A Comparison of Statin Treatment Algorithms Based on the ACC/AHA and Philippine Guidelines for Primary Prevention of Dyslipidemia in Statin-Naive Filipino Patients
DOI:
https://doi.org/10.15605/jafes.037.02.16Keywords:
dyslipidemia, hypercholesterolemia, algorithms, statins, primary preventionAbstract
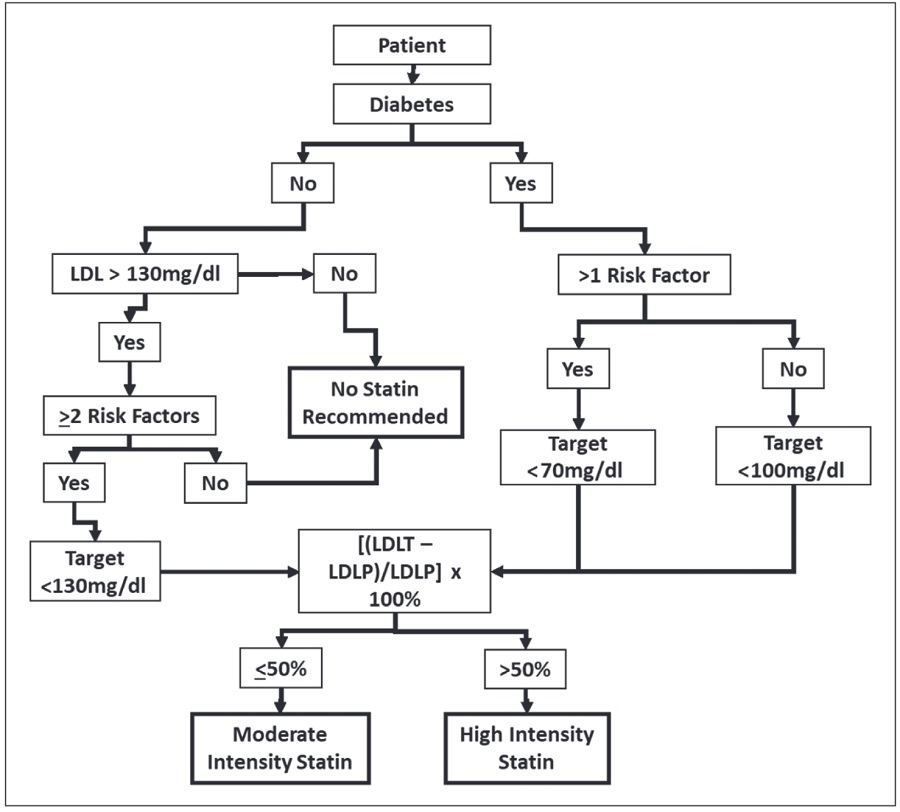
Objectives. This cross-sectional study evaluates the degree of agreement between the 2018 American College of Cardiology/American Heart Association (ACC/AHA2018) and 2020 Philippine guideline (PG2020) treatment algorithms for the primary prevention of dyslipidemia among Filipinos.
Methodology. This review included 159 charts of tatin-naive Filipinos who are 45-79 years old. Using risk profile and lipid measurements, statin treatment recommendation was determined through the PG2020 algorithm and ACC/AHA-ASCVD Risk Estimator Plus web application. The degree of agreement was measured by Cohen’s kappa statistic with the two algorithms as independent raters.
Results. A total of 159 patients were included in the final analysis. There was a slight agreement with a kappa coefficient of 0.209 or 4.4% (95% CI 0.078-0.340, p=0.003). Statin treatment was recommended in 69 out of 159 patients (43.4%) by the PG2020 overlapping with ACC/AHA2018 in 56 cases (81.2%). On the other hand, 109 cases (68.6%) were recommended for statin treatment by ACC/AHA2018 overlapping with PG2020 in only 51.4%.
Conclusions. The low degree of agreement between the two treatment algorithms highlights the key demographic and ethnic variations in dyslipidemia management necessitating outcome-based studies to translate these differences. Overestimation of ASCVD risk calculation in the ACC/AHA2018 and consideration of important, unique risk factors among Filipinos favors the applicability of the Philippine guideline.
