Metabolic Profile of People Living with HIV in a Treatment Hub in Manila, Philippines
A Pre- and Post-Antiretroviral Analysis
DOI:
https://doi.org/10.15605/jafes.037.01.17Keywords:
HIV, AIDS, dyslipidemia, hyperglycemia, antiretroviral therapyAbstract
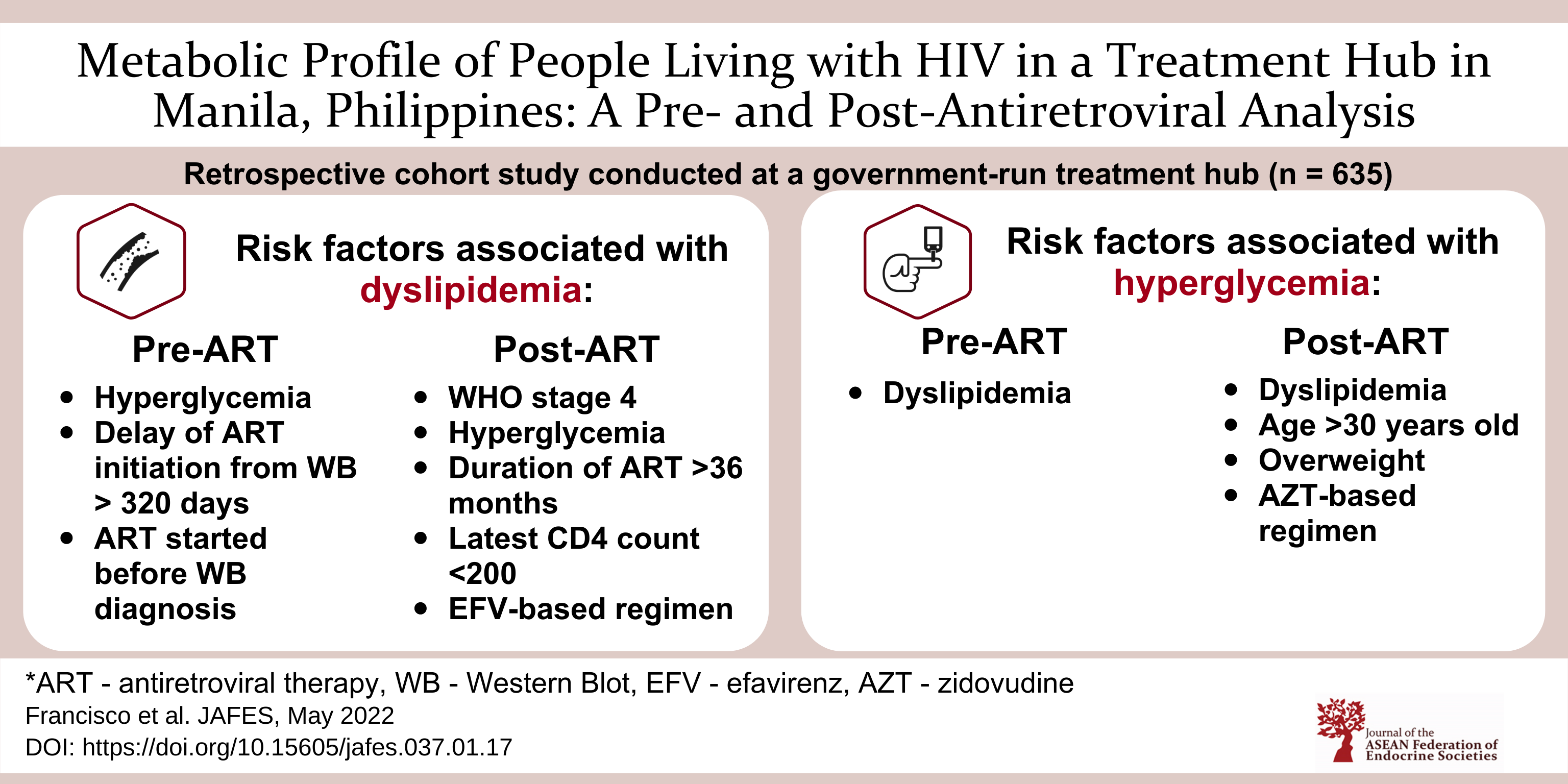
Objectives. People living with HIV (PLHIV) are susceptible to develop dyslipidemia and hyperglycemia. This study aims to determine the prevalence of these metabolic derangements among Filipino PLHIV.
