Predictors of Outcomes of Foot Ulcers among Individuals with Type 2 Diabetes Mellitus in an Outpatient Foot Clinic
DOI:
https://doi.org/10.15605/jafes.036.02.14Keywords:
foot ulcer, amputation, neuropathy, peripheral arterial diseaseAbstract
Objectives. To determine the risk factors for recurrence and persistence of non-healing foot ulcer resulting in minor and major amputations,.
Methodology. This was an ambispective cohort analysis of persons with diabetic foot ulcers consulting at the diabetic foot clinic of East Avenue Medical Center. Data were analyzed through multiple logistic regression.
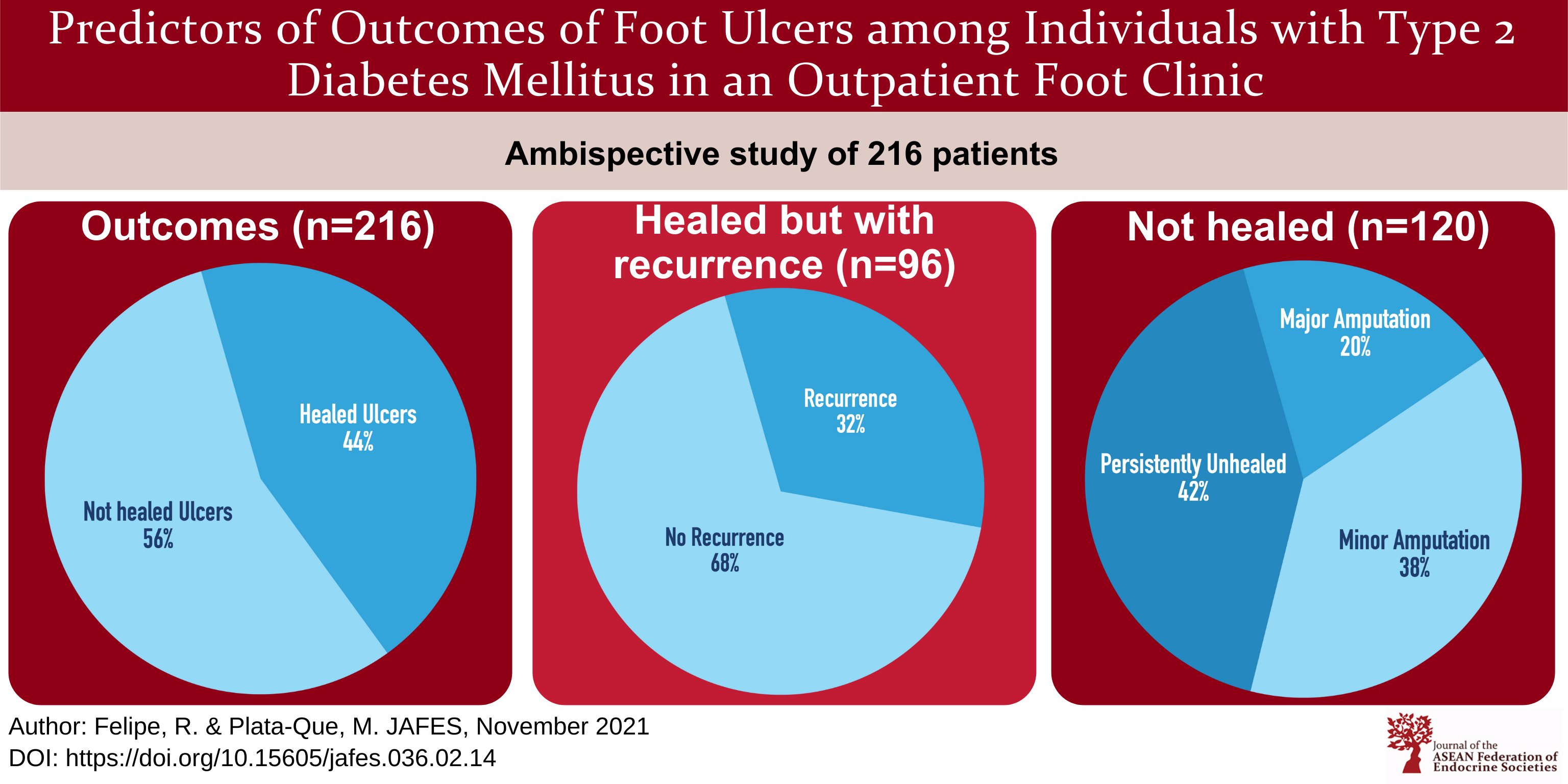
Result. Two hundred sixteen patients with Type 2 Diabetes Mellitus and diabetic foot ulcers were included in the analysis; 50.9% were males and the mean age of the cohort was 55.8 ± 9.9 years. Outcomes of foot ulcers were: healed 44.5% (healed with no recurrence 30%, healed but with recurrence 14.5%) and not healed 55.5% (major amputation 11%, minor amputation, 21.5%, and persistently non-healing 23%). Multivariate logistic regression showed the following were independent risk factors for persistent non-healing ulcer: osteomyelitis (OR 66.5; CI 19.7, 217.8), smoking (OR 28.9; CI 6.8, 129.3, and peripheral arterial disease (PAD) (OR 56.8; CI 2.5, 877.2). Independent risk factors for ulcer recurrence were: plantar location of ulcer (OR 16.8; CI 6.8, 89.4), presence of more than one ulcer (OR 7.8; CI 3.6,31.6), and neuropathy (OR 11.2; CI 7.2, 19.9). For healed foot ulcers, mean healing time was 14 ± 3 weeks. Healing time was significantly reduced from 12 weeks to 4.5 weeks (p<0.001) if patients consulted earlier (within 4 weeks from sustaining an ulcer).
Conclusion. Only half (55%) of patients with diabetic foot ulcers consulting in a dedicated outpatient foot clinic had an adverse outcome of foot ulcers (major amputation 11%, minor amputation, 21.5%, and persistently non-healing ulcer 23%) while a small portion (14.5%) of patients had recurrent foot ulcers. Arterial obstruction, smoking, low hemoglobin, neuropathy, and osteomyelitis increase the likelihood of healing failure while the presence of multiple ulcers, plantar location of ulcers, and neuropathy increase the risk of ulcer recurrence.
