Detection of Hemostasis Abnormalities in Type 2 Diabetes Mellitus Using Thromboelastography
DOI:
https://doi.org/10.15605/jafes.037.02.12Keywords:
diabetes mellitus, thromboelastography, hemostasisAbstract
Introduction. Type 2 DM (T2DM) is associated with inflammation and vascular dysfunction which impact hemostasis. Thromboelastography (TEG) as a hemostasis assessment method, is not routinely applied in T2DM.
Methodology. A cross-sectional study was conducted among T2DM patients attending the Endocrinology Clinic of Saiful Anwar Hospital, Indonesia. Glycemic profiles were determined using fasting plasma glucose (FPG), 2-hour postprandial plasma glucose (2hPPG), and glycosylated hemoglobin (HbA1c). Therapy for T2DM was classified into insulin and non-insulin regimens. The primary and secondary hemostasis profile were examined using TEG and was classified as hypo- hyper- and normo-
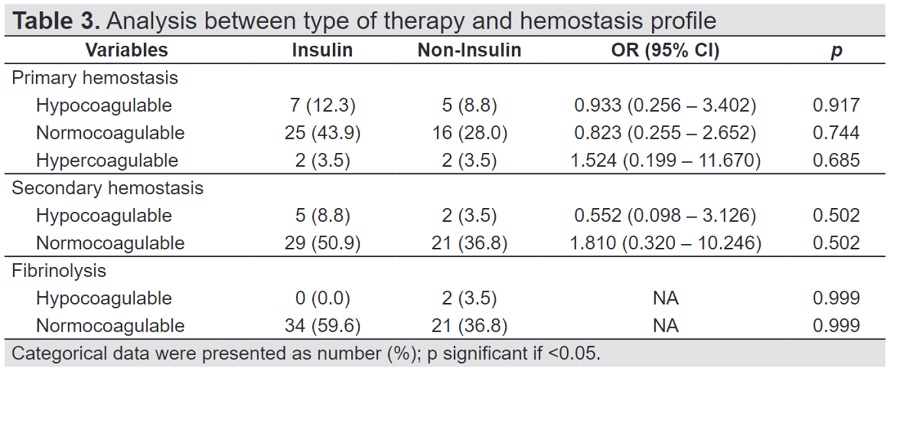
Result. A total of 57 T2DM patients were included. Kruskal-Wallis test did not reveal a significant association between glycemic profiles and groups of hemostasis. However, the median HbA1c was higher in the hypercoagulable group of primary hemostasis and fibrinolysis. The median FPG and 2hPPG were higher in the normo-coagulable group of secondary hemostasis. Logistic regression did not indicate a significant association between type of therapy for diabetes and hemostasis profile.
Conclusion. This study did not find significant associations between glycemic levels and type of DM therapy with hemostasis profiles using the TEG method in patients with T2DM.
Downloads
References
Ajjan, RA, Grant PJ. Hemostatic abnormalities in diabetes mellitus. International Textbook of Diabetes Mellitus, 4th ed, chapter 72. USA: John Wiley & Sons, Ltd.; 2015.
Calles-Escandon J, Cipolla M. Diabetes and endothelial dysfunction: A clinical perspective. Endocr Rev. 2001; 22(1):36–52. https://pubmed.ncbi.nlm.nih.gov/11159815. https://doi.org/10.1210/edrv.22.1.0417.
Lemkes BA, Hermanides J, Devries JH, Holleman F, Meijers JCM, Hoekstra JBL. Hyperglycemia: A prothrombotic factor? J Thromb Haemost. 2010;8(8):1663–9. https://pubmed.ncbi.nlm.nih.gov/20492456. https://doi.org/10.1111/j.1538-7836.2010.03910.x.
Verma M, Paneri S, Badi P, Raman PG. Effect of increasing duration of diabetes mellitus type 2 on glycated hemoglobin and insulin sensitivity. Indian J Clin Biochem. 2006;21(1):142-6. https://pubmed.ncbi.nlm.nih.gov/23105586. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3453763. https://doi.org/10.1007/BF02913083.
Vazzana N, Ranalli P, Cuccurullo C, Davì G. Diabetes mellitus and thrombosis. Thromb Res. 2012;129(3):371-7. https://pubmed.ncbi.nlm.nih.gov/22197180. https://doi.org/10.1016/j.thromres.2011.11.052.
Osende JI, Badimon JJ, Fuster V, et al. Blood thrombogenicity in type 2 diabetes mellitus patients is associated with glycemic control. J Am Coll Cardiol. 2001;38(5): 1307–12. https://pubmed.ncbi.nlm.nih.gov/11691500. https://doi.org/10.1016/s0735-1097(01)01555-8.
