Accuracy of Waist Circumference Measurement Using the WHO versus NIH Protocol in Predicting Visceral Adiposity Using Bioelectrical Impedance Analysis among Overweight and Obese Adult Filipinos in a Tertiary Hospital
DOI:
https://doi.org/10.15605/jafes.036.02.13Keywords:
waist circumference, central obesity, visceral adiposityAbstract
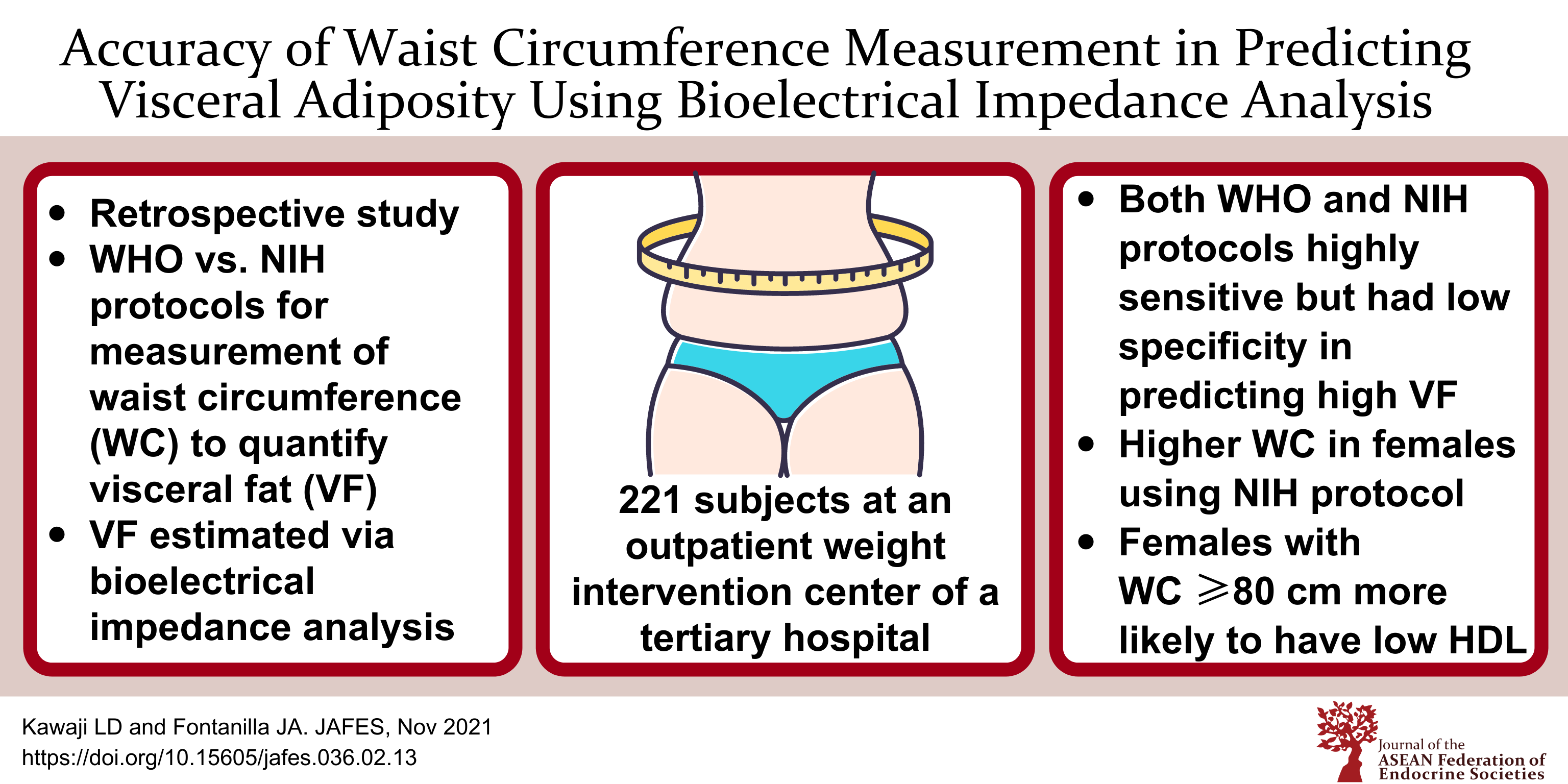
OBJECTIVES. The study aimed to compare the performance of weight circumference (WC) measurement using the (World Health Organization) WHO versus National Institutes of Health (NIH) protocol in identifying visceral adiposity, and to determine the association of WC with cardiometabolic risk factors among overweight and obese adult Filipinos.
