Gastric Outlet Obstruction following Recurrent Pancreatitis Uncovers A Giant Parathyroid Adenoma
A Case Report
DOI:
https://doi.org/10.15605/jafes.037.01.11Keywords:
Giant parathyroid adenoma, pancreatitis, gastric outlet obstruction, primary hyperparathyroidismAbstract
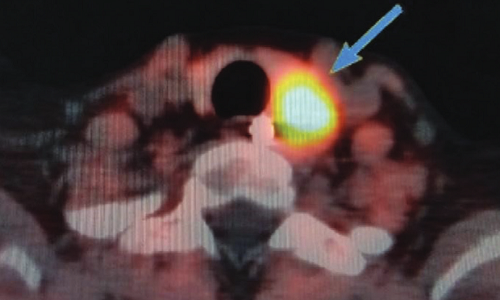
A 35-year-old female presented with abdominal pain, fever, projectile vomiting, and a diffuse tender epigastric mass. She was diagnosed to have acute persistent pancreatitis with a pancreatic pseudocyst. Elevated serum calcium levels provided an etiologic link between hypercalcemia and pancreatitis. On examination, a nodule was found in the left side of her neck which was later diagnosed as a giant left inferior parathyroid adenoma. This report highlights the critical analysis of history, examination, and investigations to reach an ultimate diagnosis. Pseudocyst drainage and parathyroidectomy resolved her symptoms.
Downloads
References
Sunkara T, Caughey ME, Rawla P, Yarlagadda KS, Gaduputi V. Severe acute pancreatitis as an index clinical manifestation of parathyroid adenoma. Cureus. 2018;10(4):e2445. https://pubmed.ncbi.nlm.nih.gov/29888149. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5991921. https://doi.org/10.7759/cureus.2445.
Aslam M, Talukdar R, Jagtap N, et al. Clinical profile and outcome of parathyroid adenoma-associated pancreatitis. Saudi J Med Med Sci. 2018;6(2):95-9. https://pubmed.ncbi.nlm.nih.gov/30787828. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6196711. https://doi.org/ 10.4103/sjmms.sjmms_80_17.
Rubin MR, Bilezikian JP, McMahon DJ, et al. The natural history of primary hyperparathyroidism with or without parathyroid surgery after 15 years. J Clin Endocrinol Metab. 2008;93(9):3462-70. https://pubmed.ncbi.nlm.nih.gov/18544625. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2567863. https://doi.org/10.1210/jc.2007-1215.
Jha S, Jayaraman M, Jha A, Jha R, Modi KD, Kelwadee JV. Primary hyperparathyroidism: A changing scenario in India. Indian J Endocrinol Metab. 2016;20(1):80-3. https://pubmed.ncbi.nlm.nih.gov/26904473. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4743389. https://doi.org/ 10.4103/2230-8210.172237.
Krishnamurthy A, Raghunandan GC, Ramshankar V. A rare case of giant parathyroid adenoma presenting with recurrent episodes of pancreatitis. Indian J Nucl Med. 2016;31(1):36-8. https://pubmed.ncbi.nlm.nih.gov/26917892. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4746839. https://doi.org/10.4103/0972-3919.172355.
Al-Hassan MS, Mekhaimar M, El Ansari W, Darweesh A, Abdelaal A. Giant parathyroid adenoma: A case report and review of the literature. J Med Case Rep. 2019;13(1):332. https://pubmed.ncbi.nlm.nih.gov/31722742. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6854700. https://doi.org/10.1186/s13256-019-2257-7.
Spanheimer PM, Stoltze AJ, Howe JR, Sugg SL, Lal G, Weigel RJ. Do giant parathyroid adenomas represent a distinct clinical entity? Surgery. 2013;154(4):714-8. https://pubmed.ncbi.nlm.nih.gov/23978594. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3787983. https://doi.org/10.1016/j.surg.2013.05.013.
Garas G, Poulasouchidou M, Dimoulas A, Hytiroglou P, Kita M, Zacharakis E. Radiological considerations and surgical planning in the treatment of giant parathyroid adenomas. Ann R Coll Surg Engl. 2015;97(4):e64-6. https://pubmed.ncbi.nlm.nih.gov/26263956. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4473887. https://doi.org/10.1308/003588415X14181254789682.
Mantzoros I, Kyriakidou D, Galanos-Demiris K, et al. A rare case of primary hyperparathyroidism caused by a giant solitary parathyroid adenoma. Am J Case Rep. 2018;19:1334-7. https://pubmed.ncbi.nlm.nih.gov/30405093. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6238585. https://doi.org/ 10.12659/AJCR.911452.
Kelly KJ, Chen H, Sippel RS. Primary hyperparathyroidism. Cancer Treat Res. 2010;153:87-103. https://pubmed.ncbi.nlm.nih.gov/19957221. https://doi.org/10.1007/978-1-4419-0857-5_6.
Bai HX, Giefer M, Patel M, Orabi AI, Husain SZ. The association of primary hyperparathyroidism with pancreatitis. J Clin Gastroenterol. 2012;46(8):656-61. https://pubmed.ncbi.nlm.nih.gov/22874807. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4428665. https://doi.org/10.1097/MCG.0b013e31825c446c.