Methodology. We reviewed 635 medical records in a treatment hub in Manila, Philippines from January 2004 to July 2016. Logistic regression analysis was done to determine factors associated with dyslipidemia and hyperglycemia pre- and post-ART.
Results. Among 635 PLHIV, 97.3% were males with mean age of 30 years and median CD4 count of 207 cells/mm3. Pre-ART, prevalence of dyslipidemia was 65.4% and hyperglycemia was 10.4%. Risk factors for dyslipidemia include hyperglycemia (AOR 3.8, p 0.001) and >320 days delay in ART initiation from HIV confirmation (AOR 1.5, p 0.032), while dyslipidemia was associated with hyperglycemia (AOR 3.1, p 0.001). Post-ART, prevalence of dyslipidemia was 48.6% and hyperglycemia was 15.6%. Risk factors for post-ART dyslipidemia include being WHO stage 4 (AOR 2.1, p 0.021), hyperglycemia (AOR 16.1, p<0.001), >36 months ART duration (AOR 8.7, p<0.001) and efavirenz-based ART (AOR 2.8, p<0.001). Low CD4 count post-ART had a negative correlation with dyslipidemia (AOR 0.5, p 0.005). Post-ART hyperglycemia was associated with age >30 years (AOR 2.1, p 0.004), being overweight (AOR 1.8, p 0.023), dyslipidemia (AOR 17.8, p<0.001) and zidovudine-based ART (AOR 1.4, p 0.051).
Conclusion. Dyslipidemia and hyperglycemia prevalence was high in Filipino PLHIV. Traditional, HIV and treatment related factors contributed to its development. Intensive monitoring and initiation of appropriate treatment is recommended.
Downloads
References
Gutierrez AD, Balasubramanyam A. Dysregulation of glucose metabolism in HIV patients: Epidemiology, mechanisms and management. Endocrine. 2012;41(1):1–10. https://pubmed.ncbi.nlm.nih.gov/22134974. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3417129. https://doi.org/10.1007/s12020-011-9565-z
Zhou DT, Kodogo V, Chokuona KFV, Gomo E, Oektedalen O, Stray-Pedersen B. Dyslipidemia and cardiovascular disease risk profiles of patients attending an HIV treatment clinic in Harare, Zimbabwe. HIV/AIDS (Auckl). 2015;7:145–55. https://pubmed.ncbi.nlm.nih.gov/25999764. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4435239. https://doi.org/10.2147/HIV.S78523.
Da Cunha J, Maselli LMF, Stem ACB, Spada C, Bydlowski SP. Impact of antiretroviral therapy on lipid metabolism of human immunodeficiency virus-infected patients: Old and new drugs. World J Virol. 2015;4(2):56-77. https://pubmed.ncbi.nlm.nih.gov/25964872. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4419122. https://doi.org/10.5501/wjv.v4.i2.56.
Omech B, Sempa J, Castelnuovo B, et. al. Prevalence of HIV-associated metabolic abnormalities among patients taking first-line antiretroviral therapy in Uganda. ISRN AIDS. 2012;2012:960178:1-6. https://pubmed.ncbi.nlm.nih.gov/24052885. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3767451. https://doi.org/10.5402/2012/960178.
Husain NEO, Ahmed MH. Managing dyslipidemia in HIV/AIDS patients: Challenges and solutions. HIV/AIDS (Auckl). 2015;7:1–10. https://pubmed.ncbi.nlm.nih.gov/25565897. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4274137. https://doi.org/10.2147/HIV.S46028.
Guillen MA, Mejia FA, Villena J, Turin CG, Carcamo CP, Ticse R. Insulin resistance by homeostasis model assessment in HIV-infected patients on highly active antiretroviral therapy: Cross-sectional study. Diabetol Metab Syndr. 2015;7:49. https://pubmed.ncbi.nlm.nih.gov/26034512. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4450995. https://doi.org/10.1186/s13098-015-0046-z.
Anuurad E, Bremer A, Berglund L. HIV protease inhibitors and obesity. Curr Opin Endocrinol Diabetes Obes. 2010;17(5):478–85. https://pubmed.ncbi.nlm.nih.gov/20717021. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3076638. https://doi.org/10.1097/MED.0b013e32833dde87.
