabetes mellitus has been linked to depression. However, this has been largely unrecognized and untreated. There are no current data available in the Philippine setting of the prevalence of the disease.
Objective. The objective of the study was to determine the prevalence of depression among adult Filipino patients with type 2 diabetes mellitus and investigate the different clinical factors associated with it.
Methodology. This is a single-center, analytic cross-sectional study conducted at a tertiary hospital, with 476 patients aged above 18 years old diagnosed with type 2 Diabetes Mellitus included. The Physicians Health Questionnaire 9 (PHQ-9) with a score of >5 was used to make a diagnosis of depression.
Results. Prevalence of depression among patients with type 2 diabetes mellitus was 19.9%. Factors associated with increased odds of depression were having a post-graduate degree (p-value=0.012), presence of retinopathy (p-value=0.018), and higher MMA Score (lower adherence) (p-value=0.000).
Conclusion. Depression is prevalent among Filipino patients with type 2 diabetes mellitus. An integrated approach by the attending physicians and psychiatrists is required for the effective management of these patients.
Keywords: depression, type 2 diabetes mellitus, Filipino, PhilippinesDepression is a common public health issue which affects all aspect of a person's life and has been recognized as an important co-morbid condition in diabetes and diabetes related complications.[1] People with diabetes are almost twice as likely to suffer from depression and anxiety as the general population. But this factor remains unrecognized and thus untreated.[2] Many studies have documented the high rate of depression found among patients with diabetes, compared with non-patient control subjects.[2],[3],[4] However, minimal data had been gathered of the prevalence of it here in the Philippines.
In China, the prevalence of depression among patients with diabetes was 5.7%. Higher body mass index (BMI) score, high glycosylated hemoglobin (HbA1c) level and low health quality insurance were associated with presence of depression.[5] According to the study of Al et al., there was also increased prevalence of depression among Jordanians with diabetes which was associated with gender (female), socioeconomic status and insulin therapy.[4] In the Mexican American population, 25% presented with minor depression and 9% with lifetime diagnosis of major depressive disorder. Greater incidence of both macro- and microvascular complications and greater incidence of disability in activities of daily living were seen among depressed depressed persons with diabetes. [6] Several factors were correlated with depression in type 2 diabetes, such as low levels of education, physical inactivity, subjective somatic complaints, and physical impairment.[7] However, there has some inconsistencies of the associations between depression and HbA1C.[5],[7]
The purpose of this study was to determine the prevalence of depression and its associated clinical factors among patients with type 2 diabetes mellitus seen at a tertiary hospital in the Philippines.
This was an analytic cross- sectional study that was conducted to determine the prevalence of depression and associated factors in patients with type 2 diabetes in St. Luke’s Medical Center from May 2018 to December 2018. Inclusion criteria of the study were diagnosed with type 2 Diabetes mellitus fulfilling criteria of American Diabetes Association (FBS >126, HbA1c >6.5, symptoms with RBS>200 mg/dl); age >18 years old; and able to read and understand the English questionnaire.
The exclusion criteria were patients with type 1 diabetes mellitus, with history of severe hypertension (HTN >160 mmHg); those clinically diagnosed with Bipolar disorders, Schizophrenia, Dementia, Anxiety Disorder, Mental retardation as reported by their attending physician; Drug or Alcohol addicts; Patients who had major life events like death of a loved one and job lost; and having diabetic ketoacidosis.
A letter of invitation to participate was disseminated to endocrinology consultants, endocrinology fellows and internal medicine residents of St. Luke’s Medical Center Quezon City. The attending physicians referred their patients to the investigator who passed the inclusion criteria of the study. Informed consent was obtained prior to collection of data.
The 30-minute interview and examination were conducted at a room at the Diabetes, Thyroid and Endocrine Center of St. Luke’s Medical Center-Quezon City to ensure privacy. Data on socio-demographic characteristics (age, gender, civil status, education, and occupation), diabetes history (duration, insulin therapy, chronic complications, glycemic control as HbA1c on the past 3 months), number of concomitant medication, BMI (body mass index — kg/m2), previous episodes of depression, treatment with antidepressant drugs and family history of depression were collected.