Arya AK, Bhadada SK, Mukherjee S, et al. Frequency & predictors of pancreatitis in symptomatic primary hyperparathyroidism. Indian J Med Res. 2018;148(6):721-7. https://pubmed.ncbi.nlm.nih.gov/30778006. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6396558. https://doi.org/10.4103/ijmr.IJMR_353_16.
Carnaille B, Oudar C, Pattou F, Combemale F, Rocha J, Proye C. Pancreatitis and primary hyperparathyroidism: Forty cases. Aust N Z J Surg. 1998;68(2):117-9. https://pubmed.ncbi.nlm.nih.gov/9494002. https://doi.org/10.1111/j.1445-2197.1998.tb04719.x.
Felderbauer P, Karakas E, Fendrich V, Lebert R, Bartsch DK, Bulut K. Multifactorial genesis of pancreatitis in primary hyperparathyroidism: evidence for “protective” (PRSS2) and “destructive” (CTRC) genetic factors. Exp Clin Endocrinol Diabetes. 2011;119(1):26–9. https://pubmed.ncbi.nlm.nih.gov/20625975. https://doi.org/10.1055/s-0030-1255106.
Imrie CW, Buist LJ, Shearer MG. Importance of cause in the outcome of pancreatic pseudocysts. Am J Surg. 1988;156 (3 Pt 1):159-62. https://pubmed.ncbi.nlm.nih.gov/2458684. https://doi.org/10.1016/s0002-9610(88)80055-2.
Boerma D, Obertop H, Gouma DJ. Pancreatic pseudocysts in chronic pancreatitis. Surgical or interventional drainage? Ann Ital Chir. 2000;71(1):43-50. https://pubmed.ncbi.nlm.nih.gov/10829523.
Gouyon B, Lévy P, Ruszniewski P, et al. Predictive factors in the outcome of pseudocysts complicating alcoholic chronic pancreatitis. Gut. 1997;41(6):821-5. https://pubmed.ncbi.nlm.nih.gov/9462217. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1891603. https://doi.org/10.1136/gut.41.6.821.
Zhang Y, Zhang SY, Gao SL, Liang ZY, Yu WQ, Liang TB. Successful resolution of gastric outlet obstruction caused by pancreatic pseudocyst or walled-off necrosis after acute pancreatitis: The role of percutaneous catheter drainage. Pancreas. 2015;44(8):1290-5. https://pubmed.ncbi.nlm.nih.gov/26465954. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4947542. https://doi.org/10.1097/MPA.0000000000000429.
Aranha GV, Prinz RA, Greenlee HB, Freeark RJ. Gastric outlet and duodenal obstruction from inflammatory pancreatic disease. Arch Surg. 1984;119(7):833–5. https://doi.org/10.1001/archsurg.1984.01390190071016.
Agalianos C, Passas I, Sideris I, Davides D, Dervenis C. Review of management options for pancreatic pseudocysts. Transl Gastroenterol Hepatol. 2018;3:18. https://pubmed.ncbi.nlm.nih.gov/29682625. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5897675. https://doi.org/10.21037/tgh.2018.03.03.
Borumandi F, Daultrey H, Laji K, Bosman D, Ashford N, Alam P. Detectability and surgical outcomes in parathyroid surgery - a single-centre experience. Br J Oral Maxillofac Surg. 2019;57(4):330-5. https://pubmed.ncbi.nlm.nih.gov/30930031. https://doi.org/10.1016/j.bjoms.2019.03.007.
Lezaic L, Rep S, Sever MJ, Kocjan T, Hocevar M, Fettich J. ¹⁸F-Fluorocholine PET/CT for localization of hyperfunctioning parathyroid tissue in primary hyperparathyroidism: a pilot study. Eur J Nucl Med Mol Imaging. 2014s;41(11):2083-9. https://pubmed.ncbi.nlm.nih.gov/25063039. https://doi.org/10.1007/s00259-014-2837-0.
Prabhu M, Damle NA. Fluorocholine PET imaging of parathyroid disease. Indian J Endocrinol Metab. 2018;22(4):535-41. https://pubmed.ncbi.nlm.nih.gov/30148104. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6085954. https://doi.org/10.4103/ijem.IJEM_707_17.
Witteveen JE, van Thiel S, Romijn JA, Hamdy NA. Hungry bone syndrome: still a challenge in the post-operative management of primary hyperparathyroidism: A systematic review of the literature. Eur J Endocrinol. 2013;168(3):R45-53. https://pubmed.ncbi.nlm.nih.gov/23152439. https://doi.org/10.1530/EJE-12-0528.
Misgar RA, Mathew V, Pandit K, Chowdhury S. Primary hyperparathyroidism presenting as recurrent acute pancreatitis: A case report and review of literature. Indian J Endocrinol Metab. 2011;15(1):54-6. https://pubmed.ncbi.nlm.nih.gov/21584170. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3079873. https://doi.org/10.4103/2230-8210.77588.
Vera C, Díez M, San Román R, Ratia T, Granell J. Primary hyperparathyroidism and acute pancreatitis. Endocrinol Nutr. 2013;60(5):275–6. https://pubmed.ncbi.nlm.nih.gov/23332718, https://doi.org/10.1016/j.endoen.2012.05.005.
Published
How to Cite
Issue
Section
License
The full license is at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.










