Weekly Versus Daily Levothyroxine Tablet Replacement in Adults with Hypothyroidism
A Meta-Analysis
DOI:
https://doi.org/10.15605/jafes.036.02.07Keywords:
hypothyroidism, levothyroxine, thyroid hormone, adherence, weekly replacementAbstract
Objectives. Daily levothyroxine is the treatment of choice and standard of care in hypothyroidism, sufficient to restore thyroid stimulating hormone (TSH) to normal range. For many patients, daily lifelong therapy is required, making adherence a major issue. In such cases, weekly replacement may be a suitable alternative to improve adherence. In this study, we aimed to determine the efficacy and safety of weekly levothyroxine replacement among adults with hypothyroidism.
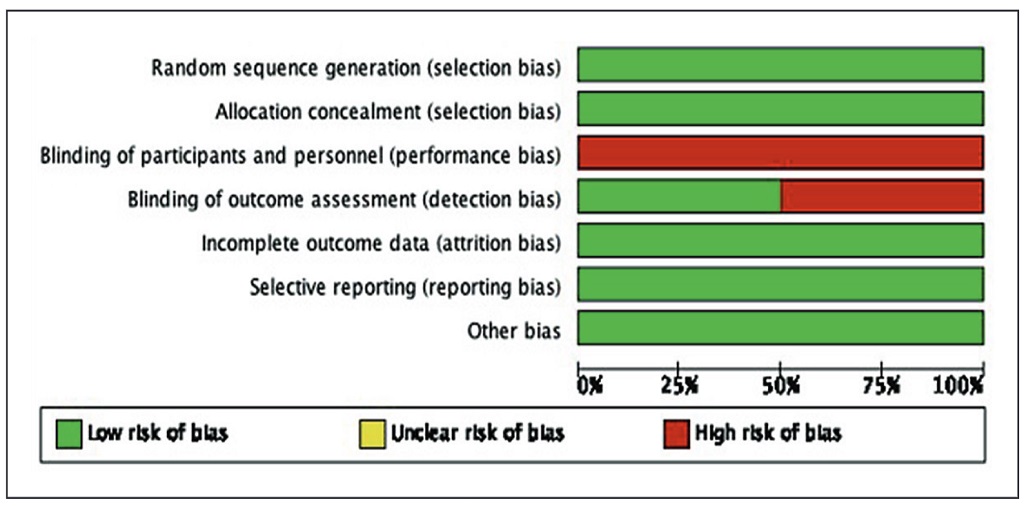
Methodology. Electronic databases were searched. Two reviewers (HCC and RBL) independently screened the abstracts, reviewed full-text papers, critically appraised the quality of included studies using PRISMA guidelines. Meta-analysis was performed using the random-effects model. The primary outcome is the difference in serum TSH levels between weekly and daily administration, while secondary outcomes included adverse events and symptoms of hypothyroidism.
Results. The primary outcome is the difference in serum TSH levels between weekly and daily administration. Secondary outcomes included adverse events and clinical symptoms. The study included two randomized trials (n=109) in the primary analysis. The difference in TSH levels was 1.78 mIU/mL higher [(95% confidence interval (CI): 1.28 to 2.28, p<0.00001] at 6 weeks and 1.22 mIU/mL higher (95% CI: 0.76 to 1.67, p<0.00001) at 12 weeks for the weekly regimen. There was no significant heterogeneity between the two groups. There was no significant difference in hypothyroid symptoms and adverse events before and after levothyroxine treatment within each group.
Conclusions. Weekly levothyroxine resulted in less suppression and higher mean serum TSH levels, while still remaining within the normal reference range. It may be a suitable alternative for non-adherent patients. However, larger randomized trials with longer duration of follow-up are needed to firmly establish its role.
Downloads
References
Jonklaas J, Bianco AC, Bauer AJ, et al. Guidelines for the treatment of hypothyroidism: prepared by the American Thyroid Association Task Force on thyroid hormone replacement. Thyroid. 2014;24(12):1670-751. https://pubmed.ncbi.nlm.nih.gov/25266247. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4267409. https://doi.org/10.1089/thy.2014.0028.
Rajput R, Pathak V. The effect of daily versus weekly levothyroxine replacement on thyroid function test in hypothyroid patients at a tertiary care center in Haryana. Eur Thyroid J. 2017;6(5):250-4. https://pubmed.ncbi.nlm.nih.gov/29071237. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5649268. https://doi.org/10.1159/000477348.
Bornschein A, Paz-Filho G, Graf H, de Carvalho GA. Treating primary hypothyroidism with weekly doses of levothyroxine: A randomized, single-blind, crossover study. Arq Bras Endocrinol Metabol. 2012;56(4):250-8. https://pubmed.ncbi.nlm.nih.gov/22790470. https://doi.org/10.1590/s0004-27302012000400006.
Grebe SK, Cooke RR, Ford HC, et al. Treatment of hypothyroidism with once weekly thyroxine. J Clin Endocrinol Metab. 1997;82(3):870-5. https://pubmed.ncbi.nlm.nih.gov/9062499. https://doi.org/10.1210/jcem.82.3.3830.
John-Kalarickal J, Pearlman G, Carlson HE. New medications which decrease levothyroxine absorption. Thyroid. 2007;17(8):763-5. https://pubmed.ncbi.nlm.nih.gov/17725434. https://doi.org/10.1089/thy.2007.0060.
