Prevalence of Metabolic Syndrome and its Associated Risk Factors in Pediatric Obesity
DOI:
https://doi.org/10.15605/jafes.037.01.05Keywords:
prevalence, metabolic syndrome, risk factors, obese childrenAbstract
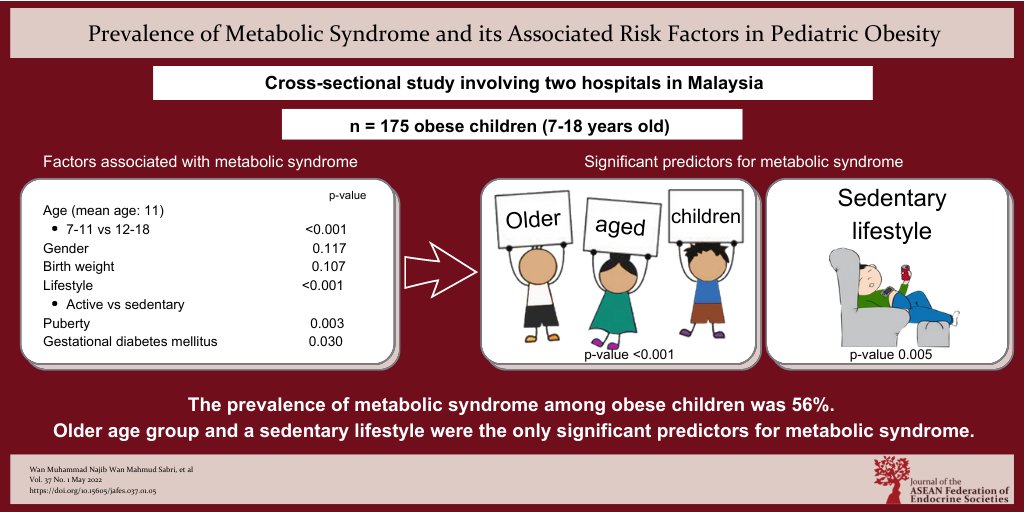
Objective. We aimed to study the prevalence of metabolic syndrome (MetS) and the factors associated with metabolic syndrome among obese children.
Methodology. We recruited 175 subjects, aged 7 to 18 years old, referred for obesity. We studied their demography (age, gender, ethnicity, family background), performed clinical/auxological examinations [weight, height, body mass index (BMI), waist circumference (WC), blood pressure (BP)], and analyzed their biochemical risks associated with metabolic syndrome [fasting plasma glucose (FPG), fasting lipid profile (FLP), fasting insulin, liver function tests (LFT)]. MetS was identified according to the criteria proposed by the International Diabetes Federation (IDF) for pediatric obesity. Multiple logistic regression models were used to examine the associations between risk variables and MetS.
Results. The prevalence of metabolic syndrome among children with obesity was 56% (95% CI: 48.6 to 63.4%), with a mean age of 11.3 ± 2.73 years. Multiple logistic regression analysis showed age [adjusted odds ratio (OR) 1.27, 95% CI: 1.15 to 1.45] and sedentary lifestyle (adjusted OR 3.57, 95% CI: 1.48 to 8.59) were the significant factors associated with metabolic syndrome among obese children.
Conclusion. The prevalence of metabolic syndrome among obese children referred to our centers was 56%. Older age group, male gender, birth weight, sedentary lifestyle, puberty and maternal history of gestational diabetes mellitus (GDM) were found to be associated with MetS. However, older age group and sedentary lifestyle were the only significant predictors for metabolic syndrome.
Downloads
References
World Health Organization. Obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed May 2020.
Gupta N, Shah P, Nayyar S, Misra A. Childhood obesity and the metabolic syndrome in developing countries. Indian J Pediatr. 2013;80(Suppl 1):S28-37. https://pubmed.ncbi.nlm.nih.gov/23334584. https://doi.org/10.1007/s12098-012-0923-5.
Organisation for Economic Cooperation and Development and the World Health Organization. Health at a Glance: Asia/Pacific 2020. Measuring Progress Towards Universal Health Coverage. Paris: OECD Publishing, 2020. https://doi.org/10.1787/26b007cd-en.
Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2-19 years: United States, 1963-1965 through 2017-2018. National Center for Health Statistics Health E-Stats. 2020. https://www.cdc.gov/nchs/data/hestat/obesity-child-17-18/obesity-child.htm.
