Discordance between Fasting Plasma Glucose (FPG) and HbA1c in Diagnosing Diabetes and Pre-diabetes in The Malaysian Cohort
DOI:
https://doi.org/10.15605/jafes.036.02.02Keywords:
type 2 diabetes mellitus, fasting plasma glucose, HbA1c, The Malaysian Cohort, diagnosis, population differencesAbstract
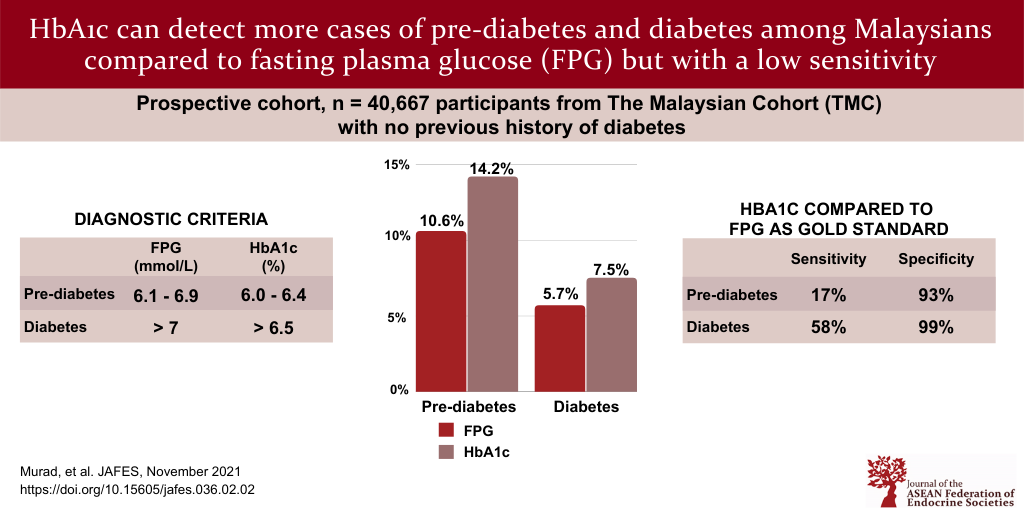
Objective. In this present study, we aim to evaluate the accuracy of the HbA1c relative to fasting plasma glucose (FPG) in the diagnosis of diabetes and pre-diabetes among The Malaysian Cohort (TMC) participants.
Methodology. FPG and HbA1c were taken from 40,667 eligible TMC participants that have no previous history of diabetes, aged between 35-70 years and were recruited from 2006 – 2012. Participants were classified as normal, diabetes and pre-diabetes based on the 2006 World Health Organization (WHO) criteria. Statistical analyses were performed using ANOVA and Chi-square test, while Pearson correlation and Cohen’s kappa were used to examine the concordance rate between FPG and HbA1c.
Results. The study samples consisted of 16,224 men and 24,443 women. The prevalence of diabetes among the
participants was 5.7% and 7.5% according to the FPG and HbA1c level, respectively. Based on FPG, 10.6% of the
participants had pre-diabetes but this increased to 14.2% based on HbA1c (r=0.86; P<0.001). HbA1c had a sensitivity of 58.20 (95% CI: 56.43, 59.96) and a specificity of 98.59 (95% CI: 98.46, 98.70).
Conclusion. A higher prevalence of pre-diabetes and diabetes was observed when using HbA1c as a diagnosis tool, suggesting that it could possibly be more useful for early detection. However, given that HbA1c may also have lower sensitivity and higher false positive rate, several diagnostic criteria should be used to diagnose diabetes accurately.
Downloads
References
Adeghate E, Schattner P, Dunn E. An update on the etiology and epidemiology of diabetes mellitus. Ann N Y Acad Science. 2006;1084:1-29. https://pubmed.ncbi.nlm.nih.gov/17151290. https://doi.org/10.1196/annals.1372.029.
Institute for Public Health (IPH) 2015. National Health and Morbidity Survey 2015 (NHMS 2015). Non-communicable diseases, risk factors and other health problems. Vol. 2. Kuala Lumpur, Malaysia. 2015;1-315. Available from: https://www.moh.gov.my/moh/resources/nhmsreport2015vol2.pdf.
