Rare Case of Large Catecholamine Secreting Ganglioneuroma in an Asymptomatic Elderly
DOI:
https://doi.org/10.15605/jafes.037.01.10Keywords:
adrenal glands, catecholamine, ganglioneuromaAbstract
Ganglioneuromas (GNs) are benign tumors that originate from neural crest cells, composed mainly of mature ganglion cells. These tumors, which are usually hormonally silent, tend to be discovered incidentally on imaging tests and occur along the paravertebral sympathetic chain, from the neck to the pelvis and occasionally in the adrenal medulla. Rarely, GNs secrete catecholamines.1 Adrenal GNs occur most frequently in the fourth and fifth decades of life, whereas GNs of the retroperitoneum and posterior mediastinum are usually encountered in younger adults.2 Adrenal GNs are commonly hormonally silent and asymptomatic; even when the lesion is of substantial size.3
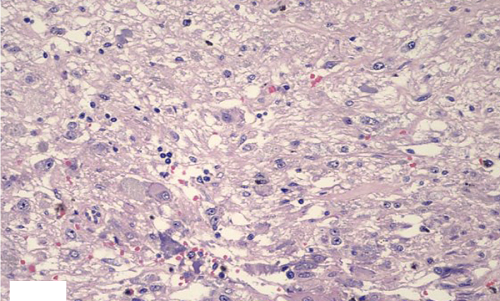
We report an incidentally detected asymptomatic case of an adrenal ganglioneuroma with mildly elevated urinary catecholamine levels in an elderly male. After preoperative alpha blockade, the patient underwent open right adrenalectomy. Upon microscopic examination, the right adrenal mass proved to be a ganglioneuroma, maturing type and the immunohistochemistry examination showed immunoreactivity to synaptophysin, chromogranin, and CD 56, while S100 was strongly positive at the Schwannian stroma. Following resection, catecholamine levels normalized, confirming the resected right adrenal ganglioneuroma as the source of the catecholamine excess. This case represents a rare presentation of catecholamine-secreting adrenal ganglioneuroma in the elderly.
Downloads
References
Chan OTM, Haghighi P. Hamartomatous polyps of the colon: Ganglioneuromas, stromal, and lipomatomous. Arch Pathol Lab Med. 2006;130(10):1561–6. https://pubmed.ncbi.nlm.nih.gov/17090203. https://doi.org/10.5858/2006-130-1561-HPOTCG.
Qing Y, Bin X, Jian W, et al. Adrenal ganglioneuromas: A 10-year experience in a Chinese population. Surgery. 2010;147(6):854–60. https://pubmed.ncbi.nlm.nih.gov/20060552. https://doi.org/10.1016/j.surg.2009.11.010.
Allende DS, Hansel DE, MacLennan GT. Ganglioneuroma of the adrenal gland. J Urol. 2009;182(2):714–5. https://pubmed.ncbi.nlm.nih.gov/9539319. https://doi.org/10.1016/j.juro.2009.05.036.
Graham-Pole J, Salmi T, Anton AH, Abramowsky C, Gross S. Tumor and urine catecholamines (CATs) in neurogenic tumors. Correlations with other prognostic factors and survival. Cancer. 1983;51(5):834-9. https://pubmed.ncbi.nlm.nih.gov/6821849.
Rha SE, Byun JY, Jung SE, et al. Neurogenic tumors in the abdomen: Tumor types and imaging characteristics. Radiographics 2003;23(1):29-43. https://pubmed.ncbi.nlm.nih.gov/12533638. https://doi.org/10.1148/rg.231025050.
Jaulim A, Nkwam N, Williams S. Mature ganglioneuroma of the adrenal gland as a new rare cause of visible haematuria: A case report & literature review. Int J Surg Case Rep. 2015;14:1-3. https://pubmed.ncbi.nlm.nih.gov/26196309. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4573211. https://doi.org/10.1016/j.ijscr.2015.06.027.
Lonergan GJ, Schwab CM, Suarez ES, Carlson CL. Neuroblastoma, ganglioneuroblastoma, and ganglioneuroma: Radiologic-pathologic correlation. Radiographics. 2002;22(4):911-34. https://pubmed.ncbi.nlm.nih.gov/12110723. https://doi.org/10.1148/radiographics.22.4.g02jl15911.
Camelo M, Aponte LF, Lugo-Vicente H. Dopamine-secreting adrenal ganglioneuroma in a child: Beware of intraoperative rebound hypertension. J Pediatr Surg. 2012;47(9):E29–32. https://pubmed.ncbi.nlm.nih.gov/22974632. https://doi.org/10.1016/j.jpedsurg.2012.04.017.
Koch CA, Brouwers FM, Rosenblatt K, et al. Adrenal ganglioneuroma in a patient presenting with severe hypertension and diarrhea. Endocr Relat Cancer. 2003;10(1):99–107. https://pubmed.ncbi.nlm.nih.gov/12653673. https://doi.org/10.1677/erc.0.0100099.
Geoerger B, Hero B, Harms D, Grebe J, Scheidhauer K, Berthold F. Metabolic activity and clinical features of primary ganglioneuromas. Cancer. 2001;91(10):1905–13. https://pubmed.ncbi.nlm.nih.gov/11346873.
Weston JA. The migration and differentiation of neural crest cells. Adv Morphog. 1970;8:41–114. https://pubmed.ncbi.nlm.nih.gov/4906187. https://doi.org/10.1016/b978-0-12-028608-9.50006-5.
Mahajan H, Lee D, Sharma R, et al. Composite phaeochromocytoma-ganglioneuroma, an uncommon entity: Report of two cases. Pathology. 2010, 42(3):295-8. https://pubmed.ncbi.nlm.nih.gov/20350228. https://doi.org/10.3109/00313021003636451.
Published
How to Cite
Issue
Section
License
The full license is at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.