The questionnaires were administered by the primary investigator trained by a psychiatrist. The participants were provided 2 questionnaires. Depressive symptoms were assessed with Patient Health Questionnaire-9 (PHQ- 9). It is a screening tool which incorporates diagnostic criteria with other leading major depressive symptoms into a brief self-report tool. The tool rates the frequency of the symptoms which factors into the scoring severity index. The total score can range from 0 to 27, with higher scores indicating greater severity of depression. A score of 0-4 is none to minimal depression requiring no treatment. A score of more than or equal to 5 makes a diagnosis of depression. A score of 5-9 is mild, 10- 14 is moderate, 15-19 is moderately severe and 20-27 is severe depression, all requiring treatment. PHQ scores of more than 10 had sensitivity of 88% and specificity of 88% for major depression.[8] Compliance to diabetes medications were assessed with the eight-item version of the Morisky Medication Adherence Scale (MMAS).[9] The questionnaires have been validated among Filipinos.[10] These were interpreted by a psychiatrist. The results were then forwarded to the attending physicians and psychiatric consult were discussed.
Description of outcome measures
The primary outcome of the study was the prevalence rate of depression among patients diagnosed with Type 2 Diabetes Mellitus using the PHQ-9.
Secondary outcomes determined the severity of depression, medication adherence and association of BMI, duration of diabetes, compliance with medications, type of medications (OADs versus insulin therapy), number of medications (single or multiple drug therapy) socioeconomic status and other comorbid diseases (hypertension, dyslipidemia, ischemic heart disease) with depression.
Sample size estimation
Minimum needed sample size for logistic regression analysis was computed using G*power 3.0.10 software.11 Based on expected medium effect size (r2 =15%), 95% confidence interval, 90% power, and 20 independent variables (sociodemographic and clinical variables) the minimum needed sample size was 191.
Data analysis
The socio-demographic and clinical characteristics were summarized using means and standard deviations for continuous data and frequencies and percentages for categorical data. Pearson chi-square and Fisher’s exact tests were used to determine if the distribution of levels of depression significantly differed per category of each variable. Multiple logistic regression analysis was used to evaluate the relationship between different variables and presence of depression among patients with type 2 diabetes mellitus. P-values less than 0.05 was used and confidence level was set at 95%. All variables that have p-value<0.10 during univariate tests of association were included in the multiple logistic regression analysis. STATA 14 was used for data analysis.
Ethical considerations
The Clinical Protocol and all relevant documents were reviewed and approved by the SLMC Institutional Ethics Review Committee. Upon the referral from the attending physicians, the significance of study was explained and an informed consent was sought by the primary investigator. Patient’s autonomy and confidentiality were respected. Data were coded and identification anonymized. All data were recorded and investigators were responsible for the integrity of the data i.e., accuracy, completeness, legibility, etc. Results were disseminated to the attending physician with the approval of the patient. The manner of disseminating and communicating the study results guaranteed the protection of the confidentiality of patient’s data. The data will be kept by the investigator until 5 years from the end of the study. Data gathered will be discarded after 5 years.
Table 1 describes the characteristics of the 476 patients included in this study. The mean age was 58.3 (SD=11.8) and majority were female (63.5%). Majority were also married (75.2%) and were college or vocational course graduates (69.1%). Almost half of them were employed (45.6%). The mean BMI of the patients was 26.7 (SD=4.9). More than half of them were also obese (59.7%).