Yürekli BPS, Ozcebe OI, Kirazli S, Gürlek A. Global assessment of the coagulation status in type 2 diabetes mellitus using rotation thromboelastography. Blood Coagul Fibrinolysis. 2006;17(7):545-9. https://pubmed.ncbi.nlm.nih.gov/16988549. https://doi.org/10.1097/01.mbc.0000245292.34150.df.
Hartmann J, Mason D, Achneck H. Thromboelastography (TEG) point-of-care diagnostic for hemostasis management. Point of Care. 2018;17(1):15-22. https://doi.org/10.1097/POC.0000000000000156.
Bolliger D, Seeberger MD, Tanaka KA. Principles and practice of thromboelastography in clinical coagulation management and transfusion practice. Transfus Med Rev. 2012;26(1):1-13. https://pubmed.ncbi.nlm.nih.gov/21872428. https://doi.org/10.1016/j.tmrv.2011.07.005.
Subramanian A, Albert V, Agrawal D, Saxena R, Pandey RM. Evaluation of the utility of thromboelastography in a tertiary trauma care centre. ISRN Hematol. 2014;2014:849626. https://pubmed.ncbi.nlm.nih.gov/24695847. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3947774. https://doi.org/10.1155/2014/849626.
Rocha LL, Pessoa CMS, Neto AS, et al. Thromboelastometry versus standard coagulation tests versus restrictive protocol to guide blood transfusion prior to central venous catheterization in cirrhosis: Study protocol for a randomized controlled trial. Trials. 2017;18(1):85. https://pubmed.ncbi.nlm.nih.gov/28241780. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5327508. https://doi.org/10.1186/s13063-017-1835-5.
Pretorius L, Thomson GJA, Adams RCM, Nell TA, Laubscher WA, Pretorius E. Platelet activity and hypercoagulation in type 2 diabetes. Cardiovasc Diabetol. 2018;17(1):141. https://pubmed.ncbi.nlm.nih.gov/30388964. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6214175. https://doi.org/10.1186/s12933-018-0783-z.
Collins S, MacIntyre C, Hewer I. Thromboelastography: Clinical application, interpretation, and transfusion management. AANA J. 2016;84(2):129-34. https://pubmed.ncbi.nlm.nih.gov/27311154.
Walker CB, Moore HB, Nydam TL, et al. The use of thromboelastography to assess post-operative changes in coagulation and predict graft function in renal transplantation. Am J Surg. 2020;220(6):1511-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7450953. https://doi.org/10.1016/j.amjsurg.2020.08.019.
Kim SM, Kim SI, Yu G, et al. Role of thromboelastography as an early predictor of disseminated intravascular coagulation in patients with septic shock. J Clin Med. 2020;9(12):3883. https://pubmed.ncbi.nlm.nih.gov/33260354. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7760761. https://doi.org/10.3390/jcm9123883.
Wang D, Liu Y, Chen Z, et al. Impact of diabetes mellitus on coagulation function before and after off-pump coronary artery bypass grafting. J Thorac Dis. 2019;11(12):5517-26. https://pubmed.ncbi.nlm.nih.gov/32030271. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6988029. https://doi.org/10.21037/jtd.2019.11.27.
Ligita T, Wicking K, Francis K, Harvey N, Nurjannah I. How people living with diabetes in Indonesia learn about their disease: A grounded theory study. PLOS One. 2019;14(2): e0212019. https://pubmed.ncbi.nlm.nih.gov/30794570. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6386238. https://doi.org/10.1371/journal.pone.0212019.
Asrat D, Tesyafe G, Gedefaw L, Wondimagegn A, Yemane T. Hemostatic abnormality and associated factors in diabetic patients at Jimma University Specialized Hospital, Jimma, Southwest Ethiopia: A comparative cross-sectional study. Ethiop J Health Sci. 2019;29(2):251-8. https://pubmed.ncbi.nlm.nih.gov/31011273. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6460446. https://doi.org/10.4314/ejhs.v29i2.12.
Palta S, Saroa R, Palta A. Overview of the coagulation system. Indian J Anaesth. 2014;58(5):515-24. https://pubmed.ncbi.nlm.nih.gov/25535411. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4260295. https://doi.org/10.4103/0019-5049.144643.
Maatman BT, Schmeisser G, Kreutz RP. Fibrin clot strength in patients with diabetes mellitus measured by thromboelastography. J Diabetes Res. 2018;2018:4543065. https://pubmed.ncbi.nlm.nih.gov/29507861. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5817329. https://doi.org/10.1155/2018/4543065.