Jamal R, Syed Zakaria SZ, Kamaruddin MA, et al. The Malaysian Cohort (TMC) project: A prospective study of non-communicable diseases in a multiethnic population. Int J Epidemiology. 2015;44(22):423-31. https://pubmed.ncbi.nlm.nih.gov/24729425. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4469794. https://doi.org/10.1093/ije/dyu089.
Institute for Public Health (IPH) 2019. National Health and Morbidity Survey 2019 (NHMS 2019). National Health and Morbidity Survey 2019. Non-communicable diseases, healthcare demand, and health literacy. Key findings. Available at http://www.iku.gov.my/nhms.
Ashraf S. Diagnosis of type 2 diabetes using serial fasting plasma glucose versus HbA1c in the primary care setting. Aust J Gen Pract. 2019;48(5):269-71. https://pubmed.ncbi.nlm.nih.gov/31129936. https://doi.org/10.31128/AJGP-07-18-4652.
Modhumi Khan RM, Yu Chua ZJ, Tan JC, Yang Y, Liao Z, Zhao Y. From pre-diabetes to diabetes: Diagnosis, treatments and translational research. Medicina (Kaunas). 2019;55(9):546. https://pubmed.ncbi.nlm.nih.gov/31470636. https://pubmed.ncbi.nlm.nih.gov/PMC6780236. https://doi.org/10.3390/medicina55090546.
Ye Y, Xie H, Zhao X, Zhang S. The oral glucose tolerance test for the diagnosis of diabetes mellitus in patients during acute coronary syndrome hospitalization: A meta-analysis of diagnostic test accuracy. Cardiovasc Diabetol. 2012; 11:155. https://pubmed.ncbi.nlm.nih.gov/23270530. https://pubmed.ncbi.nlm.nih.gov/PMC3534587. https://doi.org/10.1186/1475-2840-11-155.
Use of glycated haemoglobin (HbA1c) in the diagnosis of diabetes mellitus: Abbreviated report of a WHO Consultation. Geneva: World Health Organization. 2011. https://pubmed.ncbi.nlm.nih.gov/26158184. Bookshelf ID:NBK304267.
KP Peterson, JG Pavlovich, D Goldstein. et al. What is hemoglobin A1c? An analysis of glycated hemoglobins by electrospray ionization mass spectrometry. Clin Chem. 1998;44(9):1951–8. https://pubmed.ncbi.nlm.nih.gov/9732983.
Koenig RJ, Peterson CM, Jones RL et al. Correlation of glucose regulation and hemoglobin A1c in diabetes mellitus. N Engl J Med. 1976;295(8):417–20. https://pubmed.ncbi.nlm.nih.gov/934240. https://doi.org/10.1056/NEJM197608192950804.
Treviño G. Consensus statement on the worldwide standardization of the haemoglobin A1c measurement: The American Diabetes Association, European Association for the Study of Diabetes, International Federation of Clinical Chemistry and Laboratory Medicine, and the International Diabetes Federation: Response to the Consensus Committee. Diabetes Care. 2007;30(12):e141. https://pubmed.ncbi.nlm.nih.gov/18042750. https://doi.org/10.2337/dc07-1752.
International Expert Committee. International Expert Committee report on the role of the A1c assay in the diagnosis of diabetes. Diabetes Care. 2009;32(7):1327-34. https://pubmed.ncbi.nlm.nih.gov/19502545. https://pubmed.ncbi.nlm.nih.gov/PMC2699715. https://doi.org/10.2337/dc09-9033.
Use of glycated haemoglobin (HbA1c) in the diagnosis of diabetes mellitus: Abbreviated report of a WHO consultation. Geneva: World Health Organization; 2011. Bookshelf ID:NBK304267/.
Wang B, Liu MC, Li XY, et al. Cutoff point of HbA1c for diagnosis of diabetes mellitus in Chinese individuals. PLoS One. 2016;18:11(11):e0166597. https://pubmed.ncbi.nlm.nih.gov/27861599. https://pubmed.ncbi.nlm.nih.gov/PMC5115764. https://doi.org/10.1371/journal.pone.0166597.