METHODOLOGY. A retrospective study involving 221 subjects (99 males, 122 females) evaluated at an outpatient weight intervention center of a tertiary hospital. The WC was measured at the superior border of the iliac crest (WC-NIH) and midway between the lowest rib and the iliac crest (WC-WHO) for each patient. Using visceral fat rating (VF) derived via bioelectrical impedance analysis (BIA) as reference standard, diagnostic accuracy tests for both protocols (using cut-offs of ≥90 cm in males and ≥80 cm in females) were done. Cardiometabolic parameters were also obtained, and binary logistic regression was performed to determine associations with WC.
RESULTS. Among males, WC-WHO had 96% sensitivity (95% CI 88.8%-99.2%) and 25% specificity (95% CI 9.77%-46.7%) while WC-NIH had 94.7% sensitivity (95% CI 86.9%-98.5%) and 29.2% specificity (95% CI 12.6%-51.1%) to predict high VF >12. Among females, WC-WHO had 100% sensitivity (95% CI 90%-100%) and 24.1% specificity (95% CI 15.6%-34.5%) while WC-NIH had 100% sensitivity (95% CI 90%-100%) and 4.6% specificity (95% CI 1.3%-11.4%). Prevalence of high VF was significantly greater among males – 75.8% (95% CI 66.1%-83.8%) vs. 28.7% (95% CI 20.9%-37.6%) in females (p<0.001). Among females, WC-NIH tended to have higher measurements than WC-WHO by an average of 4.67 cm. Females with WC-WHO measurements of at least 80 cm were approximately four times more likely to have low (<50 mg/dL) HDL levels (cOR 3.82, p=<0.05), even after adjusting for age (aOR 3.83, p<0.05).
CONCLUSION. WC measurement using the WHO and NIH protocols were both highly sensitive but had low specificity in predicting high VF estimated via BIA among overweight and obese adult Filipinos in this study. WC-NIH measurements tended to be higher among the females, which may affect the classification of central obesity when using this protocol. WC ≥80 cm measured using the WHO protocol was associated with low HDL levels among female subjects. Prospective studies conducted among the general Filipino population are recommended to verify these findings.
Downloads
References
Food and Nutrition Research Institute – Expanded National Nutritional Survey 2018. https://www.fnri.dost.gov.ph/images/sources/eNNS2018/AdultsandElderly.pdf.
Klein S, Allison DB, Heymsfield SB, et al. Waist circumference and cardiometabolic risk: A consensus statement from Shaping America's Health: Association for Weight Management and Obesity Prevention; NAASO, The Obesity Society; the American Society for Nutrition; and the American Diabetes Association. Am J Clinical Nutr. 2007;85(5):1197-1202. https://pubmed.ncbi.nlm.nih.gov/17490953. https://doi.org/10.1093/ajcn/85.5.1197.
Sinha R, Dufour S, Petersen KF, et al. Assessment of skeletal muscle triglyceride content by (1)H nuclear magnetic resonance spectroscopy in lean and obese adolescents: relationships to insulin sensitivity, total body fat, and central adiposity. Diabetes. 2002;51(4):1022–7. https://pubmed.ncbi.nlm.nih.gov/11916921. https://doi.org/10.2337/diabetes.51.4.1022.
Seppälä-Lindroos A, Vehkavaara S, Häkkinen AM, et al. Fat accumulation in the liver is associated with defects in insulin suppression of glucose production and serum free fatty acids independent of obesity in normal men. J Clin Endocrinol Metab. 2002;87(7):3023–28. https://pubmed.ncbi.nlm.nih.gov/12107194. https://doi.org/10.1210/jcem.87.7.8638.
Björntorp P. Body fat distribution, insulin resistance, and metabolic diseases. Nutrition. 1997;13(9):795–803. https://pubmed.ncbi.nlm.nih.gov/9290093. https://doi.org/10.1016/s0899-9007(97)00191-3.
