An Atypical Presentation of Primary Hyperparathyroidism With Multiple Spontaneous Tendon Ruptures
A Case Report and Literature Review on the Management of Primary Hyperparathyroidism
DOI:
https://doi.org/10.15605/jafes.037.02.11Keywords:
primary hyperparathyroidism, hypercalcemia, tendon ruptureAbstract
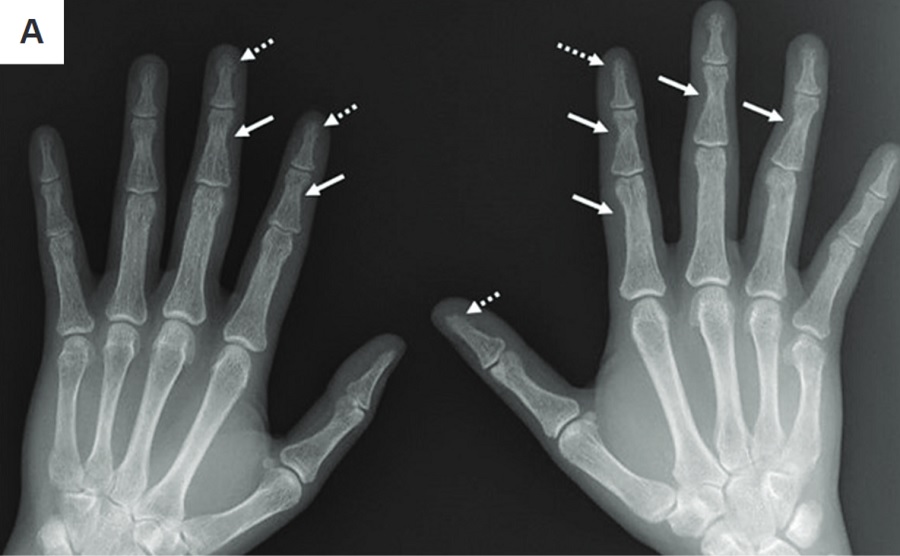
Primary hyperparathyroidism (PHPT) is a common endocrine condition, increasingly presenting asymptomatically and detected on routine laboratory examination in developed countries. Multiple spontaneous tendon ruptures as the initial presentation of PHPT is extremely rare. We present the case of a 28-year-old male diagnosed with severe hypercalcemia secondary to PHPT after presenting with complications of multiple spontaneous tendon ruptures,and discuss the management issues in PHPT for this patient.
Downloads
References
Yeh MW, Ituarte PHG, Zhou HC, et al. Incidence and prevalence of primary hyperparathyroidism in a racially mixed population. J Clin Endocrinol Metab. 2013;98(3):1122-9. https://pubmed.ncbi.nlm.nih.gov/23418315. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3590475. https://doi.org/10.1210/jc.2012-4022.
Silverberg SJ, Bilezikian JP. Evaluation and management of primary hyperparathyroidism. J Clin Endocrinol Metab. 1996;81(6):2036-40. https://pubmed.ncbi.nlm.nih.gov/8964825. https://doi.org/10.1210/jcem.81.6.8964825.
Gao X, Shao Z, Liu S, Xiang J. A case report of spontaneous rupture of the quadriceps tendon. Clin Case Rep. 2017;5(9):1477-81. https://pubmed.ncbi.nlm.nih.gov/28878908. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5582234. https://doi.org/10.1002/ccr3.786.
Yener S, Saklamaz A, Demir T, et al. Primary hyperparathyroidism due to atypical parathyroid adenoma presenting with peroneus brevis tendon rupture. J Endocrinol Invest. 2007;30(5):442-4. https://pubmed.ncbi.nlm.nih.gov/17598980. https://doi.org/10.1007/BF03346325.
Chen CH, Niu CC, Yang WE, Chen WJ, Shih CH. Spontaneous bilateral patellar tendon rupture in primary hyperparathyroidism. Orthopedics. 1999;22(12):1177-9. https://pubmed.ncbi.nlm.nih.gov/10604812. https://doi.org/10.3928/0147-7447-19991201-12.
Lavalle C, Aparicio LA, Moreno J, Chavez de los Rios J, Robles-Paramo A, Fraga A. Bilateral avulsion of quadriceps tendons in primary hyperparathyroidism. J Rheumatol. 1985;12(3):596-8. https://pubmed.ncbi.nlm.nih.gov/4045859.
Camarda L, D’Arienzo A, Morello S, Guarneri M, Balistreri F, D’Arienzo M. Bilateral ruptures of the extensor mechanism of the knee: A systematic review. J Orthop. 2017;14(4):445-53. https://pubmed.ncbi.nlm.nih.gov/28819342. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5548366. https://doi.org/10.1016/j.jor.2017.07.008.
Panagopoulos A, Kalavrytinos D, Giannatos V, Tatani I, Kouzelis A, Kokkalis Z. Early, bilateral re-rupture of quadriceps tendon after previous bone-anchor repair for simultaneous, low-energy, bilateral quadriceps rupture: A case report and literature review. Am J Case Rep. 2021;22:e932723. https://pubmed.ncbi.nlm.nih.gov/34857727. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8653756. https://doi.org/10.12659/AJCR.932723.
Shah MK. Simultaneous bilateral rupture of quadriceps tendons: Analysis of risk factors and associations. South Med J. 2002;95(8):860-6. https://pubmed.ncbi.nlm.nih.gov/12190222.