Downloads
References
Boulton AJ. The diabetic foot: Grand overview, epidemiology and pathogenesis. Diabetes Metab Res Rev. 2008;24(Suppl 1):S3–6. https://pubmed.ncbi.nlm.nih.gov/18442166. https://doi.org/10.1002/dmrr.833.
Cardino M, Josol C, Isip-Tan I. Quality of care and outcomes of diabetic extremity patients after the implementation of the revised Diabetes Extremity Care Team Protocol of the Philippine General Hospital. Philipp J Intern Med. 2009;47(2):57-63. https://drive.google.com/file/d/1D7qrRr6hdtaI3POF3nBxDczoy6HqIMIg/view.
Pemayun TGD, Naibaho RM. Clinical profile and outcome of diabetic foot ulcer, a view from tertiary care hospital in Semarang, Indonesia. Diabet Foot Ankle. 2017;18(1):1312974. https://pubmed.ncbi.nlm.nih.gov/28649296. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5475294. https://doi.org/10.1080/2000625X.2017.1312974.
Riaz M, Miyan Z, Zaidi SI, et al. Characteristics and outcomes of subjects with diabetic foot ulceration. Diabetes Care. 2012;35(9):e63. https://pubmed.ncbi.nlm.nih.gov/22923685. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3425011. https://doi.org/10.2337/dc11-1906.
Jeffcoate, WJ, Chipchase SY, Ince P,Game FL. Assessing the outcome of the management of diabetic foot ulcers using ulcer-related and person-related measures. Diabetes Care. 2006;29(8):1784-7. https://pubmed.ncbi.nlm.nih.gov/16873780. https://doi.org/10.2337/dc06-0306.
Peters EJ, Armstrong DG, Lavery LA. Risk factors for recurrent diabetic foot ulcers: Site matters. Diabetes Care. 2007;30(8):2077-9. https://pubmed.ncbi.nlm.nih.gov/17507693. https://doi.org/10.2337/dc07-0445.
Messenger G, Masoetsa R, Hussain I, Devarajan S, Jahromi M. Diabetic foot ulcer outcomes from a podiatry led tertiary service in Kuwait. Diabet Foot Ankle. 2018;9(1):1471927. https://pubmed.ncbi.nlm.nih.gov/29868165. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5974709. https://doi.org/10.1080/2000625X.2018.1471927.