Pagsisihan D, Sandoval MA, Paz-Pacheco E, Jimeno C. Low indices of overweight and obesity are associated with cardiometabolic diseases among adult Filipinos in a rural community. J ASEAN Fed Endocr Soc. 2016;31(2): 97-105. https://doi.org/10.15605/jafes.031.02.04
Shuster A, Patlas M, Pinthus JH, Mourtzakis M. The clinical importance of visceral adiposity: A critical review of methods for visceral adipose tissue analysis. Br J Radiol. 2012;85(1009):1-10. https://pubmed.ncbi.nlm.nih.gov/21937614. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3473928. https://doi.org/10.1259/bjr/38447238.
Yusuf S, Hawken S, Ounpuu S, et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: A case-control study. Lancet. 2005;366(9497):1640–49. https://pubmed.ncbi.nlm.nih.gov/16271645. https://doi.org/10.1016/S0140-6736(05)67663-5.
Suk SH, Sacco RL, Boden-Albala B, et al. Abdominal obesity and risk of ischemic stroke: The Northern Manhattan Stroke Study. Stroke. 2003;34(7):1586–92. https://pubmed.ncbi.nlm.nih.gov/12775882. https://doi.org/10.1161/01.STR.0000075294.98582.2F.
Visscher TL, Seidell JC, Molarius A, van der Kuip D, Hofman A, Witteman JC. A comparison of body mass index, waist-hip ratio and waist circumference as predictors of all-cause mortality among the elderly: The Rotterdam study. Int J Obes Relat Metab Disord. 2001;25(11):1730–5. https://pubmed.ncbi.nlm.nih.gov/11753597. https://doi.org/10.1038/sj.ijo.0801787.
Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112(17):2735–52. https://pubmed.ncbi.nlm.nih.gov/16157765. https://doi.org/10.1161/CIRCULATIONAHA.105.169404.
World Health Organization. Regional Office for the Western Pacific. The Asia-Pacific perspective: Redefining obesity and its treatment. Sydney: Health Communications Australia; 2000. https://apps.who.int/iris/bitstream/handle/10665/206936/0957708211_eng.pdf?sequence=1&isAllowed=y.
Bosy-Westphal A, Booke C-A, Blocker T, et al. Measurement site for waist circumference affects its accuracy as an index of visceral and abdominal subcutaneous fat in a Caucasian population. J Nutr. 2010;140(5):956–61. https://pubmed.ncbi.nlm.nih.gov/20335625. https://doi.org/10.3945/jn.109.118737.
Millar SR, Perry IJ, Van den Broeck J, Phillips CM. Optimal central obesity measurement site for assessing cardiometabolic and type 2 diabetes risk in middle-aged adults. PLoS One. 2015;10(6):e0129088. https://pubmed.ncbi.nlm.nih.gov/26042771. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4456242. https://doi.org/10.1371/journal.pone.0129088.
Ma WY, Yang CY, Shih SR, et al. Measurement of waist circumference: Midabdominal or iliac crest? Diabetes Care. 2013;36(6):1660-6. https://pubmed.ncbi.nlm.nih.gov/23275359. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3661855. https://doi.org/10.2337/dc12-1452.
Ross R, Berentzen T, Bradshaw AJ, et al. Does the relationship between waist circumference, morbidity and mortality depend on measurement protocol for waist circumference? Obesity Rev. 2008;9(4):312–25. https://pubmed.ncbi.nlm.nih.gov/17956544. https://doi.org/10.1111/j.1467-789X.2007.00411.x.
Nagai M, Komiya H, Mori Y, Ohta T, Kasahara Y, Ikeda Y. Estimating visceral fat area by multifrequency bioelectrical impedance. Diabetes Care. 2010;33(5):1077-9. https://pubmed.ncbi.nlm.nih.gov/20150289. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2858179. https://doi.org/10.2337/dc09-1099.
Wang JG, Zhang Y, Chen HE, et al. Comparison of two bioelectrical impedance analysis devices with dual energy x-ray absorptiometry and magnetic resonance imaging in the estimation of body composition. J Strength Cond Res. 2013;27(1):236-43. https://pubmed.ncbi.nlm.nih.gov/22344056. https://doi.org/10.1519/JSC.0b013e31824f2040.
