The Prevalence of Advanced Liver Fibrosis among Patients with Type 2 Diabetes Mellitus
A Single-Centre Experience in Penang, Malaysia
DOI:
https://doi.org/10.15605/jafes.038.01.08Keywords:
type 2 diabetes mellitus, Non-alcoholic Fatty Liver disease, Advanced Liver Fibrosis, transient elastography, FIB-4 IndexAbstract
Objectives. This study aimed to compare the severity of COVID-19, inflammatory parameters and clinical outcomes
among patients with normal and subnormal levels of Vitamin D.
Methodology. This is a retrospective cohort study of 135 patients admitted in a tertiary hospital for COVID-19. Patients
were grouped according to their Vitamin D level. Primary outcome measure was the composite of all-cause mortality and
morbidity. Other outcome measures determined were the comparison among the groups on the severity of COVID-19
infection, changes in inflammatory parameters, length of hospital stay and duration of respiratory support.
Results. There was a significant trend of higher ICU admission, mortality (p-value= 0.006) and poor clinical outcome
(p-value=0.009) among the Vitamin D deficient group. No significant difference was found for most of the inflammatory
parameters, duration of hospital stay and respiratory support. Overall, patients with deficient, but not insufficient Vitamin
D level had 6 times higher odds of composite poor outcome than those with normal Vitamin D (crude OR=5.18, p-value=
0.003; adjusted OR =6.3, p-value=0.043).
Conclusion. The inverse relationship between Vitamin D level and poor composite outcome observed in our study
suggests that low Vitamin D may be a risk factor for poor prognosis among patients admitted for COVID-19.
Downloads
References
Kuchay MS, Krishan S, Mishra SK, et al. Effect of empagliflozin on liver fat in patients with type 2 diabetes and nonalcoholic fatty liver disease: A randomized controlled trial (E-LIFT Trial). Diabetes Care. 2018;41(8):1801-8. https://pubmed.ncbi.nlm.nih.gov/29895557. https://doi.org/10.2337/dc18-0165.
Wong VW, Wong GL, Yeung DK, et al. Incidence of non-alcoholic fatty liver disease in Hong Kong: A population study with paired proton-magnetic resonance spectroscopy. J Hepatol. 2015;62(1):182-9. https://pubmed.ncbi.nlm.nih.gov/25195550. https://doi.org/10.1016/j.jhep.2014.08.041.
Wong VW, Wong GL, Choi PC, et al. Disease progression of non-alcoholic fatty liver disease: A prospective study with paired liver biopsies at 3 years. Gut. 2010;59(7):969-74. https://pubmed.ncbi.nlm.nih.gov/20581244. https://doi.org/10.1136/gut.2009.205088.
Ascha MS, Hanouneh IA, Lopez R, Tamimi TA, Feldstein AF, Zein NN. The incidence and risk factors of hepatocellular carcinoma in patients with nonalcoholic steatohepatitis. Hepatology. 2010;51(6):1972-8. https://pubmed.ncbi.nlm.nih.gov/20209604. https://doi.org/10.1002/hep.23527.
Bhala N, Angulo P, van der Poorten D, et al. The natural history of nonalcoholic fatty liver disease with advanced fibrosis or cirrhosis: An international collaborative study. Hepatology. 2011;54(4):1208-16. https://pubmed.ncbi.nlm.nih.gov/21688282. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3238674. https://doi.org/10.1002/hep.24491.
Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015;148(3):547-55. https://pubmed.ncbi.nlm.nih.gov/25461851. https://doi.org/10.1053/j.gastro.2014.11.039.
Wong RJ, Cheung R, Ahmed A. Nonalcoholic steatohepatitis is the most rapidly growing indication for liver transplantation in patients with hepatocellular carcinoma in the U.S. Hepatology. 2014;59(6):2188-95. https://pubmed.ncbi.nlm.nih.gov/25461851. https://doi.org/10.1053/j.gastro.2014.11.039.
Lai LL, Wan Yusoff WNI, Vethakkan SR, Nik Mustapha NR, Mahadeva S, Chan WK. Screening for non-alcoholic fatty liver disease in patients with type 2 diabetes mellitus using transient elastography. J Gastroenterol Hepatol. 2019;34(8):1396-1403. https://pubmed.ncbi.nlm.nih.gov/30551263. https://doi.org/10.1111/jgh.14577.
