Accuracy and Cost-effectiveness of the Diabetic Foot Screen Proforma in Detection of Diabetic Peripheral Neuropathy in Myanmar
DOI:
https://doi.org/10.15605/jafes.037.01.06Keywords:
foot screening, diabetic peripheral neuropathy, biothesiometry, cost-effectiveness, Myanmar primary careAbstract
Objective. Proper foot assessment is important for early detection and treatment of diabetic peripheral neuropathy (DPN), the main cause of diabetic foot ulcers (DFUs). This study aimed to determine the accuracy and cost-effectiveness of the locally developed Diabetic Foot Screen (DFS) proforma in detecting DPN among diabetic patients at 10 selected clinics in Yangon, Myanmar.
Methodology. The study included 625 type 2 diabetics from 10 primary care clinics who participated in the diagnostic accuracy and cost-effectiveness analysis. They were assessed with DFS proforma and biothesiometry by two examiners independently. The cost-effectiveness analysis was conducted based on available data in the local primary care setting.
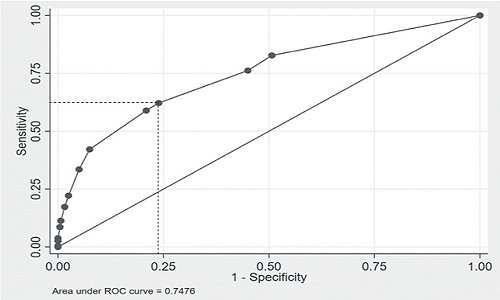
Results. The overall accuracy of the DFS proforma assessment was 74.76% (95% CI: 70.46%- 79.06%). The optimal cut-off DFS score was ≥1.5 (sensitivity 62%; specificity 76%) in detecting DPN. Compared to biothesiometry, the cost-effectiveness of DFS proforma assessment in DPN detection was 41.79 USD per DPN case detected.
Conclusion. This study supported the use of DFS proforma for DPN detection in primary care clinics. It also provided new information on the estimated costs per patient with DPN detected in Myanmar.
Downloads
References
WHO. Global Report on diabetes. 2016. ISBN: 9789241565257. https://www.who.int/publications/i/item/9789241565257
Williams R, Colagiuri S, Almutairi R. IDF Diabetes Atlas International Diabetes Federation 2019. 2019. http://www.idf.org/about-diabetes/facts-figures.
WHO. Myanmar World Health Organization – Diabetes country profiles. 2016. https://www.who.int/diabetes/country-profiles/mmr_en.pdf.
Myanmar Ministry of Health. Myanmar STEPS noncommunicable disease risk factors survey. https://pubmed.ncbi.nlm.nih.gov/23801792. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3687278. https://doi.org/10.2337/dc12-2285.
Armstrong DG, Kanda VA, Lavery LA, Marston W, Mills JL, Boulton AJM. Mind the gap: Disparity between research funding and costs of care for diabetic foot ulcers. Diabetes Care. 2013;36(7):1815-1817. https://care.diabetesjournals.org/content/36/7/1815
Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. 2005;293(2):217-28. https://pubmed.ncbi.nlm.nih.gov/15644549. https;//doi.org/10.1001/jama.293.2.217.
Boulton AJM. Management of diabetic peripheral neuropathy. Clin Diabetes. 2005;23(1):9-15. https://doi.org/10.2337/diaclin.23.1.9.
Win MMTM, Fukai K, Nyunt HH, Hyodo Y, Linn KZ. Prevalence of peripheral neuropathy and its impact on activities of daily living in people with type 2 diabetes mellitus. Nurs Heal Sci. 2019;21(4):445-53. https://pubmed.ncbi.nlm.nih.gov/31215149. https://doi.org/10.1111/nhs.12618.
American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2020;43(Suppl 1): S1-212.
Boulton AJM, Armstrong DG, Albert SF, et al. Comprehensive foot examination and risk assessment: A report of the task force of the foot care interest group of the American Diabetes Association, with endorsement by the American Association of Clinical Endocrinologists. Diabetes Care. 2008;31(8):1679-85. https://pubmed.ncbi.nlm.nih.gov/18663232. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2494620. https://doi.org/10.2337/dc08-9021.
Myanmar Ministry of Health and Sports. Myanmar Diabetic Foot Care Program. MOHS; 2016.
Pinzon RT, Kes M, Lima R. Sa R De. Diabetic peripheral neuropathy: Is it underdiagnosed? Asian J Biol Sci. 2020;13(2):168-72. https://doi.org/10.3923/ajbs.2020.168.172.
Dros J, Wewerinke A, Bindels PJ, Van Weert HC. Accuracy of monofilament testing to diagnose peripheral neuropathy: A systematic review. Ann Fam Med. 2009;7(6):555-8. https://pubmed.ncbi.nlm.nih.gov/19901316. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2775618. https://doi.org/10.1370/afm.1016.
Jayaprakash P, Bhansali A, Bhansali S, et al. Validation of bedside methods in evaluation of diabetic peripheral neuropathy. Indian J Med Res. 2011;133(6):645-9. https://pubmed.ncbi.nlm.nih.gov/21727664. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3135993.
Al-Geffari M. Comparison of different screening tests for diagnosis of diabetic peripheral neuropathy in primary health care setting. Int J Health Sci (Qassim). 2012;6(2):127-34. https://pubmed.ncbi.nlm.nih.gov/23580893. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3616942. https://doi.org/10.12816/0005988.
Moghtaderi A, Bakhshipour A, Rashidi H. Validation of Michigan neuropathy screening instrument for diabetic peripheral neuropathy. Clin Neurol Neurosurg. 2006;108(5):477-81. https://pubmed.ncbi.nlm.nih.gov/16150538. https://doi.org/10.1016/j.clineuro.2005.08.003
World Bank Group. GDP per capita (current US$) - Myanmar. 2019. Accessed April 27, 2021. https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?locations=MM.
Published
How to Cite
Issue
Section
License
The full license is at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.