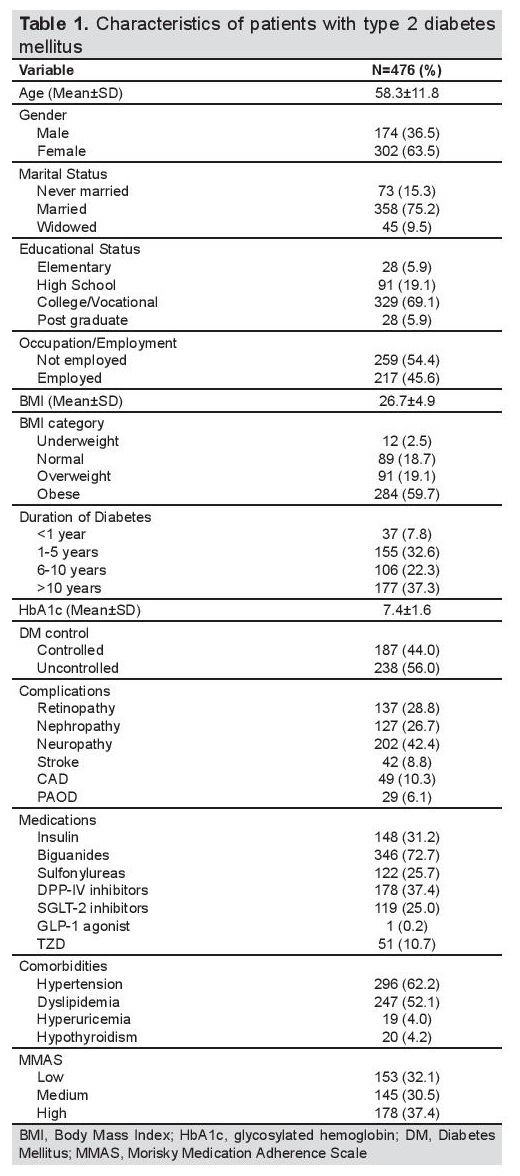
Table 1. Characterstics of patients with type 2 diabetes mellitus
In terms diabetes duration, more than half had the disease for more than 5 years already (59.6%). Their mean HbA1c value was 7.4 (SD=1.6) with almost half having uncontrolled diabetes (56.0%). The most prevalent complication experienced by the patients was neuropathy (42.4%) followed by retinopathy (28.8%) and nephropathy (26.7%). The most commonly used medication was a biguanide (72.7%), followed by DPP-IV inhibitors (37.4%), and then insulin (31.2%). In terms of their comorbidities, 62.2% had hypertension and 52.1% had dyslipidemia. It was also observed that only 37.4% had good compliance with regards to their medications.
Table 2 describes the prevalence of depression among the patients with type 2 diabetes mellitus included in the study. The mean PHQ score was 2.6 (SD=3.4). More than half of the patients had none to minimal depression (81.1%). A PHQ score of more than five denotes depression. There was a prevalence of depression of 19.9 %, with mild depression at 12.6%. Moderate depression was reported by 5.0% of the patients and 1.3% had moderately severe depression. None have severe depression.
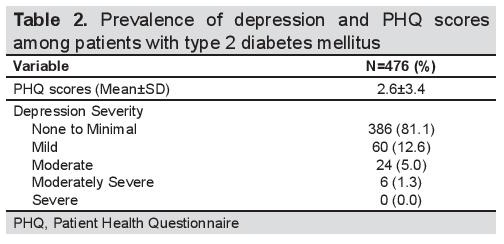
Table 2. Prevalence of depression and PHQ scores among patients with type 2 diabetes mellitus
Table 3 describes the prevalence of depression disaggregated per socioeconomic and clinical characteristics of the patient. Only gender, BMI, DM control, presence of neuropathy as complication, and level of medication adherence, had significant differences in terms of distribution of levels of depression (All p-values<0.05). Females had higher prevalence of mild depression (15.9%) and moderate to moderately severe depression (6.9%) compared to males. The prevalence of none/minimal and mild depression was 77.2% and 17.3% among those with neuropathy. In terms of BMI, moderate to moderately severe depression was highest among those with normal BMI (25.0%) and lowest among obese (4.2%). In terms of DM control, the prevalence of none/minimal (85.3%) depression was higher among those with controlled DM and the prevalence of moderate to moderately severe was higher among those with uncontrolled DM (7.5%). In terms of medication adherence, the prevalence of none/minimal (90.4%) depression was highest among those with high adherence and the prevalence of moderate to moderately severe was highest among those with low adherence (10.5%).