Ma Q, Wen X, Wang Q, Xue Y, Huang L. Effect of exogenous insulin on platelet reactivity in patients with acute ischemic vascular events. Authorea. 2020. https://doi.org/10.22541/au.159050015.53627920.
Boden G, Rao AK. Effects of hyperglycemia and hyperinsulinemia on the tissue factor pathway of blood coagulation. Curr Diab Rep. 2007;7(3):223-7. https://pubmed.ncbi.nlm.nih.gov/17547839. https://doi.org/10.1007/s11892-007-0035-1.
Gresele P, Guglielmini G, De Angelis M, et al. Acute, short-term hyperglycemia enhances shear stress-induced platelet activation in patients with type II diabetes mellitus. J Am Coll Cardiol. 2003;41(6):1013–20. https://pubmed.ncbi.nlm.nih.gov/12651051. https://doi.org/10.1016/s0735-1097(02)02972-8.
Stegenga ME, van der Crabben SN, Dessing MC, et al. Effect of acute hyperglycaemia and/or hyperinsulinaemia on proinflammatory gene expression, cytokine production and neutrophil function in humans. Diabet Med. 2008;25(2): 157–64. https://pubmed.ncbi.nlm.nih.gov/18290856. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2268957. https://doi.org10.1111/j.1464-5491.2007.02348.x.
Boden G, Vaidyula VR, Homko C, Cheung P, Rao AK. Circulating tissue factor procoagulant activity and thrombin generation in patients with type 2 diabetes: Effects of insulin and glucose. J Clin Endocrinol Metab. 2007;92(11):4352–8. https://pubmed.ncbi.nlm.nih.gov/17785358. https://doi.org/10.1210/jc.2007-0933.
Undas A, Wiek I, Stêpien E, Tracz W. Hyperglycemia is associated with enhanced thrombin formation, platelet activation, and fibrin clot resistance to lysis in patients with acute coronary syndrome. Diabetes Care. 2008;31(8):1590–5. https://pubmed.ncbi.nlm.nih.gov/18487475. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2494657. https://doi.org/10.2337/dc08-0282.
Angiolillo DJ, Bernardo E, Ramírez C, et al. Insulin therapy is associated with platelet dysfunction in patients with type 2 diabetes mellitus on dual oral antiplatelet treatment. J Am Coll Cardiol. 2006;48(2):298–304. https://pubmed.ncbi.nlm.nih.gov/16843179. https://doi.org/10.1016/j.jacc.2006.03.038.
Lam H, Katyal N, Parker C, et al. Thromboelastography with platelet mapping is not an effective measure of platelet inhibition in patients with spontaneous intracerebral hemorrhage on antiplatelet therapy. Cureus. 2018;10(4):e2515. https://pubmed.ncbi.nlm.nih.gov/29942718. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6015994. https://doi.org/10.7759/cureus.2515.
Ferreira IA, Mocking AIM, Feijge MAH, et al. Platelet inhibition by insulin is absent in type 2 diabetes mellitus. Arterioscler Thromb Vasc Biol. 2006;26(2):417–22. https://pubmed.ncbi.nlm.nih.gov/16339499. https://doi.org/10.1161/01.ATV.0000199519.37089.a0.
Vaidyula VR, Rao AK, Mozzoli M, Homko C, Cheung P, Boden G. Effects of hyperglycemia and hyperinsulinemia on circulating tissue factor procoagulant activity and platelet CD40 ligand. Diabetes. 2006;55(1):202–8. https://pubmed.ncbi.nlm.nih.gov/16380494.
Nakamura T, Ako J, Kadowaki T, et al. Impact of acute hyperglycemia during primary stent implantation in patients with ST-elevation myocardial infarction. J Cardiol. 2009;53(2):272–7. https://pubmed.ncbi.nlm.nih.gov/19304133. https://doi.org/10.1016/j.jjcc.2008.11.011.
Timmer JR, van der Horst ICC, Ottervanger JP, et al. Prognostic value of admission glucose in non-diabetic patients with myocardial infarction. Am Heart J. 2004;148(3):399–404. https://pubmed.ncbi.nlm.nih.gov/15389225. https://doi.org/10.1016/j.ahj.2004.04.007.
Kosiborod M, Rathore SS, Inzucchi SE, et al. Admission glucose and mortality in elderly patients hospitalized with acute myocardial infarction: Implications for patients with and without recognized diabetes. Circulation. 2005;111(23):3078–86. https://pubmed.ncbi.nlm.nih.gov/15939812. https://doi.org/10.1161/CIRCULATIONAHA.104.517839.
