Glycaemic Changes Among Children and Adolescents With Type 1 Diabetes Mellitus Before and During Ramadan Fasting Using Continuous Glucose Monitoring
DOI:
https://doi.org/10.15605/jafes.037.02.08Keywords:
paediatric, T1DM, CGM, Ramadan fastingAbstract
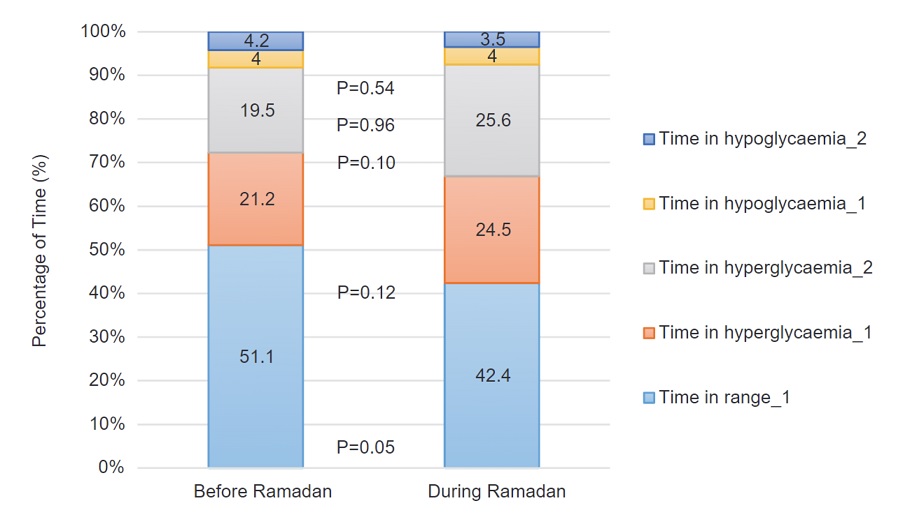
Objectives . This study described and compared glycaemic changes with the use of the following Continuous Glucose Monitoring (CGM) metrics: time in range, time in hyperglycaemia and time in hypoglycaemia from retrospective CGM data among children and adolescents with Type 1 Diabetes Mellitus (T1DM), before and during Ramadan to better understand the impact of fasting during this season.
Methodology. This study was conducted in 2 tertiary centres: Hospital Putrajaya (HPJ) and Hospital Universiti Sains Malaysia (HUSM) from February to May 2020. Muslim T1DM patients between ages 8 to18 who intended to fast during Ramadan were given Ramadan-focused education. CGM iPro2® (Medtronic) was used before and during Ramadan, complemented by finger-prick glucose monitoring or self-monitoring of blood glucose (SMBG).
Results. Of the 32 patients, only 24 (12 female) were analysed. Mean age was 13.6 ± 3.1 years old, mean HbAlc was 9.6 ± 1.9% and mean duration of illness was 5.4 ± 3.4 years. Majority (91.7%) were on multiple dose injections (MDI) while only 8.3% were on continuous subcutaneous insulin infusion (CSII). All fasted in Ramadan without acute complications. Retrospective CGM analysis revealed similar results in time in range (TIR), time in hyperglycaemia and time in hypoglycaemia before and during Ramadan, indicating no increased hypoglycaemic or hyperglycaemic events related to fasting. Glycaemic variability before Ramadan as measured by the LBGI, HBGI and MAG, were similar to values during Ramadan.
Conclusion. Ramadan fasting among T1DM children and adolescents, by itself, is not associated with short-term glycaemic deterioration. T1DM youths can fast safely in Ramadan with the provision of focused education and regular SMBG.
Downloads
References
Holy Quran. Available from https://www.quran-pdf.com/en/
Deeb A, Elbarbary N, Smart CE, et al. ISPAD Clinical Practice Consensus Guidelines: Fasting during Ramadan by young people with diabetes. Pediatr Diabetes. 2020;21(1):5-17. https://pubmed.ncbi.nlm.nih.gov/31659852. https://doi.org/10.1111/pedi.12920.