Fife CE, Horn SD, Smout RJ, Barrett RS, Thomson B. A predictive model for diabetic foot ulcer outcome: The wound healing index. Adv Wound Care (New Rochelle). 2016;5(7):279–87. https://pubmed.ncbi.nlm.nih.gov/27366589. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4900227. https://doi.org/10.1089/wound.2015.0668.
Chang AO, Eslao EA, Panilagao GP, Quimpo JA. Diabetic foot ulcers - experience at the Philippine General Hospital. Philipp J Intern Med. 1996;34(6):205-9. https://drive.google.com/file/d/1Gkqgl87I3_Tc4nXnarrTpApY6e8H-iLE/view.
Balderas JAJ, Oribio RU, Racho V, Lim-Abrahan MA. Diabetic extremity management by a multidisciplinary care team: The PGH Experience. Philipp J Intern Med. 1999;37 (5):246-52. https://drive.google.com/file/d/1G92oS9Exc1Cqb5uVgGYVaCvbVnQDMDA1/view.
Cardino MJT, Josol CV, Isip-Tan I, Jimeno CA. Risk factors for major amputation of diabetic foot ulcers. Philipp J Intern Med. 2011;49(2):74-8.
Panuda JP, Macalalad-Josue AA, Buenaluz-Sedurante M. Factors associated with in-hospital mortality among patients with diabetes admitted for lower extremity infections. J ASEAN Fed Endocr Soc. 2019;34(1):36-43. https://pubmed.ncbi.nlm.nih.gov/33442135. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7784136. https://doi.org/10.15605/jafes.034.01.07.
Schaper NC, van Netten JJ, Apelqvist J, et al. IWGDF practical guidelines on the prevention and management of diabetic foot disease. https://iwgdfguidelines.org/wp-content/uploads/2021/03/IWGDF-2019-final.pdf. Accessed June 1, 2020.
Gonzalez-Santos LE, Oliva R, Jimeno CA, et al. Executive summary of the 2020 Clinical Practice Guidelines for the management of dyslipidemia in the Philippines: 2020 Dyslipidemia CPG. J ASEAN Fed Endocr Soc. 2021:36(1), 5-11. https://pubmed.ncbi.nlm.nih.gov/34177082. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8214350. https://doi.org/10.15605/jafes.036.01.01.
Moghtaderi A, Bakhshipour A, Rashidi H. Validation of Michigan neuropathy screening instrument. Clin Neurol Neurosurg. 2006;108(5):477-81. https://pubmed.ncbi.nlm.nih.gov/16150538. https://doi.org/10.1016/j.clineuro.2005.08.003.
Herman WH, Pop-Busui R, Braffett BH, et al. Use of Michigan Neuropathy Screening Instrument as a measure of distal symmetrical peripheral neuropathy in type 1 diabetes: results from the diabetes control and complications trial/epidemiology of diabetes interventions and complications. Diabet Med. 2012;29(7);937-44. https://pubmed.ncbi.nlm.nih.gov/22417277. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3641573. https://doi.org/10.1111/j.1464-5491.2012.03644.x.
Aboyans V, Ho E, Denenberg JO, Ho LA, Natarajan L, Criqui MH. The association between elevated ankle systolic pressures and peripheral occlusive arterial disease in diabetic and nondiabetic subjects. J VascSurg. 2008;48(5):1197–203. https://pubmed.ncbi.nlm.nih.gov/18692981. https://doi.org/10.1016/j.jvs.2008.06.005.
Reiber GE, Pecoraro RE, Koepsell TD. Risk factors for amputation in patients with diabetes mellitus. A case-control study. Ann Intern Med. 1992;117(2):97–105. https://pubmed.ncbi.nlm.nih.gov/1605439. https://doi.org/10.7326/0003-4819-117-2-97.
Boulton AJ, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J. The global burden of diabetic foot disease. Lancet. 2005;366(9498):1719–24. https://pubmed.ncbi.nlm.nih.gov/16291066. https://doi.org/10.1016/S0140-6736(05)67698-2.