Downloads
References
Lee ZV, Llanes EJ, Sukmawan R, et al. Prevalence of plasma lipid disorders with an emphasis on LDL cholesterol in selected countries in the Asia-Pacific region. Lipids Health Dis. 2021;20(1):33. https://pubmed.ncbi.nlm.nih.gov/33858442. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8051043. https://doi.org/10.1186/s12944-021-01450-8.
Lin CF, Chang YH, Chien SC, Lin YH, Yeh HY. Epidemiology of Dyslipidemia in the Asia Pacific Region. Int J Gerontol. 2018;12(1):2-6. doi:10.1016/j.ijge.2018.02.010
Alshamiri M, Ghanaim MMA, Barter P, et al. Expert opinion on the applicability of dyslipidemia guidelines in Asia and the Middle East. Int J Gen Med. 2018;11:313-22. https://pubmed.ncbi.nlm.nih.gov/30050317. https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC6055898. https://doi.org/10.2147/IJGM.S160555.
Gonzalez-Santos LE, Oliva R, Jimeno C, et al. Executive summary of the 2020 Clinical Practice Guidelines for the management of dyslipidemia in the Philippines. J ASEAN Fed Endocr Soc. 2021;36(1):5-11. https://pubmed.ncbi.nlm.nih.gov/34177082. https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC8214350. https://doi.org/10.15605/jafes.036.01.01.
Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73(24):3168-209. https://pubmed.ncbi.nlm.nih.gov/30423391. https://doi.org/10.1016/J.JACC.2018.11.002.
Bujang MA, Baharum N. Guidelines of the minimum sample size requirements for Cohen’s Kappa. Epidemiol Biostat Public Health. 2017;14(2):e12267-1.
FNRI. Philippine Nutrition Facts and Figures 2013: 8th National Nutrition Survey Overview. Taguig City, Manila: FNRI Institute; 2015. Available from http://enutrition.fnri.dost.gov.ph/assets/uploads/publications/Overview_8thNNS_050416.pdf. Accessed May 27, 2022.
Barter PJ, Yamashita S, Laufs U, et al. Gaps in beliefs and practice in dyslipidaemia management in Japan, Germany, Colombia and the Philippines: Insights from a web-based physician survey. Lipids Health Dis. 2020;19(1):131. https://pubmed.ncbi.nlm.nih.gov/32522192. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7285462. https://doi.org/10.1186/s12944-020-01265-z.
LaRosa JC, Grundy SM, Waters DD, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med. 2005;352(14):1425-35.
Rodriguez F, Chung S, Blum MR, Coulet A, Basu S, Palaniappan LP. Atherosclerotic cardiovascular disease risk prediction in disaggregated Asian and Hispanic subgroups using electronic health records. J Am Heart Assoc. 2019;8(14):e011874. https://pubmed.ncbi.nlm.nih.gov/31291803. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6662141. https://doi.org/10.1161/JAHA.118.011874.
Wilson PWF, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837-47. https://pubmed.ncbi.nlm.nih.gov/9603539. https://doi.org/10.1161/01.cir.97.18.1837.
Tibrewala A, Jivan A, Oetgen WJ, Stone NJ. A comparative analysis of current lipid treatment guidelines: Nothing stands still. J Am Coll Cardiol. 2018;71(7):794-9. https://pubmed.ncbi.nlm.nih.gov/29447742. https://doi.org/10.1016/j.jacc.2017.12.025.
Liau SY, Mohamed Izham MI, Hassali MA, Shafie AA. A literature review of the cardiovascular risk-assessment tools: Applicability among Asian population. Heart Asia. 2010;2(1):15-8. https://pubmed.ncbi.nlm.nih.gov/27325935. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4898587. https://doi.org/10.1136/ha.2009.001115.
Ancheta IB, Battie CA, Volgman AS, Ancheta CV, Palaniappan L. Cardiovascular disease risk score: Results from the Filipino–American women cardiovascular study. J Racial Ethn Health Disparities. 2017;4(1):25-34. https://pubmed.ncbi.nlm.nih.gov/27294770. https://doi.org/10.1007/s40615-015-0196-6.
Ancheta IB, Battie CA, Tuason MT, Borja-Hart N, Ancheta CV. The prevalence of cardiovascular risk factors and diabetes increases with a body mass index of ≥23 kg/m2 in Filipino American women. Ethn Dis. 2014;24(1):48-54. https://pubmed.ncbi.nlm.nih.gov/24620448.