Misra R, Chandra P, Riechman SE, et al. Relationship of ethnicity and CD4 count with glucose metabolism among HIV patients on Highly-Active Antiretroviral Therapy (HAART). BMC Endocr Disord. 2013;13:13. https://pubmed.ncbi.nlm.nih.gov/23607267. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3751670. https://doi.org/10.1186/1472-6823-13-13.
Hejazi N, Rajikan R, Kwok Choong CL, Sahar S. Metabolic abnormalities in adult HIV infected population on anti-retroviral medication in Malaysia: A cross-sectional survey. BMC Public Health. 2013;13:758. https://pubmed.ncbi.nlm.nih.gov/23947428. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3844340. https://doi.org/10.1186/1471-2458-13-758.
World Health Organization. Updated recommendations on first-line and second-line antiretroviral regimens and post-exposure prophylaxis and recommendations on early infant diagnosis of HIV. https://www.who.int/publications/i/item/WHO-CDS-HIV-18.51. Accessed on August 7, 2018.
Riddell J. 2018 IAS-USA Recommendations for the use of antiretroviral therapy for HIV building decades of progress. JAMA. 2018;320(4):347. https://pubmed.ncbi.nlm.nih.gov/30043044. https://doi.org/10.1001/jama.2018.9184.
Gallant JE, Staszewski S, Pozniak AL, et al. Efficacy and safety of tenofovir DF vs stavudine in combination therapy in antiretroviral-naive patients: A 3-year randomized trial. JAMA. 2004;14;292(2):191-201. https://pubmed.ncbi.nlm.nih.gov/15249568. https://doi.org./10.1001/jama.292.2.191.
Young J, Weber R, Rickenbach M, et. al. Lipid profiles for antiretroviral-naive patients starting PI- and NNRTI-based therapy in the Swiss HIV cohort study. Antivir Ther. 2005;10(5):585-91. https://pubmed.ncbi.nlm.nih.gov/16152752.
Pinto Neto LF, das Neves MB, Ribeiro-Rodrigues R, Page K, Miranda AE. Dyslipidemia and fasting glucose impairment among HIV patients three years after the first antiretroviral regimen in a Brazilian AIDS outpatient clinic. Braz J Infect Dis. 2013;17(4):438-43. https://pubmed.ncbi.nlm.nih.gov/23735423. https://doi.org/10.1016/j.bjid.2012.12.006.
Ofotokun I, Na LH, Landovitz RJ, Ribaudo HJ, McComsey GA, et. al. Comparison of the metabolic effects of ritonavir-boosted darunavir or atazanavir versus raltegravir, and impact of ritonavir plasma exposure: ACTG 5257. Clin Infect Dis. 2015;15;60(12):1842-51. https://pubmed.ncbi.nlm.nih.gov/25767256. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4660025. https://doi.org/10.1093/cid/civ193.
Brown TT, Cole SR, Li X, et. al. Antiretroviral therapy and the prevalence and incidence of diabetes mellitus in the multicenter AIDS cohort study. Arch Intern Med. 2005;165(10):1179-84. https://pubmed.ncbi.nlm.nih.gov/15911733. https://doi.org/10.1001/archinte.165.10.1179.
Domingos H, da Cunha RV, Paniago AMM, Martins DM, Elkhoury EB, De Souza AS. Metabolic effects associated to the highly active antiretroviral therapy in AIDS patients. Braz J Infect Dis. 2009;13(2):130-6. https://pubmed.ncbi.nlm.nih.gov/20140358. https://doi.org/10.1590/s1413-86702009000200012.
Mondy K, Oovertan ET, Grubb J, et. al. Metabolic syndrome in HIV-infected patients from an Urban, Midwestern US outpatient population. Clin Infect Dis. 2007;44(5):726-34. https://pubmed.ncbi.nlm.nih.gov/17278068. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3170426. https://doi.org/10.1086/511679.
Abrahams Z, Dave JA, Maartens G, Levitt NS. Changes in blood pressure, glucose levels, insulin secretion and anthropometry after long term exposure to antiretroviral therapy in South African women. AIDS Res Ther. 2015;12:24. https://pubmed.ncbi.nlm.nih.gov/26251665. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4526419. https://doi.org/10.1186/s12981-015-0065-8.
Van Wijk JP, Cabezas MC. Hypertriglyceridemia, metabolic syndrome, and cardiovascular disease in HIV-infected patients: Effects of antioretroviral therapy and adipose tissue distribution. Int J Vasc Med. 2012;2012:201027. https://pubmed.ncbi.nlm.nih.gov/21876813. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3159991. https://doi.org/10.1155/2012/201027.