Lavery LA, Ashry HR, van Houtum W, Pugh JA, Harkless LB, Basu S. Variation in the incidence and proportion of diabetes-related amputations in minorities. Diabetes Care. 1996;19(1):48–52. https://pubmed.ncbi.nlm.nih.gov/8720533. https://doi.org/10.2337/diacare.19.1.48.
Nicolau DP, Stein GE. Therapeutic options for diabetic foot infections: a review with an emphasis on tissue penetration characteristics. J Am Podiatr Med Assoc. 2010;100(1):52–63. https://pubmed.ncbi.nlm.nih.gov/20093545. https://doi.org/10.7547/1000052.
Faglia E, Clerici G, Caminiti M, Curci V, Somalvico F. Influence of osteomyelitis location in the foot of diabetic patients with transtibial amputation. Foot Ankle Int. 2013;34(2):222–7. https://pubmed.ncbi.nlm.nih.gov/23413061. https://doi.org/10.1177/1071100712467436.
Musa HG, Ahmed ME. Associated risk factors and management of chronic diabetic foot ulcers exceeding 6 months' duration. Diabet Foot Ankle. 2012;3. https://pubmed.ncbi.nlm.nih.gov/23119125. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3485402. https://doi.org/10.3402/dfa.v3i0.18980.
Marston WA, Dermagraft Diabetic Foot Ulcer Study Group. Risk factors associated with healing chronic diabetic foot ulcers: The importance of hyperglycemia. Ostomy Wound Manage. 2006;52(3):26–8. https://pubmed.ncbi.nlm.nih.gov/16567857.
Margolis DJ, Kantor J, Santanna J, Strom BL, Berlin JA. Risk factors for delayed healing of neuropathic diabetic foot ulcers: A pooled analysis. Arch Dermatol. 2000;136(12):1531–5. PMID: 11115166. https://doi.org/10.1001/archderm.136.12.1531.
Poredos P, Jug B. The prevalence of peripheral arterial disease in high risk subjects and coronary or cerebrovascular patients. Angiology. 2007;58(3):309-15. PMID: 17626985. https://doi.org/10.1177/0003319707302494.
Waaijman R, de Haart M, Arts ML, et al. Risk factors for plantar foot ulcer recurrence in neuropathic diabetic patients. Diabetes Care. 2014;37(6):1697–705. PMID: 24705610. https://doi.org/10.2337/dc13-2470.
Khalifa WA. Risk factors for diabetic foot ulcer recurrence: A prospective 2-year follow-up study in Egypt. Foot (Edinb). 2018;35:11–5. PMID: 29753996. https://doi.org/10.1016/j.foot.2017.12.004.
Xiang J, Wang S, He Y, Xu L, Zhang S, Tang Z. Reasonable glycemic control would help wound healing during the treatment of diabetic foot ulcers. Diabetes Ther. 2019;10(1):95-105. PMID: 30465160. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6349287. https://doi.org/10.1007/s13300-018-0536-8.
Christman AL, Selvin E, Margolis DJ, Lazarus GS, Garza LA. Hemoglobin A1c predicts healing rate in diabetic wounds. J Invest Dermatol. 2011;131(10):2121-7. PMID: 21697890. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3174328. https://doi.org/10.1038/jid.2011.176.
Fesseha BK, Abularrage CJ, Hines KF, et al. Association of hemoglobin A1C and wound healing in diabetic foot ulcers. Diabetes Care. 2018;41(7):1478-85. PMID: 29661917. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6014539. https://doi.org/10.2337/dc17-1683.
Ozenç S, Simsek K, Yildirim AO, et al. Association between the development of diabetic foot and serum fetuin A levels. Pol Arch Med Wewn. 2013;123(10):513-8. PMID: 23974250. https://doi.org/10.20452/pamw.1921.
Sarinnapakorn, V, Sunthorntepwarakul T, Deerochanawong C, Niramitmahapanya S, Napartivaumnuay N. Prevalence of diabetic foot ulcers and risk classifications in type 2 diabetes mellitus patients at Rajavithi hospital. J Med Assoc Thai. 2016;99(Suppl 2):S99-105. PMID: 27266223.
Published
How to Cite
Issue
Section
License
Copyright (c) 2021 Roy Raoul Felipe, Ma. Teresa Plata-Que

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The full license is at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.










