Association between Degrees of Malnutrition and Clinical Outcomes among Non-critically Ill Hospitalized Adult Patients with Type 2 Diabetes Mellitus
DOI:
https://doi.org/10.15605/jafes.036.02.12Keywords:
malnutrition, hospital outcome, diabetes mellitusAbstract
Introduction. Malnutrition among hospitalized patients is highly prevalent. This adversely affects outcomes with longer length of stay (LOS), higher treatment costs and increased mortality. People with diabetes mellitus (DM) are particularly vulnerable to malnutrition and its consequences.
Objective. To determine the association of nutritional status with LOS and mortality among adults with Type 2 DM.
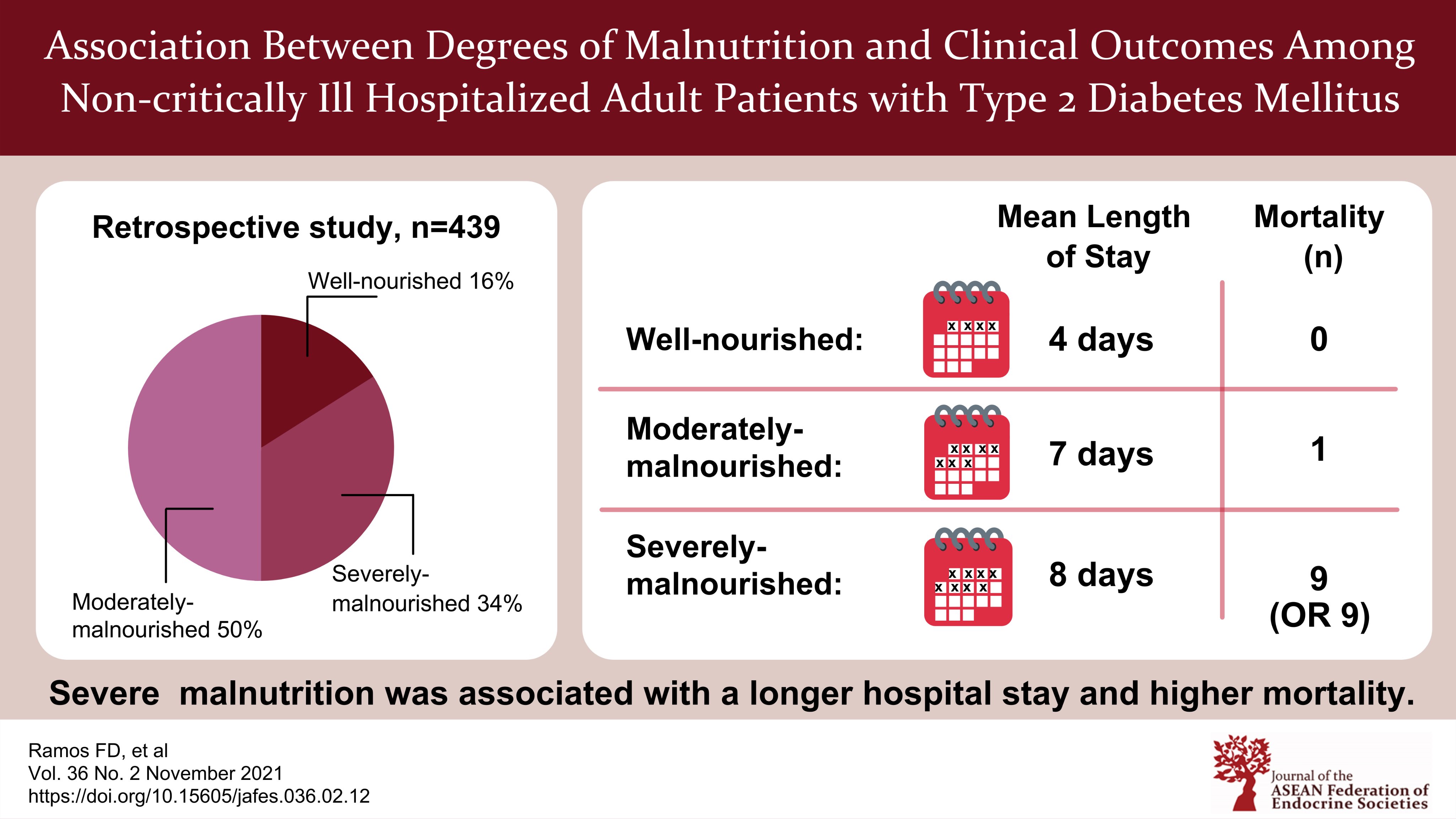
Methodology. This was a retrospective study of 439 adult patients with type 2 diabetes admitted in the medical ward of a tertiary hospital from January 1, 2018 to December 31, 2018. Demographics, anthropometrics, feeding route, LOS and outcomes were taken from the Clinical Nutrition Service database; biochemical data were taken from the Healthcare System, and were analyzed.
Results. In our analysis, 83.8% were found to be malnourished with 50.3% moderately-malnourished (MM) (Nutrition risk level 1-2) and 33.5% severely-malnourished (SM) (Nutrition risk level ³3). BMI category and malnutrition were the significant confounders for LOS. After controlling for BMI, LOS was longer by a mean of 2.2 days in SM compared to well-nourished (WN) patients (95% CI=0.49-3.95, p=0.012). Of the malnourished patients, 6.1% of SM and 0.5% of MM patients died. None of the WN patients died. Feeding route, admitted for neoplasm, low albumin levels and malnutrition were the confounding factors associated with mortality. After controlling for these factors, SM had higher odds of dying compared to MM patients [adjusted OR=8.91 (95% CI=1.04-76.18, p=0.046)].