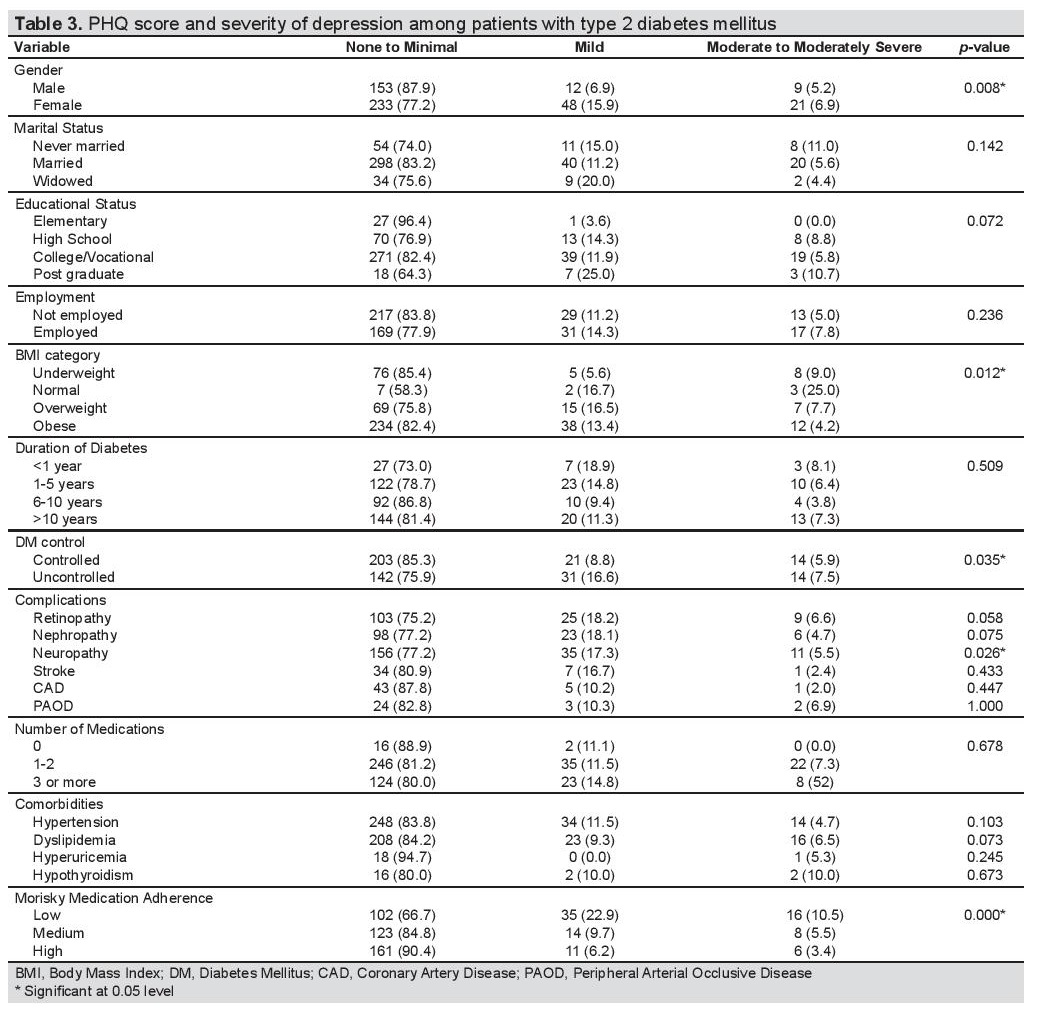
Table 3. PHQ score and severity of depression among patients with type 2 diabetes mellitus
Table 4 shows that results of the univariate logistic regression analysis on the association of socioeconomic status and clinical factors with depression among patients with type 2 diabetes mellitus. It can be seen that increasing age (p-value=0.001), hypertension (p-value=0.015), having diabetes for 6-10 years (p-value=0.027) and medium/high medication adherence (p-value=0.005 and 0.000, respectively) were significantly associated with decreased odds for depression. On the other hand, being female (p-value=0.012), having a post-graduate degree (p-value=0.020), being underweight (p-value=0.022), higher HbA1c (p-value=0.002), uncontrolled diabetes (p-value=0.017), presence of retinopathy (p-value=0.026), and higher MMA Score (lower adherence) (p-value=0.000) were significantly associated with increased odds for depression.