Strock GA, Cottrell ER, Abang AE, Buschbacher RM, Hannon TS. Childhood obesity: A simple equation with complex variables. J Long Term Eff Med Implants. 2005;15(1):15-32. https://pubmed.ncbi.nlm.nih.gov/15715513. https://doi.org/10.1615/jlongtermeffmedimplants.v15.i1.30.
Sangun Ö, Dündar B, Köşker M, Pirgon Ö, Dündar N. Prevalence of metabolic syndrome in obese children and adolescents using three different criteria and evaluation of risk factors. J Clin Res Pediatr Endocrinol. 2011;3(2):70-6. https://pubmed.ncbi.nlm.nih.gov/21750635. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3119444. https://doi.org/10.4274/jcrpe.v3i2.15.
Weiss R, Dziura J, Burgert TS, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004;350(23):2362-74. https://doi.org/10.1056/NEJMoa031049.
Ford ES, Li C, Zhao G, Pearson WS, Mokdad AH. Prevalence of the metabolic syndrome among U.S. adolescents using the definition from the International Diabetes Federation. Diabetes Care. 2008;31(3):587-9. https://pubmed.ncbi.nlm.nih.gov/18071007. https://doi.org/10.2337/dc07-1030.
Poh BK, Ng BK, Siti Haslinda MD, et al. Nutritional status and dietary intakes of children aged 6 months to 12 years: Findings of the Nutrition Survey of Malaysian Children (SEANUTS Malaysia). Br J Nutr. 2013;110(Suppl 3):S21-35. https://pubmed.ncbi.nlm.nih.gov/24016764. https://doi.org/10.1017/S0007114513002092.
Institute for Public Health, Ministry of Health Malaysia. National Health and Morbidity Survey 2015 (NHMS 2015). Vol. II: Non-communicable diseases, risk factors and other health problems. https://www.moh.gov.my/moh/resources/nhmsreport2015vol2.pdf
Fadzlina AA, Harun F, Nurul Haniza MY, et al. Metabolic syndrome among 13 year old adolescents: Prevalence and risk factors. BMC Public Health. 2014;14(Suppl 3):S7. https://pubmed.ncbi.nlm.nih.gov/25437226. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4251137. https://doi.org/10.1186/1471-2458-14-S3-S7.
Mohd Nasir MT, Nurliyana AR, Norimah AK, et al. Consumption of ready-to-eat cereals (RTEC) among Malaysian children and association with socio-demographic and nutrient intakes: Findings from the MyBreakfast study. Food Nutr Res. 2017;61(1):1304692. https://pubmed.ncbi.nlm.nih.gov/28469545. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5404428. https://doi.org/10.1080/16546628.2017.1304692.
Food and Nutrition Research Institute, Department of Science and Technology. Philippine Nutrition Facts & Figures 2005. Nutritional status of Filipino children and selected population groups: 2005 update.
Jitnarin N, Kosulwat V, Rojroongwasinkul N, Boonpraderm A, Haddock CK, Poston WSC. Prevalence of overweight and obesity in Thai population: Results of the National Thai Food Consumption Survey. Eat Weight Disord. 2011;16(4):e242-9. https://pubmed.ncbi.nlm.nih.gov/22526130. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5824639. https://doi.org/10.1007/BF03327467.
Nguyen PVN, Hong TK, Hoang T, Nguyen DT, Robert AR. High prevalence of overweight among adolescents in Ho Chi Minh City, Vietnam. BMC Public Health. 2013;13:141. https://pubmed.ncbi.nlm.nih.gov/23414441. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3598401. https://doi.org/10.1186/1471-2458-13-141.
Agirbasli M, Tanrikulu AM, Berenson GS. Metabolic syndrome: Bridging the gap from childhood to adulthood. Cardiovasc Ther. 2016;34(1):30-6. https://pubmed.ncbi.nlm.nih.gov/26588351. https://doi.org/10.1111/1755-5922.12165.
Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1988;37(12):1595-607. https://pubmed.ncbi.nlm.nih.gov/3056758. https://doi.org/10.2337/diab.37.12.1595.
Andrabi SMS, Bhat MH, Andrabi SRS, et al. Prevalence of metabolic syndrome in 8-18-year-old school-going children of Srinagar City of Kashmir India. Indian J Endocrinol Metab. 2013;17(1):95-100. https://pubmed.ncbi.nlm.nih.gov/23776859. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3659914. https://doi.org/10.4103/2230-8210.107812.