Conclusion. Among hospitalized non-critically ill adult patients with type 2 diabetes, SM patients but not MM patients had significantly longer LOS compared to WN patients, and greater degrees of malnutrition were associated with higher mortality.
Downloads
References
World Health Organization. Fact sheets. Malnutrition. https://www.who.int/news-room/fact-sheets/detail/malnutrition.
Cederholm T, Barazzoni R, Austin P, et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr. 2017;36(1):49-64. https://pubmed.ncbi.nlm.nih.gov/27642056. https://doi.org/10.1016/j.clnu.2016.09.004.
Tappenden KA, Quatrara B, Parkhurst ML, Malone AM, Fanjiang G, Ziegler TR. Critical role of nutrition in improving quality of care: An interdisciplinary call to action to address adult hospital malnutrition. J Acad Nutr Diet. 2013;113(9):1219-37. https://pubmed.ncbi.nlm.nih.gov/23871528. https://doi.org/10.1016/j.jand.2013.05.015.
Mc Whirter JP, Pennington CR. Incidence and recognition of malnutrition in hospital. Br Med J. 1994;308(6934):945-8. https://pubmed.ncbi.nlm.nih.gov/8173401. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2539799. https://doi.org/10.1136/bmj.308.6934.945.
Baccaro F, Moreno JB, Borlenghi C, et al. Subjective global assessment in the clinical setting. JPEN J Parenteral Enteral Nutr. 2007;31(5):406-9. https://pubmed.ncbi.nlm.nih.gov/17712149. https://doi.org/10.1177/0148607107031005406.
Hospital Malnutrition and Clinical Nutrition Program Task Force, Metro Manila, Philippines. The value of implementing a clinical nutrition program and nutrition support team (NST) to address the problem of malnutrition in the hospitals of the Philippines. PhilSPEN Online Journal of Parenteral and Enteral Nutrition. Jan 2010 – Jan 2012:Article 5(POJ_0017):42-54. http://www.philspenonlinejournal.com/POJ_0017.html.
Cabangon MR, Narvacan-Montano C, del Rosario-Capellan ML, Campos-Cagingin ML. Prevalence of malnutrition among patients with diabetes mellitus type 2 admitted in a tertiary hospital. Philipp J Intern Med. 2016;54(2):1-11. https://drive.google.com/file/d/1InkHyJj70wc1P_ouCS72FPDPNrUTYI2R/view.
Barker LA, Gout BS, Crowe TC. Hospital malnutrition: Prevalence, identification and impact on patients and the healthcare system. Int J Environ Res Public Health. 2011;8(2):514-27. https://pubmed.ncbi.nlm.nih.gov/21556200. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3084475. https://doi.org/10.3390/ijerph8020514.
Dominguez RJ. Burden of malnutrition in a tertiary care hospital in Baguio City. SAGE Pub. 2013:1–7. https://doi.org/10.1177/2158244013504936.
Alberda C, Gramlich L, Jones N, at al. The relationship between nutritional intake and clinical outcomes in critically ill patients: Results of an international multicenter observational study. Intensive Care Med. 2009;35(10):1728-37. https://pubmed.ncbi.nlm.nih.gov/19572118. https://doi.org/10.1007/s00134-009-1567-4.
Favaro-Moreira NC, Krausch-Hofmann S, Matthys C, et al. Risk factors for malnutrition in older adults: A systematic review of the literature based on longitudinal data. Adv Nutr 2016;7(3):507–22. https://pubmed.ncbi.nlm.nih.gov/27184278. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4863272. https://doi.org/10.3945/an.115.011254.
Avelino-Silva TJ, Jaluul O. Malnutrition in hospitalized older patients: Management strategies to improve patient care and clinical outcomes. Int J Gerontol. 2017;11(2):56-61. https://reader.elsevier.com/reader/sd/pii/S1873959817301461?token=9B6206B33C4F64B3021175C7BD4102AB18C5E0C81B2E5555294A3CA4499D6FA141E666BE650C194DDD6687E0CEC6FF12&originRegion=eu-west-1&originCreation=20210815062934.
Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: An independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 87(3):978–82. https://pubmed.ncbi.nlm.nih.gov/11889147. https://doi.org/10.1210/jcem.87.3.8341.
Evans DC, Corkins MR, Malone A, et al. The use of visceral proteins as nutrition markers: An ASPEN position paper. Nutr Clin Pract. 2021;36(1):22–8. https://pubmed.ncbi.nlm.nih.gov/33125793. https://doi.org/10.1002/ncp.10588.
Demling RH. Nutrition, anabolism, and wound healing process: An overview. Eplasty. 2009;9:e9. https://pubmed.ncbi.nlm.nih.gov/19274069. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2642618.
Kuzuya M, Kanda S, Koike T, Suzuki Y, Iguchi A. Lack of correlation between total lymphocyte count and nutritional status in the elderly. Clin Nutr. 2005;24(3):427-32. https://pubmed.ncbi.nlm.nih.gov/15896430. https://doi.org/10.1016/j.clnu.2005.01.003.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2007;30(Suppl 1):S42-7. https://pubmed.ncbi.nlm.nih.gov/17192378. https://doi.org/10.2337/dc07-S042.
Al-Goblan AS, Al-Alfi MA, Khan MZ. Mechanism linking diabetes mellitus and obesity. Diabetes Metab Syndr Obes. 2014;7:587–91. https://pubmed.ncbi.nlm.nih.gov/25506234. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4259868. https://doi.org/10.2147/DMSO.S67400.
Published
How to Cite
Issue
Section
License
Copyright (c) 2021 Freyja Diana Ramos, Joy Arabelle Fontanilla, Reginna Emiliene Lat

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The full license is at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.