Pao V, Lee GA, Grunfeld C. HIV therapy, metabolic syndrome and cardiovascular risk. Curr Atheroscler Rep. 2008;10(1):61-70. https://pubmed.ncbi.nlm.nih.gov/18366987. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3166347. https://doi.org/10.1007/s11883-008-0010-6.
Paula AA, Falcão MCN, Pacheco AG. Metabolic syndrome in HIV-infected individuals: Underlying mechanisms and epidemiological aspects. AIDS Res Ther. 2013;10(1):32. https://pubmed.ncbi.nlm.nih.gov/24330597. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3874610. https://doi.org/10.1186/1742-6405-10-32.
Armstrong C, Liu E, Okuma J, et. al. Dyslipidemia in an HIV-positive, antiretroviral treatment-naïve population in Dar es Salaam, Tanzania. J Acquir Immune Defic Syndr. 2011; 57(2):141–5. https://pubmed.ncbi.nlm.nih.gov/21436713. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3125454. https://doi.org/QAI.0b013e318219a3d1.
Daniyam CA, Iroezindu MO. Lipid profile of anti-retroviral treatment-naive HIV-infected patients in Jos, Nigeria. Ann Med Health Sci Res. 2013;3(1):26-30. https://pubmed.ncbi.nlm.nih.gov/23634325. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3634219. https://doi.org/10.4103/2141-9248.109468.
Singh J, Verma M, Ghalaut PS, Verma R, Soni A, Ghalaut VS. Alteration in lipid profile in treatment-naive HIV-infected patients and changes following HAART initiation in Haryana. J Endocrinol Metab. 2014;4(1-2):25-31.
Yinzhong S, Jiangrong W, Zhenyan W, et. al. Prevalence of dyslipidemia among antiretroviral-naive HIV-infected individuals in China. Medicine (Baltimore). 2015;94(48):e2201. https://pubmed.ncbi.nlm.nih.gov/26632908. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4674211. https://doi.org/10.1097/MD.0000000000002201.
Zephy D, Lakshmi LJ, Ashraff R. Lipid profile among art treated and untreated patients in HIV positive cases. Arch Med. 2015;8:2.
Wang Q, Ding H, Xu J, et. al. Lipids profile among ART-naïve HIV infected patients and men who have sex with men in China: A case control study. Lipids in Health Dis. 2016;15(1):149. https://pubmed.ncbi.nlm.nih.gov/27600391. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5012071. https://doi.org/10.1186/s12944-016-0297-1
Kohli R, Shevitz A, Gorbach S, Wanke C. A randomized placebo-controlled trial of metformin for the treatment of HIV lipodystrophy. HIV Med. 2007;8(7):420-6. https://pubmed.ncbi.nlm.nih.gov/17760733. https://doi.org/10.1111/j.1468-1293.2007.00488.x.
Adewole OO, Eze S, Betiku Y, Anteyi E, Wada I, Ajuwon Z. Lipid profile in HIV/AIDS patients in Nigeria. Afr Health Sci. 2010;10(2):144–149. https://pubmed.ncbi.nlm.nih.gov/21326966. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2956300.
Grunfeld C, Kotler DP, Hamadeh R, Tierney A, Wang J, Pierson RN. Hypertriglyceridemia in the acquired immunodeficiency syndrome. Am J Med. 1989;86(1):27-31. https://pubmed.ncbi.nlm.nih.gov/2910092. https://doi.org/10.1016/0002-9343(89)90225-8.
Shor-Posner G, Basit A, Lu Y, et al. Hypocholesterolemia is associated with immune dysfunction in early human immunodeficiency virus-1 infection. Am J Med. 1993;94(5):515-9. https://pubmed.ncbi.nlm.nih.gov/7605397. https://doi.org/10.1016/0002-9343(93)90087-6.
Coodley G, Coodley MK. Hypocholesterolemia and malabsorption in HIV infection. West J Med. 1991;154(6):735. https://pubmed.ncbi.nlm.nih.gov/1877219. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1002890
Njoroge A. Prevalence and correlates of dyslipidemia among HIV-1 Infected and HIV-1 Uninfected Individuals in Nairobi, Kenya. https://digital.lib.washington.edu/researchworks/handle/1773/26189. Accessed on June 15, 2017.
