The Role of Triglyceride-Glucose Index in the Prediction of the Development of Hypertension
Findings from a Community Cohort in Singapore
DOI:
https://doi.org/10.15605/jafes.038.01.09Keywords:
Diabetes Mellitus, Type 2, Triglycerides, Hypertension, Screening, Population ScienceAbstract
Objectives. Triglyceride-glucose index (TyGI) is an emerging surrogate marker of insulin resistance. We aim to explore the role of triglyceride-glucose index in the prediction of the development of hypertension.
Methodology. We conducted a retrospective cohort study that included 3,183 study participants identified from a community health screening programme who had no baseline hypertension and were then followed up after an average of 1.7 years. Cox proportional-hazard model was used to assess the association between risk of incident hypertension and TyGI in quartiles, while adjusting for demographics and clinical characteristics.
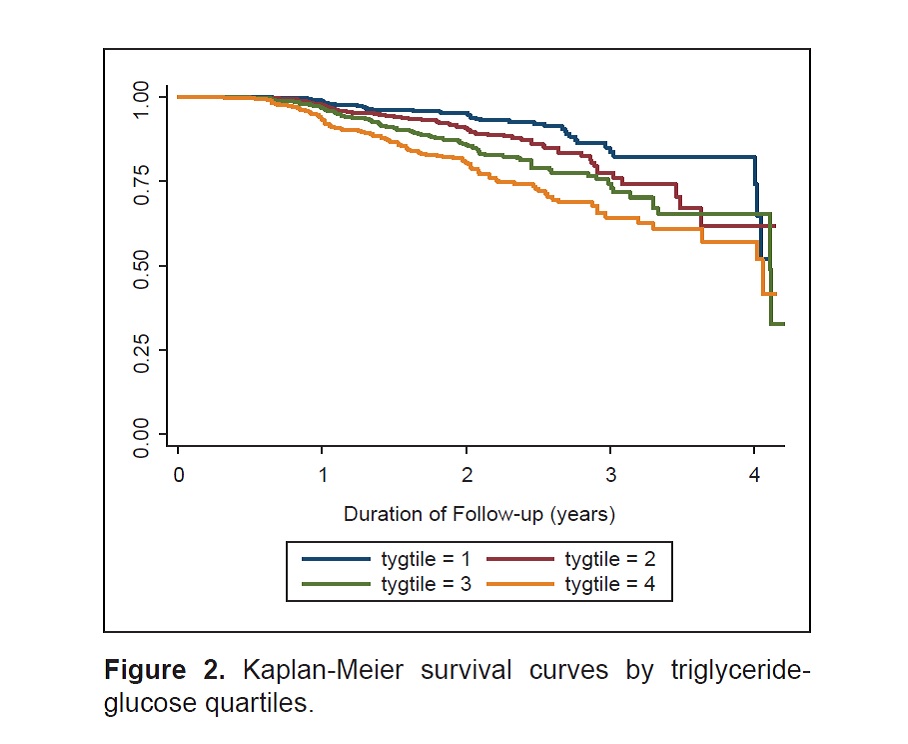
Results. Hypertension occurred in 363 study participants (11.4%). Those who developed hypertension had higher TyGI [8.6 (IQR 8.2-9.0)] than those who did not [8.2 (IQR 8.0-8.7)] (p<0.001). Significant association between TyGI and hypertension was observed in both the unadjusted and proportional hazard model [Quartile (Q)2, p=0.010; Q3, p<0.001 and Q4, p<0.001] and the model that adjusted for demographics (Q2, p=0.016; Q3, p=0.003; Q4, p<0.001). In the model adjusted for clinical covariates, the hazard of developing hypertension remained higher in TyGI Q4 compared to TyGI Q1(Hazard Ratio=2.57; 95% Confidence Interval: 1.71, 3.87). Increasing triglyceride-glucose index accounted for 16.4% of the association between increasing BMI and incident hypertension, after adjusting for age, gender, ethnicity and baseline HDL cholesterol (p<0.001).
Conclusion. Triglyceride-glucose index was an independent predictor of the development of hypertension. It may potentially be used as an inexpensive indicator to predict the development of hypertension and risk-stratify individuals to aid management in clinical practice.
Downloads
References
Leiba A, Twig G, Levine H, et al. Hypertension in late adolescence and cardiovascular mortality in midlife: A cohort study of 2.3 million 16- to 19-year-old examinees. Pediatr Nephrol. 2016;31(3):485-92. MID: 26508439. https://doi.org/10.1007/s00467-015-3240-1.
Lotfaliany M, Akbarpour S, Mozafary A, Boloukat RR, Azizi F, Hadaegh F. Hypertension phenotypes and incident cardiovascular disease and mortality events in a decade follow-up of a Middle East cohort. J Hypertens. 2015;33(6):1153-61. https://pubmed.ncbi.nlm.nih.gov/25699976. https://doi.org/10.1097/HJH.0000000000000540.