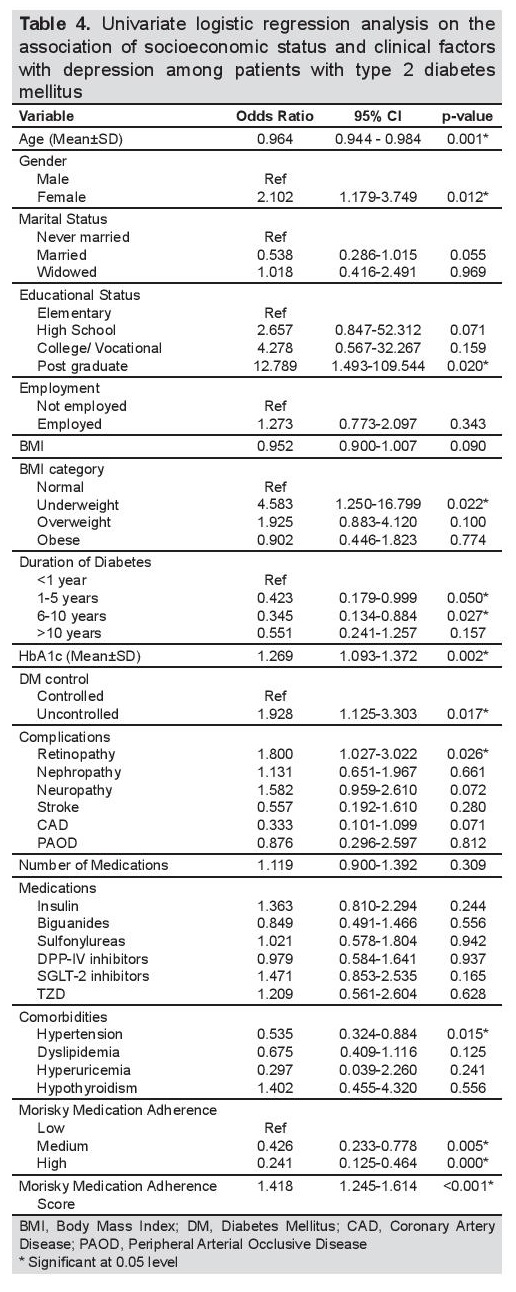
Table 4. Univariate logistic regression analysis on the association of socioeconomic status and clinical factors with depression among patients with type 2 diabetes mellitus
Table 5 shows that results of the multiple logistic regression analysis on the association of socioeconomic status and clinical factors with depression among patients with type 2 diabetes mellitus (R2 value=21.20). It can be seen that increasing age (p-value=0.021) and chronic duration of diabetes (6-10 years) (0.033) were significantly associated with decreased odds for depression. On the other hand, having a post-graduate degree (p-value=0.012), presence of retinopathy (p-value=0.018), and higher MMA Score (lower adherence) (p-value=0.000) were significantly associated with increased odds for depression.
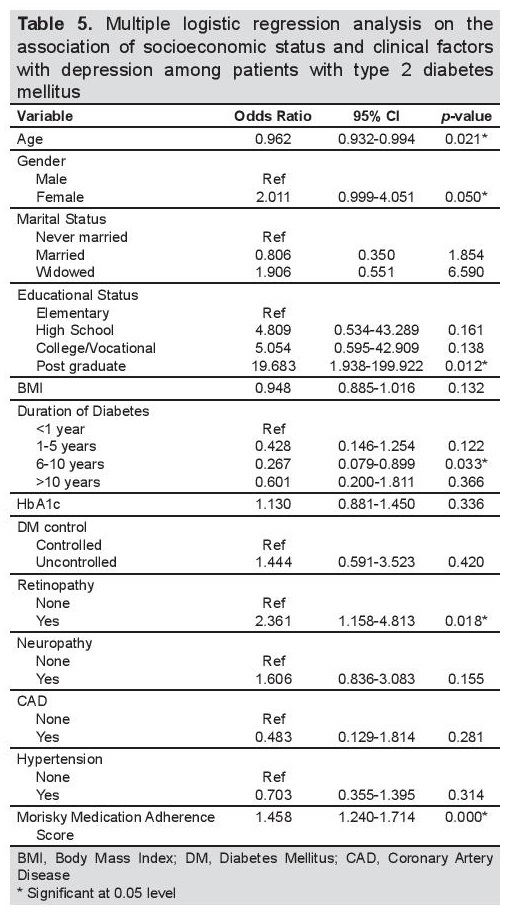
Table 5. Multiple logistic regression analysis on the association of socioeconomic status and clinical factors with depression among patients with type 2 diabetes mellitus
In a survey conducted by Perlas, Tronco et al., in the Philippines, about 5.3 percent of Filipinos with chronic illness were suffering from depression.[12] In the study of Dy Nieva et al., 31% of patients with type 2 diabetes mellitus had depression, with 24% as mild, and 7% had moderate depression.[13] In our study, the prevalence of depression among patients with diabetes mellitus in the Philippines was lower at 18.2%, with mild depression at 13% and moderate depression at 5.2%. Unlike the study of Dy Nieva et al.,[13] our sample size was larger.