Gasevic D, Ross ES, Lear SA. Ethnic differences in cardiovascular disease risk factors: A systematic review of North American evidence. Can J Cardiol. 2015;31(9):1169-79. https://pubmed.ncbi.nlm.nih.gov/26239006. https://doi.org/10.1016/j.cjca.2015.06.017.
Goh LGH, Dhaliwal SS, Welborn TA, Lee AH, Della PR. Ethnicity and the association between anthropometric indices of obesity and cardiovascular risk in women: A cross-sectional study. BMJ Open. 2014;4(5):e004702. https://pubmed.ncbi.nlm.nih.gov/24852299. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4039846. https://doi.org/10.1136/bmjopen-2013-004702
Selvarajah S, Kaur G, Haniff J, et al. Comparison of the Framingham Risk Score, SCORE and WHO/ISH cardiovascular risk prediction models in an Asian population. Int J Cardiol. 2014;176(1):211-8. https://pubmed.ncbi.nlm.nih.gov/25070380. https://doi.org/10.1016/J.IJCARD.2014.07.066.
Chia YC, Gray SYW, Ching SM, Lim HM, Chinna K. Validation of the Framingham general cardiovascular risk score in a multiethnic Asian population: A retrospective cohort study. BMJ Open. 2015;5(5):e007324. https://pubmed.ncbi.nlm.nih.gov/25991451. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4442208. https://doi.org/10.1136/BMJOPEN-2014-007324
Lloyd-Jones DM, Braun LT, Ndumele CE, et al. Use of risk assessment tools to guide decision-making in the primary prevention of atherosclerotic cardiovascular disease circulation: Special report from the American Heart Association and American College of Cardiology. Circulation. 2019;139:1162-77. https://pubmed.ncbi.nlm.nih.gov/30586766. https://doi.org/10.1161/CIR.0000000000000638
Ancheta IB, Carlson JM, Battie CA, Borja-Hart N, Cobb S, Ancheta CV. One size does not fit all: Cardiovascular health disparities as a function of ethnicity in Asian-American women. Appl Nurs Res. 2015;28(2):99-105. https://pubmed.ncbi.nlm.nih.gov/25069635. https://doi.org/10.1016/J.APNR.2014.06.001
Pavlović J, Greenland P, Deckers JW, et al. Comparison of ACC/AHA and ESC guideline recommendations following trial evidence for statin use in primary prevention of cardiovascular disease: Results from the population-based rotterdam study. JAMA Cardiol. 2016;1(6):708-13. https://pubmed.ncbi.nlm.nih.gov/27439175. https://doi.org/10.1001/JAMACARDIO.2016.1577
Ridker PM, Cook NR. Statins: New American guidelines for prevention of cardiovascular disease. Lancet. 2013;382(9907):1762-5.https://pubmed.ncbi.nlm.nih.gov/24268611. https://doi.org/10.1016/S0140-6736(13)62388-0
Fox CS, Coady S, Sorlie PD, et al. Increasing cardiovascular disease burden due to diabetes mellitus: The Framingham Heart Study. Circulation. 2007;115(12):1544-50. https://pubmed.ncbi.nlm.nih.gov/17353438. https://doi.org/10.1161/CIRCULATIONAHA.106.658948
Torp-Pedersen C, Jeppesen J. Diabetes and hypertension and atherosclerotic cardiovascular disease: Related or separate entities often found together. Hypertension. 2011;57(5):887-8. https://pubmed.ncbi.nlm.nih.gov/21403088. https://doi.org/10.1161/HYPERTENSIONAHA.110.168583.
Devroey D, Vandevoorde J. The “five risks algorithm”: An easy tool for cardiovascular risk estimation. Cent Eur J Public Health. 2009;17(3):133-8. https://pubmed.ncbi.nlm.nih.gov/20020602. https://doi.org/10.21101/cejph.b0016.
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Bayani Pocholo Maglinte, Alex Junia, Jeremyjones Robles

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Journal of the ASEAN Federation of Endocrine Societies is licensed under a Creative Commons Attribution-NonCommercial 4.0 International. (full license at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.