Xie X, Wang M, Lu Y, et al. Thromboelastography (TEG) in normal pregnancy and its diagnostic efficacy in patients with gestational hypertension, gestational diabetes mellitus, or preeclampsia. J Clin Lab Anal. 2021;35(2):e23623. https://pubmed.ncbi.nlm.nih.gov/33067885. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7891543. https://doi.org/10.1002/jcla.23623.
Rao AK, Chouhan V, Chen X, Sun L, Boden G. Activation of the tissue factor pathway of blood coagulation during prolonged hyperglycemia in young healthy men. Diabetes. 1999;48(5):1156–61. https://pubmed.ncbi.nlm.nih.gov/10331423. https://doi.org/ 10.2337/diabetes.48.5.1156.
Nieuwdorp M, van Haeften TW, Gouverneur MC, et al. Loss of endothelial glycocalyx during acute hyperglycemia coincides with endothelial dysfunction and coagulation activation in vivo. Diabetes. 2006;55(2):480–6. https://pubmed.ncbi.nlm.nih.gov/16443784. https://doi.org/10.2337/diabetes.55.02.06.db05-1103.
Iwasaki Y, Kambayashi M, Asai M, Yoshida M, Nigawara T, Hashimoto K. High glucose alone, as well as in combination with proinflammatory cytokines, stimulates nuclear factor kappa-B-mediated transcription in hepatocytes in vitro. J Diabetes Complications 2007;21(1):56–62. https://pubmed.ncbi.nlm.nih.gov/17189875. https://doi.org/10.1016/j.jdiacomp.2006.02.001.
Wieczór R, Wieczór AM, Kulwas A, Rość D. Type 2 diabetes and cardiovascular factors contrasted with fibrinolysis disorders in the blood of patients with peripheral arterial disease. Medicina (Kaunas). 2019;55(7):395. https://pubmed.ncbi.nlm.nih.gov/31336615. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6681256. https://doi.org/10.3390/medicina55070395.
Bryk AH, Konieczynska M, Rostoff P, et al. Plasma protein oxidation as a determinant of impaired fibrinolysis in type 2 diabetes. Thromb Haemost. 2018;119(2):213-22. https://pubmed.ncbi.nlm.nih.gov/30605917. https://doi.org/10.1055/s-0038-1676609.
Alzahrani SH, Ajjan RA. Coagulation and fibrinolysis in diabetes. Diab Vasc Dis Res. 2010;7(4):260–73. https://pubmed.ncbi.nlm.nih.gov/20847109. https://doi.org/10.1177/1479164110383723.
Ribo M, Molina C, Montaner J, et al. Acute hyperglycemia state is associated with lower tPA-induced recanalization rates in stroke patients. Stroke. 2005;36(8):1705–9. https://pubmed.ncbi.nlm.nih.gov/16002761. https://doi.org/10.1161/01.STR.0000173161.05453.90.9f.
Margolis DJ, Hoffstad O, Strom BL. Association between serious ischemic cardiac outcomes and medications used to treat diabetes. Pharmacoepidemiol Drug Saf. 2008;17(8):753–9. https://pubmed.ncbi.nlm.nih.gov/18613215. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2635115. https://doi.org/10.1002/pds.1630
Standeven KF, Ariens RA, Whitaker P, Ashcroft AE, Weisel JW. Grant PJ. The effect of dimethylbiguanide on thrombin activity, FXIII activation, fibrin polymerization, and fibrin clot formation. Diabetes. 2002;51(1):189–97. https://pubmed.ncbi.nlm.nih.gov/11756340. https://doi.org/10.2337/diabetes.51.1.189.
Buckingham RE. Thiazolidinediones: Pleiotropic drugs with potent anti-inflammatory properties for tissue protection. Hepatol Res. 2005;33(2):167–70. https://pubmed.ncbi.nlm.nih.gov/16198619. https://doi.org/10.1016/j.hepres.2005.09.027.
Cefalu WT, Schneider DJ, Carlson HE, et al. Effect of combination glipizide GITS/metformin on fibrinolytic and metabolic parameters in poorly controlled type 2 diabetic subjects. Diabetes Care. 2002;25(1):2123-8. https://pubmed.ncbi.nlm.nih.gov/12453948. https://doi.org/10.1016/j.diabres.2008.02.006.
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Putu Moda Arsana, Novi Khila Firani, Siti Fatonah, Affa Kiysa Waafi, Adinda Dian Novitasari

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The full license is at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.