Kwok R, Choi KC, Wong GL, et al. Screening diabetic patients for non-alcoholic fatty liver disease with controlled attenuation parameter and liver stiffness measurements: A prospective cohort study. Gut 2016;65(8):1359-68. https://pubmed.ncbi.nlm.nih.gov/25873639. https://doi.org/10.1136/gutjnl-2015-309265.
European Association for the Study of the Liver (EASL); European Association for the Study of Diabetes (EASD); European Association for the Study of Obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64(6):1388-402. https://pubmed.ncbi.nlm.nih.gov/27062661. https://doi.org/10.1016/j.jhep.2015.11.004.
Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the study of liver diseases. Hepatology. 2018;67(1):328-57. https://pubmed.ncbi.nlm.nih.gov/28714183. https://doi.org/10.1002/hep.29367.
Fallatah HI. Noninvasive biomarkers of liver fibrosis: An overview. Adv Hepatol. 2014:2014:Article ID 357287. https://doi.org/10.1155/2014/357287.
Machado MV, Cortez-Pinto H. Non-invasive diagnosis of non-alcoholic fatty liver disease. A critical appraisal. J Hepatol. 2013;58(5):1007-19. https://pubmed.ncbi.nlm.nih.gov/23183525. https://doi.org/10.1016/j.jhep.2012.11.021.
Musso G, Gambino R, Cassader M, Pagano G. Meta-analysis: Natural history of non-alcoholic fatty liver disease (NAFLD) and diagnostic accuracy of non-invasive tests for liver disease severity. Ann Med. 2011;43(8):617-49. https://pubmed.ncbi.nlm.nih.gov/21039302. https://doi.org/10.3109/07853890.2010.518623.
Castera L. Non-invasive methods to assess liver disease in patients with hepatitis B or C. Gastroenterology. 2012;142(6):1293-302.e4. https://pubmed.ncbi.nlm.nih.gov/22537436. https://doi.org/10.1053/j.gastro.2012.02.017.
Shah AG, Lydecker A, Murray K, et al. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2009;7(10):1104-12. https://pubmed.ncbi.nlm.nih.gov/19523535. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3079239. https://doi.org/10.1016/j.cgh.2009.05.033.
Boursier J, Zarski JP, de Ledinghen V, et al. Determination of reliability criteria for liver stiffness evaluation by transient elastography. Hepatology 2013;57(3):1182-91. https://pubmed.ncbi.nlm.nih.gov/22899556. https://doi.org/10.1002/hep.25993.
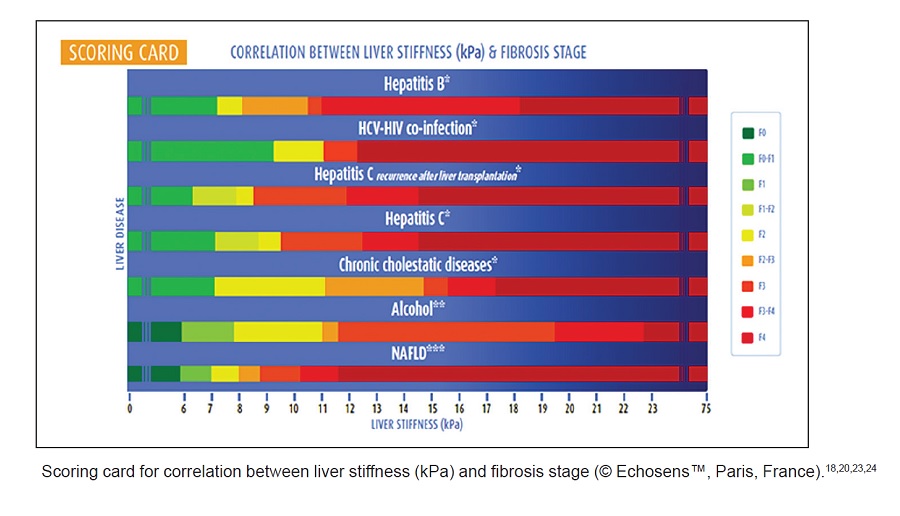
de Lédinghen V, Vergniol J. Transient elastography (FibroScan). Gastroenterol Clin Bio. 2008;32(6 Suppl 1):58-67. https://pubmed.ncbi.nlm.nih.gov/18973847. https://doi.org/10.1016/S0399-8320(08)73994-0.
Castéra L, Foucher J, Bernard PH, et al. Pitfalls of liver stiffness measurement: A 5-year prospective study of 13,369 examinations. Hepatology. 2010;51(3):828-35. https://pubmed.ncbi.nlm.nih.gov/20063276. https://doi.org/10.1002/hep.23425.
