Clinicodemographic Profile and Outcomes of Type 2 Diabetes Mellitus in the Indonesian Cohort of DISCOVER
A 3-Year Prospective Cohort Study
DOI:
https://doi.org/10.15605/jafes.038.01.10Keywords:
diabetes type 2, vascular complications, real-world study, IndonesiaAbstract
Background. Indonesia is amongst the top 10 countries with the highest prevalence of Type 2 Diabetes Mellitus (T2DM) at 10.8%. However, the distinguishable features of T2DM in Indonesia remain obscure. Therefore, the DISCOVER study aimed to describe the characteristics of T2DM patients, associated vascular complications and treatment in Indonesia.
Methodology. DISCOVER study is a multi-country, multicenter, prospective, cohort study over 3 years. In the present study, the data were collected from 13 sites from clinical practice, hospitals and public health facilities in Indonesia.
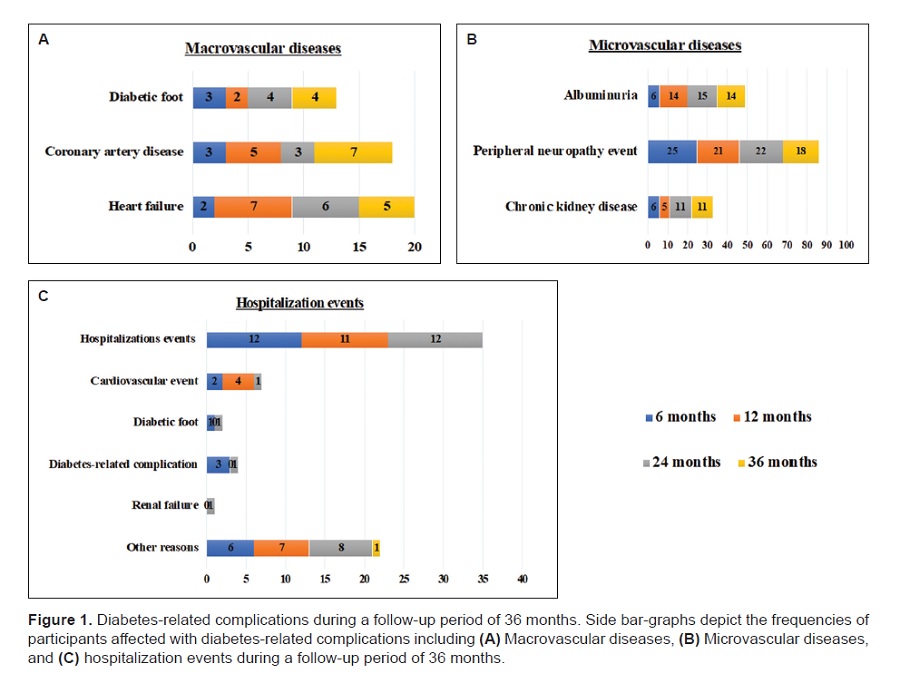
Results. A total of 221 subjects were recruited with a mean age of 55.6 ± 9.8 years and body mass index (BMI) of 26.4 ± 4.4 kg/m2. Over 40% of patients had hypertension and/or hyperlipidemia. The mean duration of T2DM was 58.3 ± 62.0 months while the mean HbA1c levels was 9.2 ± 2%. In total, 82.4% completed the study within a 36-month follow-up period. BMI remained elevated i.e., >25 kg/m2. A significant reduction was observed in HbA1c levels as compared to baseline (9.2 ± 2% to 8.1 ± 1.8%). T2DM-associated microvascular complications such as peripheral neuropathy, albuminuria and chronic kidney disease were observed in 17.2%. Macrovascular complications including coronary artery disease and heart failure were seen in 26.2% of patients. We also found that more than 70% of patients were on metformin and/or sulfonylurea.
Conclusion. The features of patients with T2DM in Indonesia were high BMI, with hypertension and hyperlipidemia as co-morbidities. Metformin and sulfonylureas were the most common treatment. HbA1c reduction during follow-up did not reach recommended target. Thus, early detection and intervention using available glucose-lowering medications and aggressive management of risk factors and complications are essential to improve outcomes of diabetes management
in Indonesia.
Downloads
References
International Diabetes Federation. IDF Diabetes Atlas. 10th edition. Brussels; 2021.
Indonesia KKR. Hasil Utama Riset Kesehatan Dasar (RISKESDAS); 2018. https://kesmas.kemkes.go.id/assets/upload/dir_519d41d8cd98f00/files/Hasil-riskesdas-2018_1274.pdf.
PERKENI. Pedoman Pengelolaan dan Pencegahan Diabetes melitus Tipe 2 Dewasa di Indonesia: PB PERKENI; 2021. https://pbperkeni.or.id/wp-content/uploads/2021/11/22-10-21-Website-Pedoman-Pengelolaan-dan-Pencegahan-DMT2-Ebook.pdf.
American Diabetes Association. Introduction: Standard of Medical Care in Diabetes - 2022. Diabetes Care. 2022;45(Suppl 1):S1-2.
Kosiborod M, Gomes MB, Nicolucci A, et al. Vascular complications in patients with type 2 diabetes: Prevalence and associated factors in 38 countries (the DISCOVER study program). Cardiovasc Diabetol. 2018;17(1):150. https://pubmed.ncbi.nlm.nih.gov/30486889. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6260731. https://doi.org/10.1186/s12933-018-0787-8.