El-Sadr WM, Mullin CM, Carr A, et. al. Effects of HIV disease on lipid, glucose and insulin levels: Results from a large antiretroviral-naive cohort. HIV Med. 2005;6(2):114–21. https://pubmed.ncbi.nlm.nih.gov/15807717. https://doi.org/10.1111/j.1468-1293.2005.00273.x.
Jantarapakde J, Phanuphak N, Chaturawit C, et. al. Prevalence of metabolic syndrome among antiretroviral- naïve and antiretroviral-experienced HIV-1 infected Thai adults. AIDS Patient Care STDS. 2014;28(7):331-40. https://pubmed.ncbi.nlm.nih.gov/24914459. https://doi.org/10.1089/apc.2013.0294.
Chan JC, Malik V, Jia W, et al. Diabetes in Asia: Epidemiology, risk factors, and pathophysiology. JAMA. 2009;301(20):2129-40. https://pubmed.ncbi.nlm.nih.gov/19470990. https://doi.org/10.1001/jama.2009.726.
Dubé MP, Sprecher D, Henry WK, et. al. Preliminary guidelines for the evaluation and management of dyslipidemia in adults infected with human immunodeficiency virus and receiving antiretroviral therapy: Recommendations of the Adult AIDS Clinical Trial Group Cardiovascular Disease Focus Group. Clin Infect Dis. 2000;31(5):1216-24. https://pubmed.ncbi.nlm.nih.gov/11073755. https://doi.org/10.1086/317429.
Oka F, Naito T, Oike M, et al. Correlation between HIV disease and lipid metabolism in antiretroviral-naïve HIV-infected patients in Japan. J Infect Chemother. 2012;18(1):17–21. https://pubmed.ncbi.nlm.nih.gov/21735099. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3278606. https://doi.org/10.1007/s10156-011-0275-5.
Dave JA, Levitt NS, Ross IL, Lacerda M, Maartens G, Blom D. Anti-retroviral therapy increases the prevalence of dyslipidemia in South African HIV-infected patients. PLoS ONE. 2016;11(3):1-13. https://pubmed.ncbi.nlm.nih.gov/26986065. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4795704. https://doi.org/10.1371/journal.pone.0151911.
Domingo P, Suarez-Lozano I, Teira R, et al. Dyslipidemia and cardiovascular disease risk factor management in HIV-1-infected subjects treated with HAART in the Spanish VACH cohort. Open AIDS J. 2008;2:26–38. https://pubmed.ncbi.nlm.nih.gov/18923695. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2556198. https://doi.org/10.2174/1874613600802010026.
Sinxadi PZ, McIlleron HM, Dave JA, et al. Plasma efavirenz concentrations are associated with lipid and glucose concentrations. Medicine (Baltimore). 2016;95(2):e2385. https://pubmed.ncbi.nlm.nih.gov/26765416. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4718242. https://doi.org/10.1097/MD.0000000000002385.
Schulte-Hermann K, Schalk H, Haider B, et. al. Impaired lipid profile and insulin resistance in a cohort of Austrian HIV patients. J Infect Chemother. 2016;22(4):248-53. https://pubmed.ncbi.nlm.nih.gov/26907935. https://doi.org/10.1016/j.jiac.2016.01.007.
Pérez-Matute P, Pérez-Martinez L, Blanco JR, Oteo JA. Role of mitochondria in HIV infection and associated metabolic disorders: Ffocus on non-alcoholic fatty liver disease and lipodystrophy syndrome. Oxid Med Cell Longev. 2013;2013:493413. https://pubmed.ncbi.nlm.nih.gov/23970949. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3736404. https://doi.org/10.1155/2013/493413.
Liang H, Xie Z, Shen T. Monocyte activation and cardiovascular disease in HIV infection. Cell Mol Immunol. 2017;14(12):960-2. https://pubmed.ncbi.nlm.nih.gov/29082920. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5719136. https://doi.org/10.1038/cmi.2017.109
Rao PV. Persons with type 2 diabetes and co-morbid active tuberculosis should be treated with insulin. Int J Diab Dev Countries. 1999;19:79-86.
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Christian Francisco, Eddieson Gonzales, Marc Gregory Yu, Edsel Maurice Salvaña, Cybele Abad, Paul Ferdinand Reganit, Patricia Maningat, Olivia Sison, Marissa Alejandria

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The full license is at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.