Wong VW, Vergniol J, Wong GL, et al. Diagnosis of fibrosis and cirrhosis using liver stiffness measurement in nonalcoholic fatty liver disease. Hepatology. 2010;51(2):454-62. https://pubmed.ncbi.nlm.nih.gov/20101745. https://doi.org/10.1002/hep.23312.
Wong VW, Vergniol J, Wong GL, et al. Liver stiffness measurement using XL probe in patients with nonalcoholic fatty liver disease. Am J Gastroenterol. 2012;107(12):1862-71. https://pubmed.ncbi.nlm.nih.gov/23032979. https://doi.org/10.1038/ajg.2012.331.
Castera L, Forns X, Alberti A. Non-invasive evaluation of liver fibrosis using transient elastography. J Hepatol 2008;48(5):835–47. https://pubmed.ncbi.nlm.nih.gov/18334275. https://doi.org/10.1016/j.jhep.2008.02.008.
Nahon P, Kettaneh A, Tengher-Barna I, et al. Assessment of liver fibrosis using transient elastography in patients with alcoholic liver disease. J Hepatol. 2008;49(6):1062-8. https://pubmed.ncbi.nlm.nih.gov/18930329. https://doi.org/10.1016/j.jhep.2008.08.011.
Nguyen-Khac E, Chatelain D, Tramier B, et al. Assessment of asymptomatic liver fibrosis in alcoholic patients using fibroscan: Prospective comparison with seven non-invasive laboratory tests. Aliment Pharmacol Ther. 2008;28(10):1188-98. https://pubmed.ncbi.nlm.nih.gov/18705692. https://doi.org/10.1111/j.1365-2036.2008.03831.x.
Sterling RK, Lissen E, Clumeck N, et al.; APRICOT Clinical Investigators. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology. 2006;43(6):1317-25. https://pubmed.ncbi.nlm.nih.gov/16729309. https://doi.org/10.1002/hep.21178.
de Lédinghen V, Vergniol J, Gonzalez C, et al. Screening for liver fibrosis by using FibroScan(®) and FibroTest in patients with diabetes. Dig Liver Dis. 2012;44(5):413-8. https://pubmed.ncbi.nlm.nih.gov/22285146. https://doi.org/10.1016/j.dld.2011.12.005.
Roulot D, Roudot-Thoraval F, NKontchou G, et al. Concomitant screening for liver fibrosis and steatosis in French type 2 diabetic patients using Fibroscan. Liver Int. 2017;37(12):1897-1906. https://pubmed.ncbi.nlm.nih.gov/28556413. https://doi.org/10.1111/liv.13481.
Sporea I, Mare R, Lupușoru R, et al. Liver stiffness evaluation by transient elastography in type 2 diabetes mellitus patients with ultrasound-proven steatosis. J Gastrointestin Liver Dis. 2016;25(2):167-74. https://pubmed.ncbi.nlm.nih.gov/27308647. https://doi.org/10.15403/jgld.2014.1121.252.lsf.
Zhao H, Song X, Li Z, Wang X. Risk factors associated with nonalcohol fatty liver disease and fibrosis among patients with type 2 diabetes mellitus. Medicine (Baltimore). 2018;97(37):e12356. https://pubmed.ncbi.nlm.nih.gov/30212992. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6156034. https://doi.org/10.1097/MD.0000000000012356.
Metcalfe C. Biostatistics: A foundation for analysis in the health sciences, 7th ed. Wayne W. Daniel, Wiley. Stat Med. 2001;20(2):324-6. https://doi.org/10.1002/1097-0258(20010130)20:2<324::AID-SIM635>3.0.CO;2-O.
National Institutes of Health, Ministry of Health Malaysia. None-communicable diseases, healthcare demand, and health literacy. National Health and Morbidity Survey 2019. Accessed September 20, 2020. http://mpaeds.my/national-health-and-morbidity-survey-2019.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157-63. https://pubmed.ncbi.nlm.nih.gov/4726171. https://doi.org/10.1016/S0140-6736(03)15268-3.
Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the study of liver diseases. Hepatology. 2018;67(1):328-57. https://pubmed.ncbi.nlm.nih.gov/28714183. https://doi.org/10.1002/hep.29367.
Boursier J, Calès P. Controlled attenuation parameter (CAP): A new device for fast evaluation of liver fat? Liver Int. 2012;32(6):875-7. https://pubmed.ncbi.nlm.nih.gov/22672640. https://doi.org/10.1111/j.1478-3231.2012.02824.x.
