Fatal Case of Possible Thyroid Crisis Induced by SARS-CoV-2 Infection
A Case Report
DOI:
https://doi.org/10.15605/jafes.037.02.19Keywords:
COVID-19, SARS-CoV-2, thyrotoxic crisis, thryoid storm, thyrotoxicosisAbstract
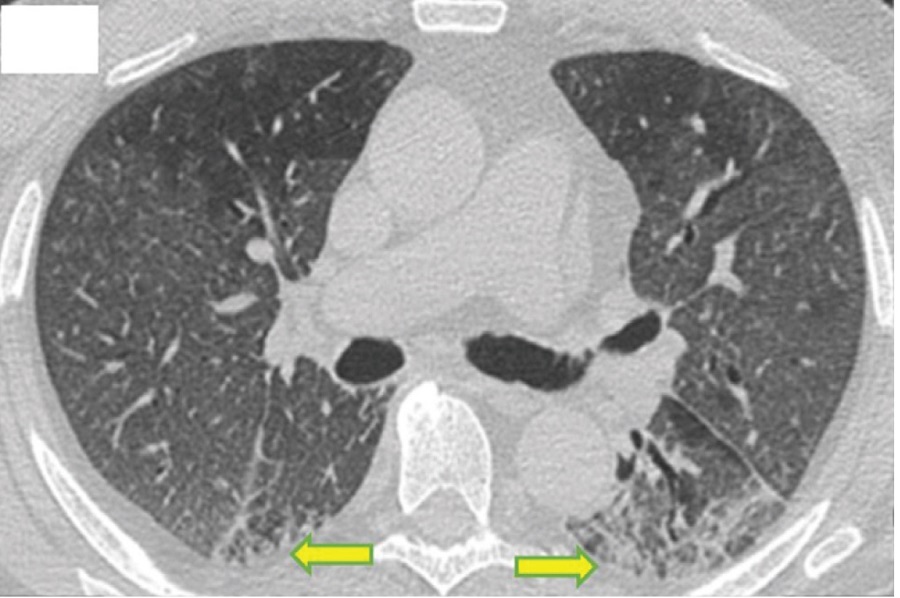
Thyroid crisis is an emergency due to impaired thyroid function caused by various conditions, particularly infections such as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that result in the dysfunction of various vital organs. We report a case of a 31-year-old Indonesian female with a 2-year history of hyperthyroidism with elevated thyroid-stimulating hormone (TSH) receptor antibodies. (TRAb) who developed thyroid crisis possibly in association with SARS-CoV-2 pneumonia, sepsis, and disseminated intravascular coagulation (DIC). Prior to admission, she was treated for her hyperthyroidism with propylthiouracil and had been in stable remission for a year. She was admitted to the Emergency Room with complaints of watery stools, icteric sclerae, jaundice, coughing, and shortness of breath. The physical examination showed a World Health Organization (WHO) performance score of 4, delirium, blood pressure within normal limits, tachycardia, tachypnea, axillary temperature of 36.7°C, icteric sclerae, jaundice, and exophthalmos. There was a 3 cm palpable nodule on the right side of the neck. Auscultation of the lungs revealed bilateral pulmonary rales. Abdominal examination noted a palpable liver and enlarged spleen. Laboratory tests showed thrombocytopenia, electrolyte imbalance, hypoalbuminemia and elevated transaminases. The thyroid function tests showed a suppressed TSH level with an elevated free thyroxine (FT4) level. The SARS-CoV-2 polymerase chain reaction (PCR) swab test was positive. Initial patient management was with supportive therapy that included favipiravir and anti-hyperthyroidism medication; however, despite these interventions, her condition continued to deteriorate and she died after a few hours. This case demonstrates no difference in therapy between patients with thyroid crises and COVID-19 or other infections. Proper and timely treatment is important for reducing mortality rates.
