Comparison of Maternal and Neonatal Outcomes Among High-Risk Filipino Women With Gestational Diabetes Diagnosed Before and After 24 Weeks of Gestation
DOI:
https://doi.org/10.15605/jafes.037.02.05Keywords:
prenatal screening, diabetes, gestational, pregnancy outcomesAbstract
Objectives. This study determined the prevalence, clinical characteristics and pregnancy outcomes of high-risk women diagnosed with gestational diabetes mellitus (GDM) before and after 24 weeks of gestation.
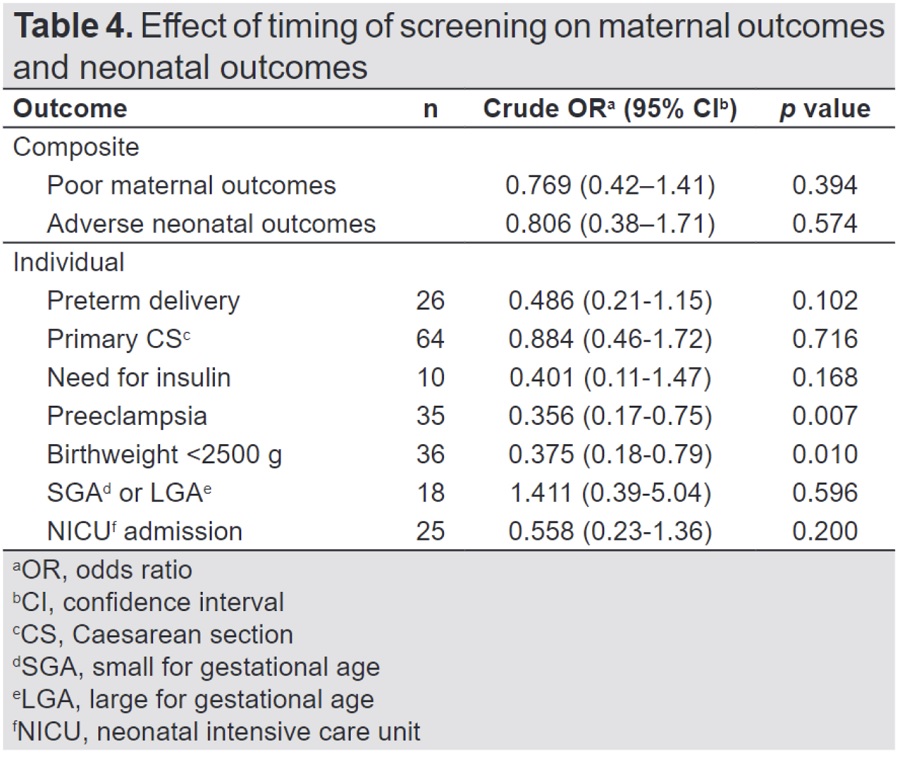
Methodology. This retrospective study included all singleton deliveries with GDM at the Pasig City General Hospital from January 2018 to December 2019. Subjects were grouped into those who were diagnosed with GDM before 24 weeks of gestation (<24 weeks, n=61) and thereafter (≥24 weeks, n=219). Outcomes examined were preeclampsia, cesarean delivery, preterm birth, macrosomia, large-for-gestational age, small-for-gestational age, neonatal hypoglycemia, neonatal ICU admission, congenital malformations and perinatal mortality.
Results. The group diagnosed with GDM before 24 weeks was significantly older (33.0 ± 5.7 years versus 29.4 ± 5.9 years, p<0.001), had higher 2-hour 75 g oral glucose tolerance test (OGTT) results (158.2 ± 20.0 mg/dL versus 150.0 ± 23.7 mg/dL, p=0.014), and had more pregnancies with preeclampsia (23.0% versus 9.6%, p=0.005).
Conclusion. High-risk women diagnosed with GDM before 24 weeks of gestation had a higher incidence of preeclampsia compared with high-risk women diagnosed with GDM after 24 weeks of gestation.
Downloads
References
REFERENCES
Urbanozo H, Isip-Tan IT. Association of gestational diabetes mellitus diagnosed using the IADPSG and the POGS 75 gram oral glucose tolerance test cut-off values with adverse perinatal outcomes in the Philippine General Hospital. J ASEAN Fed Endocr Soc. 2014;29(2):157-62. https://doi.org/10.15605/jafes.029.02.09.
Vandorsten JP, Dodson WC, Espeland MA, et al. National Institutes of Health Consensus Development Conference Statement: Diagnosing gestational diabetes mellitus. NIH Consens State Sci Statements. 2013;29(1):1-31. https://pubmed.ncbi.nlm.nih.gov/23748438.
Berga SL, Nitsche JF, Braunstein GD. Endocrine changes in pregnancy. In: Melmed S, Polonsky KS, Larsen PR, Kronenberg HM. Williams Textbook of Endocrinology E-Book. Elsevier Health Sciences; 2015.
Immanuel J, Simmons D. Screening and treatment for early-onset gestational diabetes mellitus: A systematic review and meta-analysis. Curr Diab Rep . 2017;17,(11):115. https://pubmed.ncbi.nlm.nih.gov/28971305 https://doi.org/10.1007/s11892-017-0943-7.