Lim KG, Cheah WK. A review of metabolic syndrome research in Malaysia. Med J Malaysia. 2016;71(Suppl 1):20-8. https://pubmed.ncbi.nlm.nih.gov/27801385.
Wee BS, Poh BK, Bulgiba A, Ismail MN, Ruzita AT, Hills AP. Risk of metabolic syndrome among children living in metropolitan Kuala Lumpur: A case control study. BMC Public Health. 2011;11:333. https://pubmed.ncbi.nlm.nih.gov/21592367. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3111384. https://doi.org/10.1186/1471-2458-11-333.
Weiss R, Dziura J, Burgert TS, Tamborlane WV, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004;350(23):2362-74. MID: 15175438. https://doi.org/10.1056/NEJMoa031049. P
Šimunović M, Božić J, Milić L, Unić I, Škrabić V. The prevalence of metabolic syndrome and cardiovascular risk factors in obese children and adolescents in Dalmatia: A hospital-based study. Int J Endocrinol. 2016;2016:1823561. https://pubmed.ncbi.nlm.nih.gov/27752263. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5056285. https://doi.org/10.1155/2016/1823561.
Friend A, Craig L, Turner S. The prevalence of metabolic syndrome in children: A systematic review of the literature. Metab Syndr Relat Disord. 2013;11(2):71-80. https://pubmed.ncbi.nlm.nih.gov/23249214. https://doi.org/10.1089/met.2012.0122.
Yee KT, Thwin T, Khin E, et al. Metabolic syndrome in obese and normal weight Myanmar children. J ASEAN Fed Endocr Soc. 2013;28(1):52-5. https://doi.org/10.15605/jafes.028.01.10
Saffari F, Jalilolghadr S, Esmailzadehha N, Azinfar P. Metabolic syndrome in a sample of the 6- to 16-year-old overweight or obese pediatric population: A comparison of two definitions. Ther Clin Risk Manag. 2012;8:55-63. https://pubmed.ncbi.nlm.nih.gov/22346358. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3277872. https://doi.org/10.2147/TCRM.S26673.
Fu JF, Liang L, Zou CC, et al. Prevalence of the metabolic syndrome in Zhejiang Chinese obese children and adolescents and the effect of metformin combined with lifestyle intervention. Int J Obes (Lond). 2007;31(1):15-22. https://pubmed.ncbi.nlm.nih.gov/16953257. https://doi.org/10.1038/sj.ijo.0803453.
Taha D, Ahmed O, bin Sadiq B. The prevalence of metabolic syndrome and cardiovascular risk factors in a group of obese Saudi children and adolescents: A hospital-based study. Ann Saudi Med. 2009;29(5):357-60. https://pubmed.ncbi.nlm.nih.gov/19700892. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3290052. https://doi.org/10.4103/0256-4947.55164.
Sen Y, Kandemir N, Alikasifoglu A, Gonc N, Ozon A. Prevalence and risk factors of metabolic syndrome in obese children and adolescents: The role of the severity of obesity. Eur J Pediatr. 2008;167(10):1183-9. https://pubmed.ncbi.nlm.nih.gov/18205011. https://doi.org/10.1007/s00431-007-0658-x.
Cruz ML, Weigensberg MJ, Huang TTK, Ball G, Shaibi GQ, Goran MI. The metabolic syndrome in overweight Hispanic youth and the role of insulin sensitivity. J Clin Endocrinol Metab. 2004;89(1):108-13. https://pubmed.ncbi.nlm.nih.gov/14715836. https://doi.org/10.1210/jc.2003-031188.
Mohsin F, Baki A, Nahar J, et al. Prevalence of metabolic syndrome among obese children and adolescents. BIRDEM Medical Journal. 2012;1(1):21-5. https://doi.org/10.3329/birdem.v1i1.12382.
Caceres M, Teran CG, Rodriguez S, Medina M. Prevalence of insulin resistance and its association with metabolic syndrome criteria among Bolivian children and adolescents with obesity. BMC Pediatr. 2008;8:31. https://pubmed.ncbi.nlm.nih.gov/18700035. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2526992. https://doi.org/10.1186/1471-2431-8-31.
Dejavitte RAS, Enes CC, Nucci LB. Prevalence of metabolic syndrome and its associated factors in overweight and obese adolescents. J Pediatr Endocrinol Metab. 2020;33(2):233-9. https://pubmed.ncbi.nlm.nih.gov/31804963. https://doi.org/10.1515/jpem-2019-0369.