Robitaille C, Dai S, Waters C, et al. Diagnosed hypertension in Canada: Incidence, prevalence and associated mortality. CMAJ. 2012;184(1):E49-56. https://pubmed.ncbi.nlm.nih.gov/22105752. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3255225. https://doi.org/10.1503/cmaj.101863.
Zheng R, Mao Y. Triglyceride and glucose (TyG) index as a predictor of incident hypertension: A 9-year longitudinal population-based study. Lipids Health Dis. 2017;16(1):175. https://pubmed.ncbi.nlm.nih.gov/28903774. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5598027. https://doi.org/10.1186/s12944-017-0562-y.
Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: A systematic analysis of population-based studies from 90 countries. Circulation. 2016;134(6):441-50. https://pubmed.ncbi.nlm.nih.gov/27502908. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4979614. https://doi.org/10.1161/CIRCULATIONAHA.115.018912.
Jian S, Su-Mei N, Xue C, Jie Z, Xue-Sen W. Association and interaction between triglyceride-glucose index and obesity on risk of hypertension in middle-aged and elderly adults. Clin Exp Hypertens. 2017;39(8):732-9. https://pubmed.ncbi.nlm.nih.gov/28737433. https://doi.org/10.1080/10641963.2017.1324477.
Lytsy P, Ingelsson E, Lind L, Arnlöv J, Sundström J. Interplay of overweight and insulin resistance on hypertension development. J Hypertens. 2014;32(4):834-9. https://pubmed.ncbi.nlm.nih.gov/24370898. https://doi.org/10.1097/HJH.0000000000000081.
Zhang M, Wang B, Liu Y, et al. Cumulative increased risk of incident type 2 diabetes mellitus with increasing triglyceride glucose index in normal-weight people: The rural Chinese cohort study. Cardiovasc Diabetol. 2017;16(1):30. https://pubmed.ncbi.nlm.nih.gov/28249577. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5333419. https://doi.org/10.1186/s12933-017-0514-x.
Du T, Yuan G, Zhang M, Zhou X, Sun X, Yu X. Clinical usefulness of lipid ratios, visceral adiposity indicators, and the triglycerides and glucose index as risk markers of insulin resistance. Cardiovasc Diabetol. 2014;13:146. https://pubmed.ncbi.nlm.nih.gov/25326814. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4209231. https://doi.org/10.1186/s12933-014-0146-3.
Navarro- González D, Sánchez-Íñigo L, Pastrana-Delgado J, Fernández-Montero A, Martinez JA. Triglyceride-glucose index (TyG index) in comparison with fasting plasma glucose improved diabetes prediction in patients with normal fasting glucose: The Vascular-Metabolic CUN cohort. Prev Med. 2016;86:99-105. https://pubmed.ncbi.nlm.nih.gov/26854766. https://doi.org/10.1016/j.ypmed.2016.01.022.
Guerrero-Romero F, Simental-Mendía LE, González-Ortiz M, et al. The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic-hyperinsulinemic clamp. J Clin Endocrinol Metab. 2010;95(7):3347-51. https://pubmed.ncbi.nlm.nih.gov/20484475. https://doi.org/10.1210/jc.2010-0288.
Simental-Mendía LE, Rodríguez-Morán M, Guerrero-Romero F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab Syndr Relat Disord. 2008;6(4):299-304. https://pubmed.ncbi.nlm.nih.gov/19067533. https://doi.org/10.1089/met.2008.0034.
Vasques AC, Novaes FS, de Oliveira Mda S, et al. TyG index performs better than HOMA in a Brazilian population: A hyperglycemic clamp validated study. Diabetes Res Clin Pract. 2011;93(3):e98-100. https://pubmed.ncbi.nlm.nih.gov/21665314. https://doi.org/10.1016/j.diabres.2011.05.030.
Wan K, Zhao J, Huang H, et al. The association between triglyceride/high-density lipoprotein cholesterol ratio and all-cause mortality in acute coronary syndrome after coronary revascularization. PloS One. 2015;10(4):e0123521. https://pubmed.ncbi.nlm.nih.gov/25880982. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4399840. https://doi.org/10.1371/journal.pone.0123521.
Lee DY, Lee ES, Kim JH, et al. Predictive value of triglyceride glucose index for the risk of incident diabetes: A 4-year retrospective longitudinal study. PloS One. 2016;11(9):e0163465. https://pubmed.ncbi.nlm.nih.gov/27682598. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5040250. https://doi.org/10.1371/journal.pone.0163465.