Jimeno CA, on behalf of the Technical Review Committee of the UNITE for DM Clinical Practice Guidelines on the Diagnosis and Mangement of Diabetes. A summary of the Philippines UNITE for Diabetes Clinical Practice Guidelines for the diagnosis and management of diabetes (Part I: Screening and diagnosis of DM). J ASEAN Fed Endocr Soc. 2011;26(1):26-30. https://doi.org/10.15605/jafes.026.01.05.
Blumer I, Hadar E, Hadden DR, et al. Diabetes and pregnancy: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2013;98(11):4227-49. https://pubmed.ncbi.nlm.nih.gov/24194617. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8998095. https://doi.org/10.1210/jc.2013-2465.
Lim-Uy SW, Cunanan EC, Andag-Silva AA. Prevalence and risk factors of gestational diabetes mellitus at the University of Santo Tomas Hospital. Philipp J Intern Med. 2010;48(1):24-31. Corpus ID: 55627702.
Litonjua AD, Waspadji S, Pheng CS. AFES Study Group on Diabetes in Pregnancy: Preliminary data on prevalence. Philipp J Intern Med. 1996;34(2):67-8.
Plows JF, Stanley JL, Baker PN, Reynolds CM, Vickers MH. The pathophysiology of gestational diabetes mellitus. Int J Mol Sci. 2018;19(11):3342. https://pubmed.ncbi.nlm.nih.gov/30373146. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6274679. https://doi.org/10.3390/ijms19113342.
The HAPO Study Cooperative Research Group. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;358(19):1991-2002. https://pubmed.ncbi.nlm.nih.gov/18463375. https;//doi.org/10.1056/NEJMoa0707943.
Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy: A World Health Organization Guideline. Diabetes Res Clin Pract. 2014;103(3):341-63. https://pubmed.ncbi.nlm.nih.gov/24847517. https://doi.org/10.1016/j.diabres.2013.10.012.
American Diabetes Association. Classification and diagnosis of diabetes. Sec. 2. In Standards of Medical Care in Diabetes—2017. Diabetes Care. 2017;40(Suppl 1):S11-24. https://pubmed.ncbi.nlm.nih.gov/27979889. https://doi.org/10.2337/dc17-S005.
Easmin S, Chowdhury TA, Islam MR, et al. Obstetric outcome in early and late onset gestational diabetes mellitus. Mymensingh Med J. 2015;24(3):450-6. https://pubmed.ncbi.nlm.nih.gov/26329938.
Seth Hawkins J, Lo JY, Casey BM, McIntire DD, Leveno KJ. Diet-treated gestational diabetes mellitus: Comparison of early vs routine diagnosis. Am J Obstet Gynecol. 2008;198(3):287.e1-6. https://pubmed.ncbi.nlm.nih.gov/18313450. https://doi.org/10.1016/j.ajog.2007.11.049.
English FA, Kenny LC, McCarthy FP. Risk factors and effective management of preeclampsia. Integr Blood Press Control. 2015;8:7-12. https://pubmed.ncbi.nlm.nih.gov/25767405. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4354613. https://doi.org/10.2147/IBPC.S50641.
Cundy T, Ackermann E, Ryan EA. Gestational diabetes: New criteria may triple the prevalence but effect on outcomes is unclear. BMJ. 2014;348:g1567. https://pubmed.ncbi.nlm.nih.gov/24618099. https://doi.org/10.1136/bmj.g1567.
Sweeting AN, Ross GP, Hyett J, et al. Gestational diabetes mellitus in early pregnancy: evidence for poor pregnancy outcomes despite treatment. Diabetes Care. 2016;39(1):75-81. https://pubmed.ncbi.nlm.nih.gov/26645084. https://doi.org/10.2337/dc15-0433.
Boriboonhirunsarn D, Kasempipatchai V. Incidence of large for gestational age infants when gestational diabetes mellitus is diagnosed early and late in pregnancy. J Obstet Gynaecol Res. 2016;42(3):273-8. https://pubmed.ncbi.nlm.nih.gov/26694998. https://doi.org/10.1111/jog.12914.
Bartha JL, Martinez-Del-Fresno P, Comino-Delgado R. Gestational diabetes mellitus diagnosed during early pregnancy. Am J Obstet Gynecol. 2000;182(2):346-50. https://pubmed.ncbi.nlm.nih.gov/10694335. https://doi.org/10.1016/s0002-9378(00)70222-5.
Hong WY, Biggio JR, Tita A, Harper LM. Impact of early screening for gestational diabetes on perinatal outcomes in high-risk women. Am J Perinatol. 2016;33(8):758-64. https://pubmed.ncbi.nlm.nih.gov/26890436. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4919164. https://doi.org/10.1055/s-0036-1571317.
Moyer VA, US Preventive Services Task Force. Screening for gestational diabetes mellitus: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160(6):414-20. https://pubmed.ncbi.nlm.nih.gov/24424622. https://doi.org/10.7326/M13-2905.
Palatnik A, Mele L, Landon MB, et al. Timing of treatment initiation for mild gestational diabetes mellitus and perinatal outcomes. Am J Obstet Gynecol. 2015;213(4):560.e1-8. https://pubmed.ncbi.nlm.nih.gov/26071920. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4609640. https://doi.org/10.1016/j.ajog.2015.06.022.
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 KRISELLE RAE DY, CHRISTY YAO

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The full license is at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.