Hassanein M, Al-Arouj M, Hamdy O, et al. Diabetes and Ramadan: Practical guidelines. Diabetes Res Clin Pract. 2017;126:303-16. https://pubmed.ncbi.nlm.nih.gov/28347497. https://doi.org/10.1016/j.diabres.2017.03.003.
IDF and DAR Alliance. Diabetes and Ramadan Guidelines; 2016. Available from www.idf.org/guidelines/diabetes-in-ramadan.
Guidelines P. Diabetes and Ramadan Diabetes and Ramadan International Diabetes Federation (IDF), in Collaboration with the Diabetes and Ramadan (DAR) International Alliance; 2021. Available from www.idf.org/guidelines/diabetes-in-ramadan
Salti I, Bénard E, Detournay B, et al. A population-based study of diabetes and its characteristics during the fasting month of ramadan in 13 countries: Results of the epidemiology of diabetes and ramadan 1422/2001 (EPIDIAR) study. Diabetes Care. 2004;27(10):2306-11. https://pubmed.ncbi.nlm.nih.gov/15451892 . https://doi.org/10.2337/diacare.27.10.2306.
Al-Arouj M, Bouguerra R, Buse J, et al. Recommendations for management of diabetes during Ramadan. Diabetes Care. 2005;28(9):2305-11. https://pubmed.ncbi.nlm.nih.gov/16123509. https://doi.org/10.2337/diacare.28.9.2305.
Hassanein M, Alamoudi RM, Kallash MA, et al. Ramadan fasting in people with type 1 diabetes during COVID-19 pandemic: The DaR Global survey. Diabetes Res Clin Pract. 2021;172:108626. https://pubmed.ncbi.nlm.nih.gov/33321160. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7836519. https://doi.org/10.1016/j.diabres.2020.108626
El-Hawary A, Salem N, Elsharkawy A, et al. Safety and metabolic impact of Ramadan fasting in children and adolescents with type 1 diabetes. J Pediatr Endocrinol Metab. 2016;29(5):533-41. https://pubmed.ncbi.nlm.nih.gov/26926864. https://doi.org/10.1515/jpem-2015-0263.
Zabeen B, Tayyeb S, Benarjee B, et al. Fasting during Ramadan in adolescents with diabetes. Indian J Endocrinol Metab. 2014;18(1):44-7. https://pubmed.ncbi.nlm.nih.gov/24701429. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3968732. https://doi.org/10.4103/2230-8210.126530.
Al-Khawari M, Al-Ruwayeh A, Al-Doub K, Allgrove J. Adolescents on basal-bolus insulin can fast during Ramadan. Pediatr Diabetes. 2010;11(2):96-100. https://pubmed.ncbi.nlm.nih.gov/19947956 . https://doi.org/10.1111/j.1399-5448.2009.00544.x.
Al-Agha AE, Kafi SE, Aldeen AMZ, Khadwardi RH. Flash glucose monitoring system may benefit children and adolescents with type 1 diabetes during fasting at Ramadan. Saudi Med J. 2017;38(4):366-71. https://pubmed.ncbi.nlm.nih.gov/28397942. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5447188. https://doi.org/10.15537/smj.2017.4.18750.
Lessan N, Hannoun Z, Hasan H, Barakat MT. Glucose excursions and glycaemic control during Ramadan fasting in diabetic patients: Insights from continuous glucose monitoring (CGM). Diabetes Metab. 2015;41(1):28-36. https://pubmed.ncbi.nlm.nih.gov/28397942. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5447188. https://doi.org/10.1016/j.diabet.2014.11.004.
Kaplan W, Afandi B. Blood glucose fluctuation during Ramadan fasting in adolescents with type 1 diabetes: Findings of continuous glucose monitoring. Diabetes Care. 2015;38(10):e162-3. https://pubmed.ncbi.nlm.nih.gov/26294662. https://doi.org/10.2337/dc15-1108.