Lee SH, Kwon HS, Park YM, et al. Predicting the development of diabetes using the product of triglycerides and glucose: The Chungju Metabolic Disease Cohort (CMC) study. PloS One. 2014;9(2):e90430. https://pubmed.ncbi.nlm.nih.gov/24587359. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3938726. https://doi.org/10.1371/journal.pone.0090430.
Low S, Khoo KCJ, Irwan B, et al. The role of triglyceride glucose index in development of type 2 diabetes mellitus. Diabetes Res Clin Pract. 2018;143:43-9. https://pubmed.ncbi.nlm.nih.gov/29936253. https://doi.org/10.1016/j.diabres.2018.06.006.
Sánchez-Íñigo L, Navarro-González D, Pastrana-Delgado J, Fernández-Montero A, Martínez JA. Association of triglycerides and new lipid markers with the incidence of hypertension in a Spanish cohort. J Hypertens. 2016;34(7):1257-65. https://pubmed.ncbi.nlm.nih.gov/27136314. https://doi.org/10.1097/HJH.0000000000000941.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499-502. https://pubmed.ncbi.nlm.nih.gov/4337382.
Roche. Glucose HK Gen.3: Cobas®. Mannheim, Germany, Roche Diagnostics GmbH; 2016.
Roche. Triglycerides: Cobas®. Mannheim, Germany, Roche Diagnostics GmbH; 2016.
Roche. HDL-Cholesterol plus 3rd generation: Cobas®. Mannheim, Germany, Rocher Diagnostics GmbH; 2016.
1999 World Health Organization-International Society of Hypertension Guidelines for the Management of Hypertension. Guidelines Subcommittee. J Hypertens. 1999;17(2):151-83. https://pubmed.ncbi.nlm.nih.gov/10067786.
Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173-82. https://pubmed.ncbi.nlm.nih.gov/3806354. https://doi.org/10.1037//0022-3514.51.6.1173.
Nagai M, Kamide K, Rakugi H, et al. Role of endothelin-1 induced by insulin in the regulation of vascular cell growth. Am J Hypertens. 2003;16(3):223-8. https://pubmed.ncbi.nlm.nih.gov/12620701. https://doi.org/10.1016/s0895-7061(02)03251-x.
Tack CJ, Smits P, Willemsen JJ, Lenders JW, Thien T, Lutterman JA. Effects of insulin on vascular tone and sympathetic nervous system in NIDDM. Diabetes. 1996;45(1):15-22. https://pubmed.ncbi.nlm.nih.gov/8522054. https://doi.org/10.2337/diab.45.1.15.
Takagi M, Tanaka Y, Yamasaki Y, et al. Responsiveness of insulin-induced cardiac sympathetic nerve activation associates with blood pressure regulation in diabetics. Am J Physiol Endocrinol Metab. 2003;284(5):E1022-6. https://pubmed.ncbi.nlm.nih.gov/12569084. https://doi.org/10.1152/ajpendo.00169.2002.
Thackeray JT, Radziuk J, Harper ME, et al. Sympathetic nervous dysregulation in the absence of systolic left ventricular dysfunction in a rat model of insulin resistance with hyperglycemia. Cardiovasc Diabetolol. 2011;10:75. https://pubmed.ncbi.nlm.nih.gov/21831292. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3170183. https://doi.org/10.1186/1475-2840-10-75.
Axelrod L. Insulin, prostaglandins, and the pathogenesis of hypertension. Diabetes. 1991;40(10):1223-7. https://pubmed.ncbi.nlm.nih.gov/1936584. https://doi.org/10.2337/diab.40.10.1223.
Frank HJ, Levin ER, Hu RM, Pedram A. Insulin stimulates endothelin binding and action on cultured vascular smooth muscle cells. Endocrinology. 1993;133(3):1092-7. https://pubmed.ncbi.nlm.nih.gov/8365355. https://doi.org/10.1210/endo.133.3.8365355.
Saitoh S. [Insulin resistance and renin-angiotensin-aldosterone system]. Nihon Rinsho. 2009;67(4):729-34. https://pubmed.ncbi.nlm.nih.gov/19348235.
Soleimani M. Insulin resistance and hypertension: New insights. Kidney Int. 2015;87(3):497-9. https://pubmed.ncbi.nlm.nih.gov/25723632. https://doi.org/10.1038/ki.2014.392.
Zemel MB. Insulin resistance vs. hyperinsulinemia in hypertension: Insulin regulation of Ca2+ transport and Ca(2+)-regulation of insulin sensitivity. J Nutr. 1995;125(6 Suppl):1738s-43s. https://pubmed.ncbi.nlm.nih.gov/7782937. https://doi.org/10.1093/jn/125.suppl_6.1738S.
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Jonathon Khoo, Serena Low, Bastari Irwan, Justin Tang, Chee Fang Sum, Tavintharan Subramaniam, Su Chi Lim

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The full license is at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.