The prevalence result of our study was lower than Varma et al. (49.48%),[14]Al Ghamdi (34%),[15] Sweileh et al. (40%),[16] Salinero- Fort et al. (20.03 %),[17] and Rodriguez Calvin (32.7),18 but higher than the study of Zhang in China (5.7%).[5]
The prevalence of moderate to severe depression in our study was 6.3%. This was lower in comparison with the Mexican American population which 25% presented with minor depression and 9% with lifetime diagnosis of major depressive disorder.[6] In the study of Varma et al., in India, their prevalence of depression in patients with Type 2 diabetes mellitus was 49.5%, with those having severe depression at 7.16%.[14]
Inconsistent with other studies, female gender did not increase the risk of depression.[14],[16]-[17] Being single, including being unmarried, widowed, and divorced, was identified as a risk factor according to the study of Zhang,[5] however, in our study the marital status was not a significant factor. Having higher educational degree, increases depression, which were in contrast with the results of the other studies.[16]
Different from other studies,[5],[14] the number of medications and type of medication, whether oral antidiabetic medications or insulin, did not increase the risk of depression. Furthermore, in contrast with the study of Zhang,[5] Sweileh[16] and Dy Nieva,[13] which revealed higher BMI had association with depression, weight was not a factor for depression in our study.
Diabetic complications were found to be strongly associated with increasing depression.[6],[14] Other studies showed depression was associated with neuropathy[17] but in our study, retinopathy was the connected complication.
Blurring of vision or visual abnormalities are noticeable symptoms which may add to the stress of the patient and affect their activities of daily living.
As seen with the study of Sweileh et al.,[16] low medication adherence revealed to be associated with depression. Patients with poor glycemic control have greater risk of experiencing depression than those who have good control as seen in our study. Several studies have confirmed this association.[14],[18] When T2DM and depression co-exist in an individual, he/she is more prone to develop worse glycemic control due to poorer medication adherence, which could lead to diabetic complications and associated morbidity.
Based from other reviews, there is a biological basis of depression and type 2 diabetes mellitus. Depression is associated with subclinical hypercortisolism secondary to hypothalamic-pituitary adrenal (HPA) axis activation.[19]-[20] Cortisol also activates lipolysis and release of free fatty acids, which can induce insulin resistance. Repeated stress with the repeated induction of corticosteroids can result in hippocampal damage, causing a failure in the downregulation of corticosteroid production by the feedback mechanism and thus persisting elevated circulating cortisol levels.[21],[22] In the study of Gold et al., individuals with type 2 diabetes have clear deficits in hippocampal-based (recent or declarative) memory and selective MRI-based atrophy of the hippocampus relative to matched control subjects.[23] These may provide an additional explanatory link between depression and type 2 diabetes.
Metabolic disturbances of diabetes also lead to changes in the brain that alter susceptibility to social stressors. It induces changes in neuronal function and structure on areas of the brain that regulate affect and, therefore, increase risk for depression.[24]
It was also noted that inflammation is also present on both diabetes mellitus and depression. A study by Brummett et al.,[25] found depression to be associated with higher inflammatory markers (CRP and IL-6), and interestingly the association was stronger in women compared with men. Both depression and diabetes are associated with enhanced cytokine production and elevation of inflammatory markers which may be another biological mechanism through which these two disorders are related.[19],[22] Catecholamines and inflammatory cytokines are known to induce insulin resistance.[19],[26] Features of type 2 diabetes, such as fatigue, sleep disturbance, and depression, are likely to be at least partly due to hypercytokinemia and activated innate immunity.[21]
It is beyond the scope of the study to investigate further the biological basis of depression among diabetes mellitus. In this study, the associated clinical risk factors for depression were: being employed, having low medication adherence and poorly controlled diabetes mellitus and, the presence of retinopathy.