Lessan N, Hasan H, Barakat MT. Ramadan fasting: A study of changes in glucose profiles among patients with diabetes using continuous glucose monitoring. Diabetes Care. 2012;35(5):2012. https://pubmed.ncbi.nlm.nih.gov/22517945. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3329831. https://doi.org/10.2337/dc11-2037.
Alfadhli EM. Higher rate of hyperglycemia than hypoglycemia during Ramadan fasting in patients with uncontrolled type 1 diabetes: Insight from continuous glucose monitoring system. Saudi Pharm J. 2018;26(7):965-9. https://pubmed.ncbi.nlm.nih.gov/30416354. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6218385. https://doi.org/10.1016/j.jsps.2018.05.006.
Kaplan W, Afandi B, Al Hassani N, Hadi S, Zoubeidi T. Comparison of continuous glucose monitoring in adolescents with type 1 diabetes: Ramadan versus non-Ramadan. Diabetes Res Clin Pract. 2017;134:178-82. https://pubmed.ncbi.nlm.nih.gov/29061323. https:ddoi.org/10.1016/j.diabres.2017.10.010.
Afandi B, Kaplan W, Majd L, Roubi S. Rate, Timing, and severity of hypoglycemia in adolescents with type 1 diabetes during Ramadan fasting: A study with freestyle libre flash glucose monitoring system. Ibnosina J Med Biomed Sci. 2018;10(1):9. https://doi.org/10.4103/ijmbs.ijmbs_73_17.
Fuziah MZ, Hong JYH, Zanariah H, et al. A national database on children and adolescent with diabetes (e-DiCARE): Results from April 2006 to June 2007. Med J Malaysia. 2008;63(Suppl C):37-40. https://pubmed.ncbi.nlm.nih.gov/19230245.
Ministry of Health Malaysia. Quick reference for healthcare providers: Diabetes Mellitus in manegment of nasopharyngeal carcinoma 2016. Putrajaya: MaHTAS Medical Development Ministry of Health Malaysia. https://www.moh.gov.my/moh/resources/Penerbitan/CPG/Kanser/QR Nasopharyngeal Carcinoma.pdf
Danne T, Nimri R, Battelino T, et al. International consensus on use of continuous glucose monitoring. Diabetes Care. 2017;40(12):1631-40. https://pubmed.ncbi.nlm.nih.gov/29162583. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6467165. https://doi.org10.2337/dc17-1600.
Battelino T, Danne T, Bergenstal RM, et al. Clinical targets for continuous glucose monitoring data interpretation: Recommendations from the international consensus on time in range. Diabetes Care. 2019;42(8):1593-1603. https://pubmed.ncbi.nlm.nih.gov/31177185. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6973648. https://doi.org/10.2337/dci19-0028.
Hill NR, Oliver NS, Choudhary P, Levy JC, Hindmarsh P, Matthews DR. Normal reference range for mean tissue glucose and glycemic variability derived from continuous glucose monitoring for subjects without diabetes in different ethnic groups. Diabetes Technol Ther. 2011;13(9):921-8. https://pubmed.ncbi.nlm.nih.gov/21714681. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3160264. https://doi.org/10.1089/dia.2010.0247.
Tang A. "Malaysia announces movement control order after spike in Covid-19 cases (updated)." The Star. March 16, 2020. https://www.thestar.com.my/news/nation/2020/03/16/malaysia-announces-restricted-movement-measure-after-spike-in-covid-19-cases.
Ramadan in Southeast Asia - statistics & facts. Statista; 2022. Available from https://www.statista.com/topics/6329/ramadan-in-southeast-asia/#topicHeader__wrapper.
NIH Ministry of Health Malaysia. National Health and Morbidity Survey 2019: NCDs - Non-Communicable Diseases: Risk factors and other health problems. Vol 1; 2019. Available from http://www.iku.gov.my/nhms-2019.