Wiersinga WM. Thyroid hormone replacement therapy. Horm Res. 2001;56(Suppl 1):74-81. https://pubmed.ncbi.nlm.nih.gov/11786691. https://doi.org/10.1159/000048140.
Bernstein RS, Robbins J. Intermittent therapy with L-thyroxine. N Engl J Med. 1969; 281(26):1444-8. https://pubmed.ncbi.nlm.nih.gov/4187605. https://doi.org/10.1056/NEJM196912252812603.
Sekadde CB, Slaunwhite WR Jr, Aceto T Jr, Murray K. Administration of thyroxin once a week. J Clin Endocrinol Metab. 1974;39(4):759-64. https://pubmed.ncbi.nlm.nih.gov/4411877. https://doi.org/10.1210/jcem-39-4-759.
Rangan S, Tahrani AA, Macleod AF, Moulik PK. Once weekly thyroxine treatment as a strategy to treat non-compliance. Postgrad Med J. 2007; 83(984):e3. https://pubmed.ncbi.nlm.nih.gov/17916865. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2600132. https://doi.org/10.1136/pgmj.2007.060244.
Oliver C, Grino M, Moatti-Vacher Coponat P, Morange I, Retornaz F. Prise hebdomadaire de L-thyroxine dans un cas de non-observance du traitement substitutif [Once weekly L-thyroxine treatment in non-compliance: A case report]. La Revue de Médecine Internet. 2017; 38(11):766-8. https://doi.org/10.1016/j.revmed.2017.06.005.
Walker JN, Shillo P, Ibbotson V, et al. A thyroxine absorption test followed by weekly thyroxine administration: A method to assess non-adherence to treatment. Eur J Endocrinol. 2013;168(6):913-7. https://pubmed.ncbi.nlm.nih.gov/23554450. https://doi.org/10.1530/EJE-12-1035.
Taylor J, Williams BO, Frater J, Stott DJ, Connell J. Twice-weekly dosing for thyroxine replacement in elderly patients with primary hypothyroidism. J Int Med Res. 1994;22(5):273-7. https://pubmed.ncbi.nlm.nih.gov/7867872. https://doi.org/10.1177/030006059402200504.
Altuntaş F, Uysal AR, Çorapçıoğlu D, Erol Ç. Twice weekly L-T4 for the treatment of primary hypothyroidism. Turk J Endocrinol Metab. 2004;1:25-34. http://www.turkjem.org/uploads/pdf/8-1-0_25-34.pdf.
Dayal D, Saini L, Attri SV, Singh B, Bhalla AK. Daily versus alternate day thyroxine therapy to maintain euthyroidism in children with congenital hypothyroidism. Int J Endocrinol Metab. 2013;11(4):e9499. https://pubmed.ncbi.nlm.nih.gov/24719634. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3968978. https://doi.org/10.5812/ijem.9499.
Negro R, Valcavi R, Agrimi D, Toulis KA. Levothyroxine liquid solution versus tablet for replacement treatment in hypothyroid patients. Endocr Pract. 2014; 20(9):901-6. https://pubmed.ncbi.nlm.nih.gov/24793916. https://doi.org/10.4158/EP13378.OR.
Crilly M, Esmail A. Randomised controlled trial of a hypothyroid educational booklet to improve thyroxine adherence. Br J Gen Pract. 2005;55(514):362-8. https://pubmed.ncbi.nlm.nih.gov/15904555. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1463159.
Laycock K, Beale C, Peters C, Anderson J. Intramuscular levothyroxine: A solution to a mental health related thyroid crisis. BMJ Case Rep. 2019;12(8):e228147. https://pubmed.ncbi.nlm.nih.gov/31434663. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6706664. https://doi.org/10.1136/bcr-2018-228147.
Hays MT. Parenteral thyroxine administration. Thyroid. 2007;17(12):127-9. https://pubmed.ncbi.nlm.nih.gov/17316114. https://doi.org/10.1089/thy.2006.0283.
Jayakumari C, Nair A, Khadar JP, et al. Efficacy and safety of once-weekly thyroxine for thyroxine-resistant hypothyroidism. J Endocr Soc. 2019;3(12):2184-93. https://pubmed.ncbi.nlm.nih.gov/31723717. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6834071. https://doi.org/10.1210/js.2019-00212.
Centanni M, Benvenga S, Sachmechi I. Diagnosis and management of treatment-refractory hypothyroidism: an expert consensus report. J Endocrinol Invest. 2017; 40(12):1289-301. https://pubmed.ncbi.nlm.nih.gov/28695483. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5680379. https://doi.org/10.1007/s40618-017-0706-y.
Shilo L, Kovatz S, Hadari R, Weiss E, Nabriski D, Shenkman L. Massive thyroid hormone overdose: Kinetics, clinical manifestations and management. Isr Med Assoc J. 2002;4(4):298-9. https://pubmed.ncbi.nlm.nih.gov/12001709.
Savran Y, Mengi T, Keskinkilic M. A severe case of levothyroxine intoxication successfully treated in intensive care unit. J Acute Dis. 2018;7(4):175-7. https://doi.org/10.4103/2221-6189.241029.
Published
How to Cite
Issue
Section
License
Copyright (c) 2021 Harold Henrison Chiu, Ramon Larrazabal, Angelique Bea Uy, Cecilia Jimeno

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The full license is at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.