Lee DH, Park KS, Ahn S, et al. Comparison of abdominal visceral adipose tissue area measured by computed tomography with that estimated by bioelectrical impedance analysis method in Korean subjects. Nutrients. 2015;7(12):10513–24. https://pubmed.ncbi.nlm.nih.gov/26694460. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4690100. https://doi.org/10.3390/nu7125548.
Shoji K, Maeda K, Nakamura T, Funahashi T, Matsuzawa Y, Shimomura I. Measurement of visceral fat by abdominal bioelectrical impedance analysis is beneficial in medical checkup. Obes Res Clin Pract. 2008;2(4):I-II. https://pubmed.ncbi.nlm.nih.gov/24351854. https://doi.org/10.1016/j.orcp.2008.09.001.
Ryo M, Maeda K, Onda T, et al. A new simple method for the measurement of visceral fat accumulation by bioelectrical impedance. Diabetes Care. 2005;28(2):451-3. https://pubmed.ncbi.nlm.nih.gov/15677816. https://doi.org/10.2337/diacare.28.2.451.
Bosy-Westphal A, Later W, Hitze B, et al. Accuracy of bioelectrical impedance consumer devices for measurement of body composition in comparison to whole body magnetic resonance imaging and dual X-ray absorptiometry. Obes Facts. 2008;1(6):319-24. https://pubmed.ncbi.nlm.nih.gov/20054195. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6452160. https://doi.org/10.1159/000176061.
Park KS, Lee DH, Lee JE, et al. Comparison between two methods of bioelectrical impedance analyses for accuracy in measuring abdominal visceral fat area. J Diabetes Complications. 2016;30(2):343-9. https://pubmed.ncbi.nlm.nih.gov/26620129. https://doi.org/10.1016/j.jdiacomp.2015.10.014.
Lu HK, Chen YY, Yeh C, et al. Discrepancies between leg-to-leg bioelectrical impedance analysis and computerized tomography in abdominal visceral fat measurement. Sci Rep. 2017;7(1):9102. https://pubmed.ncbi.nlm.nih.gov/28831095. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5567333. htts://doi.org/10.1038/s41598-017-08991-y.
Tanita Institute Contract Study. Algorithm development for estimating visceral fat rating. SB Heymsfield MD. Columbia University College of Physicians and Surgeons; 2004.
Wang Z. Japanese-American differences in visceral adiposity and a simplified estimation method for visceral adipose tissue. North American Association for the Study of Obesity Annual Meeting. Abstract 518-P; 2004.
Tanita Corporation. Tanita Technical Bulletin: Visceral fat measurement. https://www.tanita.com/data/File/AdditionalResearch/VisceralFatMeasurmentp1.pdf?rev=72DE.
Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension. 2020;75(6):1334-57. https://pubmed.ncbi.nlm.nih.gov/32370572. https://doi.org/10.1161/HYPERTENSIONAHA.120.15026.
American Diabetes Association. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2021. Diabetes Care. 2021;44 (Suppl 1):S15-33. https://pubmed.ncbi.nlm.nih.gov/33298413. https://doi.org/10.2337/dc21-S002.
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–421. https://pubmed.ncbi.nlm.nih.gov/12485966.
Hu L, Huang X, You C, et al. Prevalence of overweight, obesity, abdominal obesity and obesity-related risk factors in southern China. PLoS One. 2017;12(9):e0183934. https://pubmed.ncbi.nlm.nih.gov/28910301. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5598943. https://doi.org/10.1371/journal.pone.0183934.
Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–5. https://pubmed.ncbi.nlm.nih.gov/19805654. https://doi.org/10.1161/CIRCULATIONAHA.109.192644.
Ross R, Neeland IJ, Yamashita S, et al. Waist circumference as a vital sign in clinical practice: A consensus statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol. 2020;16(3):177-89. https://pubmed.ncbi.nlm.nih.gov/32020062. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7027970. https://doi.org/10.1038/s41574-019-0310-7.
Published
How to Cite
Issue
Section
License
Copyright (c) 2021 Leslie Daphne Kawaji, Joy Arabelle Fontanilla

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The full license is at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.