Insulin pump therapy for type 1 and type 2 diabetes. Putrajaya: MaHTAS Medical Development Ministry of Health Malaysia; 2015. Available from https://www.moh.gov.my/index.php/database_stores/attach_download/347/281.
Malaysia Statistical Handbook 2019. Department of Statistics Malaysia Official Portal; 2019. Available from https://www.dosm.gov.my/v1/index.php?r=column/cthemeByCat&cat=167&bul_id=OWZ0aFZIZmxVOTB3K1pFVjJrZFY2dz09&menu_id=WjJGK0Z5bTk1ZElVT09yUW1tRG41Zz09.
Weik MH. User guide. In: Computer science and communicationd dictionary. Springer, Boston, MA; 2000. https://doi.org/10.1007/1-4020-0613-6_20584.
Vigersky RA, McMahon C. The Relationship of hemoglobin A1C to time-in-range in patients with diabetes. Diabetes Technol Ther. 2019;21(2):81-5. https://pubmed.ncbi.nlm.nih.gov/30575414. https://doi.org/10.1089/dia.2018.0310.
Beck RW, Bergenstal RM, Cheng P, et al. The relationships between time in range, hyperglycemia metrics and HbA1c. J Diabetes Sci Technol. 2019;13(4):614-26. https://pubmed.ncbi.nlm.nih.gov/30636519. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6610606. https://doi.org/10.1177/1932296818822496.
Beck RW, Bergenstal RM, Riddlesworth TD, et al. Validation of time in range as an outcome measure for diabetes clinical trials. Diabetes Care. 2019;42(3):400-5. https://pubmed.ncbi.nlm.nih.gov/30352896. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6905478. https://doi.org/10.2337/dc18-1444.
Martín-Timón I, Del Cañizo-Gómez FJ. Mechanisms of hypoglycemia unawareness and implications in diabetic patients. World J Diabetes. 2015;6(7):912-26. https://pubmed.ncbi.nlm.nih.gov/26185599. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4499525. https://doi.org/10.4239/wjd.v6.i7.912.
Loh HH, Lim LL, Loh HS, Yee A. Safety of Ramadan fasting in young patients with type 1 diabetes: A systematic review and meta-analysis. J Diabetes Investig. 2019;10(6):1490-1501. https://pubmed.ncbi.nlm.nih.gov/30938074. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6825934. https://doi.org/10.1111/jdi.13054.
Alamoudi R, Alsubaiee M, Alqarni A, et al. Comparison of insulin pump therapy and multiple daily injections insulin regimen in patients with type 1 diabetes during ramadan fasting. Diabetes Technol Ther. 2017;19(6):349-54. https://pubmed.ncbi.nlm.nih.gov/28296467. https://doi.org/10.1089/dia.2016.0418
Khalil AB, Beshyah SA, Abu Awad SM, et al. Ramadan fasting in diabetes patients on insulin pump therapy augmented by continuous glucose monitoring: An observational real-life study. Diabetes Technol Ther. 2012;14(9):813-8. https://pubmed.ncbi.nlm.nih.gov/22827507. https://doi.org/10.1089/dia.2012.0061.
Zabeen B, Nahar J, Ahmed B, Islam N, Azad K, Donaghue K. High HbA1c is not a reason not to fast during Ramadan in children, adolescents and young adults with type 1 diabetes – An observational study in Bangladesh. Diabetes Res Clin Pract. 2021;173:108673. https://pubmed.ncbi.nlm.nih.gov/33539866. https://doi.org/10.1016/j.diabres.2021.108673.
Department of Statistics Malaysia. House income basic amenities survey report 2019 [Laporan Survei Pendapatan Isi Rumah dan Kemudahan Asas 2019]; 2020. Available from https://www.dosm.gov.my/v1/index.php?r=column/cthemeByCat&cat=120&bul_id=TU00TmRhQ1N5TUxHVWN0T2VjbXJYZz09&menu_id=amVoWU54UTl0a21NWmdhMjFMMWcyZz09.
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Sze Teik Teoh

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The full license is at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.