Downloads
References
Pranasakti ME, Talirasa N, Rasena HA, Purwanto RY, Anwar SL. Thyrotoxicosis occurrence in SARS-CoV-2 infection: A case report. Ann Med Surg. 2022;78:103700. doi:10.1016/j.amsu.2022.103700
McDougall IR. Hyperthyroidism. In: McDougall IR, ed. Thyroid Disease in Clinical Practice. Springer US; 1992:82-162. doi:10.1007/978-1-4899-2881-8_5
Satoh T, Isozaki O, Suzuki A, et al. 2016 Guidelines for the management of thyroid storm from The Japan Thyroid Association and Japan Endocrine Society (First edition). Endocr J. 2016;63(12):1025-1064. doi:10.1507/endocrj.EJ16-0336
Oley MH, Oley MC, Kepel BJ, et al. ICAM-1 levels in patients with covid-19 with diabetic foot ulcers: A prospective study in southeast asia. Ann Med Surg. 2021;63:102171. doi:10.1016/j.amsu.2021.02.017
Inaba H, Aizawa T. Coronavirus Disease 2019 and the Thyroid - Progress and Perspectives. Front Endocrinol (Lausanne). 2021;12(June):1-10. doi:10.3389/fendo.2021.708333
Lisco G, De Tullio A, Jirillo E, et al. Thyroid and COVID-19: a review on pathophysiological, clinical and organizational aspects. J Endocrinol Invest. 2021;44(9):1801-1814. doi:10.1007/s40618-021-01554-z
Duntas LH, Jonklaas J. COVID-19 and Thyroid Diseases: A Bidirectional Impact. J Endocr Soc. 2021;5(8):1-11. doi:10.1210/jendso/bvab076
Garcia ML, Szuman G, Scoscia MF, Bacigaluppi S, Panebianco MV, Rella N. The challenge of diagnosing thyroid storm: a comparison of the Japanese Thyroid Association Criteria to de Burch Wartofsky Point Scale. Endocr Abstr. Published online May 3, 2017. doi:10.1530/endoabs.49.EP1251
Akamizu T. Thyroid Storm: A Japanese Perspective. Thyroid. 2018;28(1):32-40. doi:10.1089/thy.2017.0243
Chen M, Zhou W, Xu W. Thyroid Function Analysis in 50 Patients with COVID-19: A Retrospective Study. Thyroid. 2021;31(1):8-11. doi:10.1089/thy.2020.0363
Ross DS, Burch HB, Cooper DS, et al. 2016 American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis. Thyroid. 2016;26(10):1343-1421. doi:10.1089/thy.2016.0229
Lania A, Sandri MT, Cellini M, Mirani M, Lavezzi E, Mazziotti G. Thyrotoxicosis in patients with COVID-19: the THYRCOV study. Eur J Endocrinol. 2020;183(4):381-387. doi:10.1530/EJE-20-0335
Croce L, Gangemi D, Ancona G, et al. The cytokine storm and thyroid hormone changes in COVID-19. J Endocrinol Invest. 2021;44(5):891-904. doi:10.1007/s40618-021-01506-7
Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181-1247. doi:10.1007/s00134-021-06506-y
Amin Akbarzadeh M, Mohammad-Salar H. Hepatobiliary involvement in COVID-19 patients. Bionatura. 2021;6(2):1681-1682. doi:10.21931/RB/2021.06.02.3
Hayat MH, Moazzam Z, Ziogas IA, Yousaf A, Hayat M. Thyroid Storm Presenting as Acute Liver Failure in a Patient with Graves’ Disease. Cureus. 2020;12(9):e10333. doi:10.7759/cureus.10333
Ali A, Mostafa W, Fernandez C, Ahmad H, Htwe N. Apathetic Thyroid Storm with Cardiorespiratory Failure, Pulmonary Embolism, and Coagulopathy in a Young Male with Graves’ Disease and Myopathy. Case Rep Endocrinol. 2020;2020:1-9. doi:10.1155/2020/8896777
Eljilany I, Elzouki A-N. D-Dimer, Fibrinogen, and IL-6 in COVID-19 Patients with Suspected Venous Thromboembolism: A Narrative Review. Vasc Health Risk Manag. 2020;Volume 16:455-462. doi:10.2147/VHRM.S280962
Asakura H, Ogawa H. COVID-19-associated coagulopathy and disseminated intravascular coagulation. Int J Hematol. 2021;113(1):45-57. doi:10.1007/s12185-020-03029-y
Thachil J, Tang N, Gando S, et al. ISTH interim guidance on recognition and management of coagulopathy in COVID‐19. J Thromb Haemost. 2020;18(5):1023-1026. doi:10.1111/jth.14810
Lavon O, Tamir T. Evaluation of the Padua Prediction Score ability to predict venous thromboembolism in Israeli non-surgical hospitalized patients using electronic medical records. Sci Rep. 2022;12(1):6121. doi:10.1038/s41598-022-10209-9
Arpaia GG, Caleffi A, Marano G, et al. Padua prediction score and IMPROVE score do predict in-hospital mortality in Internal Medicine patients. Intern Emerg Med. 2020;15(6):997-1003. doi:10.1007/s11739-019-02264-4
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Febriyani, Andi Makbul Aman, Harun Iskandar

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The full license is at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.