Cholil AR, Lindarto D, Pemayun TGD, Wisnu W, Kumala P, Puteri HHS. DiabCare Asia 2012: Diabetes management, control, and complications in patients with type 2 diabetes in Indonesia. Med J Indones. 2019;28(1):47-56. https://doi.org/10.13181/mji.v28i1.2931.
Milibari AA, Matuure EY, Gadah EM. Prevalence, determinants and prevention of type 2 diabetes mellitus (T2DM) in Arabic countries: A systematic review study. Health Sci J. 2020;14(2):1-8.
Colosia AD, Palencia R, Khan S. Prevalence of hypertension and obesity in patients with type 2 diabetes mellitus in observational studies: A systematic literature review. Diabetes Metab Syndr Obes. 2013;6:327-38. https://pubmed.ncbi.nlm.nih.gov/24082791. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3785394. https://doi.org/10.2147/DMSO.S51325.
Haddad JA, Al Hyari MA, Al Momani MS, Al Omari AA, Ammari FL, Annabi FO. Baseline characteristics and treatment pattern of type 2 diabetes patients in Jordan: Analysis from the DISCOVER patient population. Alexandria J Med. 2020;56(1):51-5. https://doi.org/10.1080/20905068.2020.1747733.
Gomes MB, Rathmann W, Charbonnel B, et al. Treatment of type 2 diabetes mellitus worldwide: Baseline patient characteristics in the global DISCOVER study. Diabetes Res Clin Pract. 2019;151:20-32. https://pubmed.ncbi.nlm.nih.gov/30904743. https://doi.org/10.1016/j.diabres.2019.03.024.
Nicolucci A, Charbonnel B, Gomes MB, et al. Treatment patterns and associated factors in 14 668 people with type 2 diabetes initiating a second-line therapy: Results from the global DISCOVER study programme. Diabetes Obes Metab. 2019;21(11):2474-85. https://pubmed.ncbi.nlm.nih.gov/31297947. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6852520. https://doi.org/10.1111/dom.13830.
Soewondo P, Soegondo S, Suastika K, Pranoto A, Soeatmadji DW, Tjokroprawiro A. The DiabCare Asia 2008 study - Outcomes on control and complications of type 2 diabetic patients in Indonesia. Med J Indones. 2010;19(4):235-44. https://doi.org/10.13181/mji.v19i4.412.
Paul SK, Klein K, Thorsted BL, Wolden ML, Khunti K. Delay in treatment intensification increases the risks of cardiovascular events in patients with type 2 diabetes. Cardiovasc Diabetol. 2015;14:100. https://pubmed.ncbi.nlm.nih.gov/26249018. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4528846. https://doi.org/10.1186/s12933-015-0260-x.
(PERNEFRI) PNI. First Report of Indonesian Renal Registry. Indonesia: Perkumpulan Nefrologi Indonesia (PERNEFRI); 2018. https://www.indonesianrenalregistry.org/data/IRR%202018.pdf.
Cavender MA, Norhammar A, Birkeland KI, et al. SGLT-2 inhibitors and cardiovascular risk: An analysis of CVD-REAL. J Am Coll Cardiol. 2018;71(22):2497-506. https://pubmed.ncbi.nlm.nih.gov/29852973. https://doi.org/10.1016/j.jacc.2018.01.085.
Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644-57. https://pubmed.ncbi.nlm.nih.gov/28605608. https://doi.org/10.1056/NEJMoa1611925.
Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380(4):347-57. https://pubmed.ncbi.nlm.nih.gov/30415602. https://doi.org/10.1056/NEJMoa1812389.
Leiter LA, Cefalu WT, de Bruin TW, et al. Long-term maintenance of efficacy of dapagliflozin in patients with type 2 diabetes mellitus and cardiovascular disease. Diabetes Obes Metab. 2016;18(8):766-74. https://pubmed.ncbi.nlm.nih.gov/27009868. https://doi.org/10.1111/dom.12666.
Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117-28. https://pubmed.ncbi.nlm.nih.gov/26378978. https://doi.org/10.1056/NEJMoa1504720.
Gregg EW, Sattar N, Ali MK. The changing face of diabetes complications. Lancet Diabetes Endocrinol. 2016;4(6):537-47. https://pubmed.ncbi.nlm.nih.gov/27156051. https://doi.org/10.1016/S2213-8587(16)30010-9.
Wilkinson E, Randhawa G, Farrington K, et al. Lack of awareness of kidney complications despite familiarity with diabetes: A multi-ethnic qualitative study. J Ren Care. 2011;37(1):2-11. https://pubmed.ncbi.nlm.nih.gov/21288311. https://doi.org/10.1111/j.1755-6686.2011.00199.x.
Zhuo X, Zhang P, Hoerger TJ. Lifetime direct medical costs of treating type 2 diabetes and diabetic complications. Am J Prev Med. 2013;45(3):253-61. https://pubmed.ncbi.nlm.nih.gov/23953350. https://doi.org/10.1016/j.amepre.2013.04.017.
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Djoko Wahono Soeatmadji, Rulli Rosandi, Made Ratna Saraswati, Roy Panusunan Sibarani, Widya Oktaviana Tarigan

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The full license is at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.