Thaunat M, Gaudin P, Naret C, Beaufils P, Thaunat O. Role of secondary hyperparathyroidism in spontaneous rupture of the quadriceps tendon complicating chronic renal failure. Rheumatology (Oxford). 2006;45(2):234-5. https://pubmed.ncbi.nlm.nih.gov/16332956. https://doi.org/10.1093/rheumatology/kei022.
Islam AK. Advances in the diagnosis and the management of primary hyperparathyroidism. Ther Adv Chronic Dis. 2021;12:20406223211015965. https://pubmed.ncbi.nlm.nih.gov/34178298. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8202248. https://doi.org/10.1177/20406223211015965.
Ghemigian A, Trandafir AI, Petrova E, et al. Primary hyperparathyroidism-related giant parathyroid adenoma (Review). Exp Ther Med. 2022;23(1):88. https://pubmed.ncbi.nlm.nih.gov/34934453. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8652388. https://doi.org/10.3892/etm.2021.11011.
Chandran M, Bilezikian JP, Salleh NM, et al. Hungry bone syndrome following parathyroidectomy for primary hyperparathyroidism in a developed country in the Asia Pacific. A cohort study. Osteoporos Sarcopenia. 2022;8(1):11-6. https://pubmed.ncbi.nlm.nih.gov/35415277. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8987324. https://doi.org/10.1016/j.afos.2022.03.004.
Silverberg SJ. Vitamin D deficiency and primary hyperparathyroidism. J Bone Miner Res. 2007;22 Suppl 2:V100-4. https://pubmed.ncbi.nlm.nih.gov/18290710. https://doi.org/10.1359/jbmr.07s202.
Eastell R, Brandi ML, Costa AG, D’Amour P, Shoback DM, Thakker RV. Diagnosis of asymptomatic primary hyperparathyroidism: Proceedings of the Fourth International Workshop. J Clin Endocrinol Metab. 2014;99(10):3570-9. https://pubmed.ncbi.nlm.nih.gov/25162666. https://doi.org/10.1210/jc.2014-1414.
Rolighed L, Rejnmark L, Sikjaer T, et al. Vitamin D treatment in primary hyperparathyroidism: A randomized placebo controlled trial. J Clin Endocrinol Metab. 2014;99(3):1072-80. https://pubmed.ncbi.nlm.nih.gov/24423366. https://doi.org/10.1210/jc.2013-3978.
Marcocci C, Bollerslev J, Khan AA, Shoback DM. Medical management of primary hyperparathyroidism: Proceedings of the Fourth International Workshop on the management of asymptomatic primary hyperparathyroidism. J Clin Endocrinol Metab. 2014;99(10):3607-18. https://pubmed.ncbi.nlm.nih.gov/25162668. https://doi.org/10.1210/jc.2014-1417.
Wagner D, Xia Y, Hou R. Safety of vitamin D replacement in patients with primary hyperparathyroidism and concomitant vitamin D deficiency. Endocr Pract. 2013;19(3):420-5. https://pubmed.ncbi.nlm.nih.gov/23337136. https://doi.org/10.4158/EP12155.OR.
Shah VN, Shah CS, Bhadada SK, Sudhakar Rao D. Effect of 25 (OH) D replacements in patients with primary hyperparathyroidism (PHPT) and coexistent vitamin D deficiency on serum 25(OH) D, calcium and PTH levels: A meta-analysis and review of literature. Clin Endocrinol (Oxf). 2014;80(6):797-803. https://pubmed.ncbi.nlm.nih.gov/24382124. https://doi.org/10.1111/cen.12398.
Witteveen JE, van Thiel S, Romijn JA, Hamdy NAT. Hungry bone syndrome: Still a challenge in the post-operative management of primary hyperparathyroidism: A systematic review of the literature. Eur J Endocrinol. 2013;168(3):R45-53. https://pubmed.ncbi.nlm.nih.gov/23152439. https://doi.org/10.1530/EJE-12-0528.
Wilhelm SM, Wang TS, Ruan DT, et al. The American Association of Endocrine Surgeons guidelines for definitive management of primary hyperparathyroidism. JAMA Surg. 2016;151(10):959-68. https://pubmed.ncbi.nlm.nih.gov/27532368. https://doi.org/10.1001/jamasurg.2016.2310.
Parnell KE, Oltmann SC. The surgical management of primary hyperparathyroidism: An updated review. Int J Endocr Oncol. 2018;5(1):IJE07. https://doi.org/10.2217/ije-2017-0019.
Iacobone M, Carnaille B, Palazzo FF, Vriens M. Hereditary hyperparathyroidism—a consensus report of the European Society of Endocrine Surgeons (ESES). Langenbecks Arch Surg. 2015;400(8):867-86. https://pubmed.ncbi.nlm.nih.gov/26450137. https://doi.org/10.1007/s00423-015-1342-7.
Lou I, Balentine C, Clarkson S, Schneider DF, Sippel RS, Chen H. How long should we follow patients after apparently curative parathyroidectomy? Surgery. 2017;161(1):54-61. https://pubmed.ncbi.nlm.nih.gov/27863779. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5164956. https://doi.org/10.1016/j.surg.2016.05.049.
Mallick R, Nicholson KJ, Yip L, Carty SE, McCoy KL. Factors associated with late recurrence after parathyroidectomy for primary hyperparathyroidism. Surgery. 2020;167(1):160-5. https://pubmed.ncbi.nlm.nih.gov/31606193. https://doi.org/10.1016/j.surg.2019.05.076.
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Jielin Yew, Shui Boon Soh

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Journal of the ASEAN Federation of Endocrine Societies is licensed under a Creative Commons Attribution-NonCommercial 4.0 International. (full license at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.