You MA, Son YJ. Prevalence of metabolic syndrome and associated risk factors among Korean adolescents: Analysis from the Korean national survey. Asia Pac J Public Health. 2012;24(3):464-71. https://pubmed.ncbi.nlm.nih.gov/21527432. https://doi.org/10.1177/1010539511406105.
Tchernof A, Després JP. Pathophysiology of human visceral obesity: An update. Physiol Rev. 2013;93(1):359-404. https://pubmed.ncbi.nlm.nih.gov/23303913. https://doi.org/10.1152/physrev.00033.2011.
Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005;365(9468):1415-28. https://pubmed.ncbi.nlm.nih.gov/15836891. https://doi.org/10.1016/S0140-6736(05)66378-7.
Quah YVJ, Poh BK, Ismail MN. Metabolic syndrome based on IDF criteria in a sample of normal weight and obese school children. Malays J Nutr. 2010;16(2):207-17. https://pubmed.ncbi.nlm.nih.gov/22691926.
Tam WH, Ma RCW, Yang X, et al. Glucose intolerance and cardiometabolic risk in children exposed to maternal gestational diabetes mellitus in utero. Pediatrics. 2008; 122(6):1229-34. https://pubmed.ncbi.nlm.nih.gov/19047239. https://doi.org/10.1542/peds.2008-0158.
Boney CM, Verma A, Tucker R, Vohr BR. Metabolic syndrome in childhood: Association with birth weight, maternal obesity, and gestational diabetes mellitus. Pediatrics. 2005;115(3):e290-6. https://pubmed.ncbi.nlm.nih.gov/15741354. https://doi.org/10.1542/peds.2004-1808.
Luna AM, Wilson DM, Wibbelsman CJ, et al. Somatomedins in adolescence: A cross-sectional study of the effect of puberty on plasma insulin-like growth factor I and II levels. J Clin Endocrinol Metab. 1983;57(2):268-71. https://pubmed.ncbi.nlm.nih.gov/6345568. https://doi.org/10.1210/jcem-57-2-268.
Daughaday WH, Rotwein P. Insulin-like growth factors I and II. Peptide, messenger ribonucleic acid and gene structures, serum, and tissue concentrations. Endocr Rev. 1989;10(1):68-91. https://pubmed.ncbi.nlm.nih.gov/2666112. https://doi.org/10.1210/edrv-10-1-68.
Rabinowitz D, Klassen GA, Zierler KL. Effect of human growth hormone on muscle and adipose tissue metabolism in the forearm of man. J Clin Invest. 1965;44(1):51-61. https://pubmed.ncbi.nlm.nih.gov/14254256. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC442018. https://doi.org/10.1172/JCI105126.
Moran A, Jacobs DRJ, Steinberger J, et al. Changes in insulin resistance and cardiovascular risk during adolescence: Establishment of differential risk in males and females. Circulation. 2008;117(18):2361-8. https://pubmed.ncbi.nlm.nih.gov/18427135. https://doi.org/10.1161/CIRCULATIONAHA.107.704569.
Moran A, Jacobs DRJ, Steinberger J, et al. Insulin resistance during puberty: Results from clamp studies in 357 children. Diabetes. 1999;48(10):2039-44. https://pubmed.ncbi.nlm.nih.gov/10512371. https://doi.org/10.2337/diabetes.48.10.2039.
Siwarom S, Aekplakorn W, Pirojsakul K, et al. Metabolic syndrome in Thai adolescents and associated factors: The Thai National Health Examination Survey V (NHES V). BMC Public Health. 2021;21(1):678. https://pubmed.ncbi.nlm.nih.gov/33827482. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8028250. https://doi.org/10.1186/s12889-021-10728-6.
Zurlo F, Larson K, Bogardus C, Ravussin E. Skeletal muscle metabolism is a major determinant of resting energy expenditure. J Clin Invest. 1990;86(5):1423-7. https://pubmed.ncbi.nlm.nih.gov/2243122. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC296885. https://doi.org/10.1172/JCI114857.
Holloszy JO, Coyle EF. Adaptations of skeletal muscle to endurance exercise and their metabolic consequences. J Appl Physiol Respir Environ Exerc Physiol. 1984;56(4):831-8. https://pubmed.ncbi.nlm.nih.gov/6373687. https://doi.org/10.1152/jappl.1984.56.4.831.
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Wan Muhammad Najib Wan Mahmud Sabri, Rashdan Zaki Mohamed, Najib Majdi Yaacob, Suhaimi Hussain

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The full license is at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.