Limitations of the study
Our study investigated the prevalence and associated factors of depression in patients with type 2 diabetes mellitus in the Philippines. However, our study has few limitations: (1) consecutive sampling was done to recruit participants, (2) samples were recruited from 1 hospital only and are not representative of the subsets of patients in the Philippines, (3) complications of diabetes were noted per chart review and as reported by the subjects only, (4) this study is cross-sectional where causal relationship between diabetes and depression cannot be established.
Depression is prevalent among Filipino patients with Type 2 Diabetes Mellitus. About two out of five patients (19.9%) with diabetes mellitus have depression. Low medication adherence, having a postgraduate degree and presence of retinopathy as complication, were significantly associated with depression. These findings support a recommendation for routine screening and regular psychosocial assessment for depression among Filipino patients with diabetes. Integrated approach by the attending physicians and psychiatrists may be required for the effective management of these patients. Statement of Authorship
All authors certified fulfillment of ICMJE authorship criteria.
Author DisclosureThe authors declared no conflict of interest
Funding SourcePSEDM-Servier Research Grant in Diabetes Year 2018 aided in funding this study.
[1] Shera AS, Jawad F. Basil A. Diabetes related knowledge, attitude
and practices of family physicians in Pakistan. J Pak Med Assoc.
2002;52(10):465-70.
[2] Tovilla-Zárate C, Juárez-Rojop I, Peralta Jimenez Y, et al. Prevalence
of anxiety and depression among outpatients with type 2 diabetes in
the Mexican population. PloS One. 2012;7(5):e36887.
[3] Bartoli F, Carrà G, Crocamo C., et al. Association between depression
and neuropathy in people with type 2 diabetes: A meta‐analysis. Int
J Geriatr Psychiatry. 2016;31(8):829-36.
[4] Al-Amer RM, Sobeh MM, Zayed AA, Al-Domi HA. Depression among
adults with diabetes in Jordan: Risk factors and relationship to blood
sugar control. J Diabetes Complications. 2011;25(4):247-52.
[5] Zhang W, Xu H, Zhao S, et al. Prevalence and influencing factors
of co-morbid depression in patients with type 2 diabetes mellitus:
A general hospital based study. Diabetol Metab Syndr. 2015;7:60.
[6] Black SA, Markides KS, Ray LA. Depression predicts increased
incidence of adverse health outcomes in older Mexican Americans
with type 2 diabetes. Diabetes Care. 2003;26(10):2822-8.
[7] Engum A, Mykletun A, Midthjell K, Holen A, Dahl AA. Depression
and diabetes: A large population-based study of sociodemographic,
lifestyle, and clinical factors associated with depression in type 1 and
type 2 diabetes. Diabetes Care. 2005;28(8):1904-9.
[8] Kroenke K, Spitzer RL, Williams JB. The PHQ‐9: validity of a brief
depression severity measure. J Gen Intern Med. 2001;16(9):606-13.
[9] Moon SJ, Lee WY, Hwang JS, Hong YP, Morisky DE. Accuracy of a
screening tool for medication adherence: A systematic review and
meta-analysis of the Morisky Medication Adherence Scale-8. PloS
One. 2017;12(11):e0187139.
[10] Garabiles MR, Lao CK, Yip P, Chan EWW, Mordeno I, Hall BJ.
Psychometric validation of PHQ–9 and GAD–7 in Filipino migrant
domestic workers in Macao (SAR), China. J Pers Assess. 2019:30:1-12.
[11] Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible
statistical power analysis program for the social, behavioral,
and biomedical sciences. Behav Res Methods. 2007;39(2):175-91.
[12] Perlas AP, Briones-Querijero MM, Abcede D, et al. The prevalence
of psychiatric disorders among the chronically-ill medical patients
in selected tertiary hospitals in the Philippines. Philipp J Psychiatry.
2004;28:17-24. PCHRDPC050267
[13] Nieva SJD, Capellan MLD, Montano CN. Prevalence and risk factors
for depression among Filipino adults with diabetes mellitus type 2 at
the Makati Medical Center Outpatient Department. Philipp J Int Med.