Nam HK, Cho WK, Kim JH, et al. HbA1c cutoff for prediabetes and diabetes based on oral glucose tolerance test in obese children and adolescents. J Korean Med Sci. 2018;19;33(12):e93. https://pubmed.ncbi.nlm.nih.gov/29542302. https://pubmed.ncbi.nlm.nih.gov/PMC5852422. https://doi.org/10.3346/jkms.2018.33.e93.
Wan Nazaimoon WM, Md Isa SH, Wan Mohamad WB, et al. Prevalence of diabetes in Malaysia and usefulness of HbA1c as a diagnostic criterion. Diabet Med. 2013; 30(7):825-8. https://pubmed.ncbi.nlm.nih.gov/23413941. https://doi.org/doi: 10.1111/dme.12161.
Lim WY, Ma S, Heng D, Tai ES, Khoo CM, Loh TP. Screening for diabetes with HbA1c: Test performance of HbA1c compared to fasting plasma glucose among Chinese, Malay and Indian community residents in Singapore. Sci Rep. 2018; 20;8(1):12419. https://pubmed.ncbi.nlm.nih.gov/30127499. https://pubmed.ncbi.nlm.nih.gov/PMC6102285. https://doi.org/10.1038/s41598-018-29998-z.
Herman WH, Dungan KM, Wolffenbuttel BHR, et al. Racial and ethnic differences in mean plasma glucose, hemoglobin A1c, and 1,5-anhydroglucitol in over 2000 patients with type 2 diabetes. J Clin Endocrinol Metab. 2009; 94(5):1689-94. https://pubmed.ncbi.nlm.nih.gov/19276235. https://doi.org/10.1210/jc.2008-1940.
Ho-Pham LT, Nguyen UDT, Tran TX, Tran TX, Nguyen TV. Discordance in the diagnosis of diabetes: Comparison between HbA1c and fasting plasma glucose. PLoS ONE. 2017; 12(8): e0182192. https://pubmed.ncbi.nlm.nih.gov/28817663. https://pubmed.ncbi.nlm.nih.gov/PMC5560685. https://doi.org/10.1371/journal.pone.0182192.
Kim HK, Kim CH, Kim EU, Bae SJ, Park JY. Usefulness of hemoglobin A1c as a criterion of dysglycemia in the definition of metabolic syndrome in Koreans. Diabetes Res Clin Pract. 2012; 95(3):333-9. https://pubmed.ncbi.nlm.nih.gov/22071434. https://doi.org/10.1016/j.diabres.2011.10.012.
Unwin N, Howitt C, Mc Rose A, Samuels TA, Hennis AJ, Hambleton IR. Prevalence and phenotype of diabetes and prediabetes using fasting glucose vs H bA1c in a Caribbean population. J Glob Health. 2017;7(2):020407. https://pubmed.ncbi.nlm.nih.gov/28959440. https://pubmed.ncbi.nlm.nih.gov/PMC5604098. https://doi.org/10.7189/jogh.07.020407.
Hudson PR, Child DF, Jones H, Williams CP. Differences in rates of glycation (glycation index) may significantly affect individual HbA1c results in type 1 diabetes. Ann Clin Biochem. 1999; 36(Pt 4):451-9. https://pubmed.ncbi.nlm.nih.gov/10456207. https://doi.org/10.1177/000456329903600408.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care.2010; 33 (Suppl 1):S26-9. https://pubmed.ncbi.nlm.nih.gov/24357215. https://doi.org/10.2337/dc14-S081.
Gallagher EJ, Le Roith D, Bloomgarden Z. Review of hemoglobin A(1c) in the management of diabetes. J Diabetes. 2009;1(1):9-17. https://pubmed.ncbi.nlm.nih.gov/20923515. https://doi.org/10.1111/j.1753-0407.2009.00009.x
American Association of Clinical Endocrinologists/American College of Endocrinology Statement on the use of hemoglobin A1C for the diagnosis of diabetes. AACE/ACE Position Statement. 2010;16(2):155-6. https://doi.org/10.4158/EP.16.2.155.
Published
How to Cite
Issue
Section
License
Copyright (c) 2021 Nor Azian Abdul Murad, Noraidatulakma Abdullah, Mohd Arman Kamaruddin, Nazihah Abd Jalal, Norliza Ismail, Nurul Ain Mhd Yusof, Norlaila Mustafa, Rahman Jamal

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The full license is at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.