Wong VW, Chan WK, Chitturi S, et al. Asia-Pacific working party on non-alcoholic fatty liver disease guidelines 2017-part 1: Definition, risk factors and assessment. J Gastroenterol Hepatol. 2018;33(1):70-85. https://pubmed.ncbi.nlm.nih.gov/28670712. https://doi.org/10.1111/jgh.13857.
Ekstedt M, Hagström H, Nasr P, et al. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology. 2015;61(5):1547-54. https://pubmed.ncbi.nlm.nih.gov/25125077. https://doi.org/10.1002/hep.27368.
Angulo P, Machado MV, Diehl AM. Fibrosis in nonalcoholic Fatty liver disease: Mechanisms and clinical implications. Semin Liver Dis. 2015;35(2):132-45. https://pubmed.ncbi.nlm.nih.gov/25974899. https://doi.org/10.1055/s-0035-1550065.
Stål P. Liver fibrosis in non-alcoholic fatty liver disease - diagnostic challenge with prognostic significance. World J Gastroenterol. 2015;21(39):11077-87. https://pubmed.ncbi.nlm.nih.gov/26494963. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4607906. https://doi.org/10.3748/wjg.v21.i39.11077.
Hagström H, Nasr P, Ekstedt M, et al. Fibrosis stage but not NASH predicts mortality and time to development of severe liver disease in biopsy-proven NAFLD. J Hepatol. 2017;67(6):1265-73. https://pubmed.ncbi.nlm.nih.gov/28803953. https://doi.org/10.1016/j.jhep.2017.07.027.
AURORA: Phase 3 study for the efficacy and safety of Cenicriviroc (CVC) for the treatment of liver fibrosis in adults with nonalcoholic steatohepatitis (NASH) (AURORA). Accessed October 15, 2020. http:// clinicaltrials.gov/ct2/show/NCT03028740.
Phase 3 study to evaluate the efficacy and safety of elafibranor versus placebo in patients with nonalcoholic steatohepatitis (NASH) (RESOLVE-IT). Accessed October 15, 2020. http://clinicaltrials.gov/ct2/show/NCT02704403.
Younossi ZM, Ratziu V, Loomba R, et al.; REGENERATE Study Investigators. Obeticholic acid for the treatment of non-alcoholic steatohepatitis: Interim analysis from a multicentre, randomised, placebo-controlled phase 3 trial. Lancet. 2019;394(10215):2184-96. https://pubmed.ncbi.nlm.nih.gov/31813633. https://doi.org/10.1016/S0140-6736(19)33041-7.
Study evaluating the efficacy and safety of obeticholic acid in subjects with compensated cirrhosis due to nonalcoholic steatohepatitis (REVERSE). Accessed October 15, 2020. http:// clinicaltrials.gov/ct2/show/NCT03439254.
A phase 3 study to evaluate the efficacy and safety of mgl-3196 (resmetirom) in patients with NASH and fibrosis (MAESTRO-NASH). Accessed October 15, 2020. http:// clinicaltrials.gov/ct2/show/NCT03900429.
A phase ¾ clinical study to evaluate the efficacy and safety of aramchol versus placebo in subjects with NASH (ARMOR). Accessed October 15, 2020. http:// clinicaltrials.gov/ct2/show/NCT04104321.
Wong VW, Wong GL, Tsang SW, et al. Metabolic and histological features of non-alcoholic fatty liver disease patients with different serum alanine aminotransferase levels. Aliment Pharmacol Ther. 2009;29(4):387-96. https://pubmed.ncbi.nlm.nih.gov/19035982. https://doi.org/10.1111/j.1365-2036.2008.03896.x.
Guidelines for the prevention, care and treatment of persons with chronic hepatitis B infection. Geneva: World Health Organization; 2015. http://apps.who.int/iris/bitstream/handle/10665/154590/9789241549059_eng.pdf.
Prati D, Taioli E, Zanella A, et al. Updated definitions of healthy ranges for serum alanine aminotransferase levels. Ann Intern Med. 2002;137(1):1-10. https://pubmed.ncbi.nlm.nih.gov/12093239. https://doi.org/10.7326/0003-4819-137-1-200207020-00006.
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Xe Hui Lee, Lisa Mohamed Nor, Choon Seong Ang, Toh Peng Yeow, Shueh Lin Lim

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The full license is at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.