2017;55(2):1-10.
[14] Varma P, Kant R. Mishra PP. Depression in type 2 diabetes
mellitus: A cross-sectional study in tertiary teaching hospital in India.
J Diab Endocrinol Assoc Nepal. 2018;2(1):24-8.
[15] Al-Ghandi AA. A high prevalence of depression among
diabetic patients at a teaching hospital in Western Saudi Arabia.
Neurosciences (Riyadh). 2004;9(2):108-12.
[16] Sweileh WM, Abu-Hadeed HM, Al-Jabi SW, Zyoud SH. Prevalence
of depression among people with type 2 diabetes mellitus: A crosssectional
study in Palestine. BMC Public Health. 2014;14(1):163.
[17] Salinero-Fort MA, Gómez-Campelo P, San Andrés-Rebollo FJ, et al.
Prevalence of depression in patients with type 2 diabetes mellitus
in Spain (the DIADEMA Study): Results from the MADIABETES
cohort. BMJ Open. 2018;8(9): e020768.
[18] Calvín JLR, Gaviria AZ, Ríos MM. Prevalence of depression in
type 2 diabetes mellitus 2. Revista Clínica Española (English ed).
2015;215(3):156-64.
[19] Champaneri S, Wand GS, Malhotra SS, Casagrande SS, Golden SH.
Biological basis of depression in adults with diabetes. Curr Diab Rep.
2010;10(6):396-405.
[20]Sadeghi A, Hami J, Razavi S, Esfandiary E, Hejazi Z. The effect
of diabetes mellitus on apoptosis in hippocampus: Cellular and
molecular aspects. Int J Prev Med. 2016;7:57.
[21] Pickup JC. Inflammation and activated innate immunity in the
pathogenesis of type 2 diabetes. Diabetes Care. 2004;27(3):813-23.
[22] Laake JP, Stahl D, Amiel SA, et al. The association between depressive
symptoms and systemic inflammation in people with type 2 diabetes:
Findings from the South London Diabetes Study. Diabetes Care.
2014;37(8):2186-92.
[23] Gold SM, Dziobek I, Sweat V, et al. Hippocampal damage and
memory impairments as possible early brain complications of type 2
diabetes. Diabetologia. 2007;50(4):711-9.
[24] Jacobson AM, Samson JA, Weinger K, Ryan CM. Diabetes, the
brain, and behavior: Is there a biological mechanism underlying the
association between diabetes and depression? Int Rev Neurobiol.
2002;51:455-79.
[25] Brummett BH, Boyle SH, Ortel TL, Becker RC, Siegler IC, Williams
RB. Associations of depressive symptoms, trait hostility, and gender
with C-reactive protein and interleukin-6 response following emotion
recall. Psychosom Med. 2010;72(4):333-9.
[26] Moulton CD, Pickup JC, Ismail K. The link between depression
and diabetes: The search for shared mechanisms. Lancet Diabetes
Endocrinol. 2015;3(6):461-71.
Authors are required to accomplish, sign and submit scanned copies of the JAFES Author Form consisting of: (1) Authorship Certification, that all the requirements for authorship have been met by each author, and that the final version of the manuscript has been read and approved by all authors; (2) the Author Declaration, that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere; (3) the Statement of Copyright Transfer [accepted manuscripts become the permanent property of the JAFES and are licensed with an Attribution-Share Alike-Non-Commercial Creative Commons License. Articles may be shared and adapted for non-commercial purposes as long as they are properly cited]; and the ICMJE form for Disclosure of Potential Conflicts of Interest. For original articles, authors are required to submit a scanned copy of the Ethics Review Approval of their research as well as registration in trial registries as appropriate. For manuscripts reporting data from studies involving animals, authors are required to submit a scanned copy of the Institutional Animal Care and Use Committee approval. For Case Reports or Series, and Images in Endocrinology, consent forms, are required for the publication of information about patients; otherwise, appropriate ethical clearance has been obtained from the institutional review board. Articles and any other material published in the JAFES represent the work of the author(s) and should not be construed to reflect the opinions of the Editors or the Publisher.