Critical Illness-Related Corticosteroid Insufficiency (CIRCI) among Patients with COVID-19 at a Tertiary Hospital
Clinical Characteristics and Outcomes
DOI:
https://doi.org/10.15605/jafes.038.01.02Keywords:
adrenal insufficiency, COVID-19, critical illness, shockAbstract
Objectives. Among critically ill patients, there is usually impairment of the hypothalamic-pituitary- adrenal axis, leading to a condition known as critical illness-related corticosteroid insufficiency (CIRCI). The aims of this investigation are to determine the incidence of and characterize CIRCI among patients with COVID-19 as well as to analyze the outcomes of these critically ill patients.
Methodology . This is a single-center, retrospective, cohort study that investigated the occurrence of CIRCI among critically ill patients infected with COVID-19.
Results. In this cohort, there were 145 COVID-19 positive patients with refractory shock included, which reflects that 22.94% of the COVID-19 admissions have probable CIRCI.
Patients who were given corticosteroids were found to have statistically significant longer median days on ventilator (p= 0.001). However, those on the corticosteroid arm were at higher risk of morbidity and mortality and a greater proportion of patients with organ dysfunction.
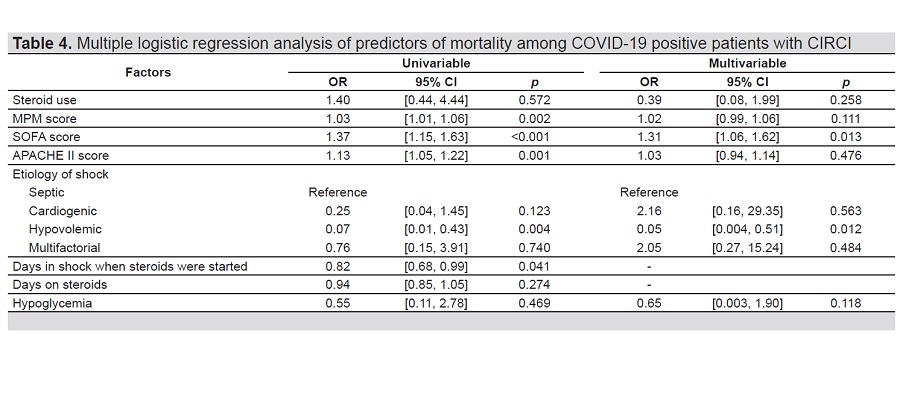
Multivariable logistic regression analysis revealed that SOFA score was a significant predictor of mortality in CIRCI (p=0.013).
Conclusion. CIRCI has a unique presentation among COVID-19 patients because of the presence of a high level of inflammation in this life-threatening infection. It possibly is a harbinger of markedly increased risk of mortality in these patients.
Downloads
References
Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061-9. https://pubmed.ncbi.nlm.nih.gov/32031570. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7042881. https://doi.org/10.1001/jama.2020.1585.
COVID-19: Case tracker. Department of Health. 2020. Accessed May 25, 2021. https://doh.gov.ph/covid19tracker
Zhou W, Liu Y, Tian D, et al. Potential benefits of precise corticosteroids therapy for severe 2019-nCoV pneumonia. Sig Transduct Target Ther. 2020;5(1): 18. https://pubmed.ncbi.nlm.nih.gov/32296012. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7035340. https://doi.org/10.1038/s41392-020-0127-9.
Interim guidelines on the clinical management of adult patients with suspected or confirmed COVID-19 Infection Version 3.1. Philippine Society for Microbiology and Infectious Diseases. 2020. Accessed May 25, 2021 . https://www.psmid.org/interim-management-guidelines-for-covid-19-version-3-1/.
Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. https://pubmed.ncbi.nlm.nih.gov/31986264. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7159299. https://doi.org/10.1016/S0140-6736(20)30183-5.
Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020; 395(10229):1054-62. https://pubmed.ncbi.nlm.nih.gov/32171076. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7270627. https://doi.org/10.1016/S0140-6736(20)30566-3.
Rivas M, Sotello D. Critical illness-related corticosteroid insufficiency: What we know and what we don’t know. Southwest Respir Crit Care Chron. 2019;7(31):44-8. https://doi.org/10.12746/swrccc.v7i31.595.
Ok YJ, Lim JY, Jung SH. Critical illness-related corticosteroid insufficiency in patients with low cardiac output syndrome after cardiac surgery. Korean J Thorac Cardiovasc Surg. 2018;51(2):109-113. https://pubmed.ncbi.nlm.nih.gov/29662808. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5894574. https://doi.org/10.5090/kjtcs.2018.51.2.109.
Cutillar CS, Ramirez J, Ardena JR, Lantion-Ang L, Jimeno C, Laurel MT. Prevalence of adrenal insufficiency using random cortisol level among patients with sepsis and septic shock admitted at the Philippine General Hospital; 2005. [Unpublished].
Annane D, Pastores SM, Rochwerg B, et al. Guidelines for the diagnosis
and management of critical illness-related corticosteroid insufficiency (CIRCI) in critically ill patients (Part I): Society of Critical Care Medicine (SCCM) and European Society of Intensive Care Medicine (ESICM) 2017. Intensive Care Med. 2017;43(12):1751–63. https://pubmed.ncbi.nlm.nih.gov/28940011. https://doi.org/10.1007/s00134-017-4919-5.
Huang X, Hu W, He X, Zhang G. A potential diagnostic protocol for critical illness-related corticosteroid insufficiency (CIRCI) in critically ill patients. J Emerg Crit Care Med. 2018;2:86. https://doi.org/10.21037/jeccm.2018.10.11.
Annane D, Pastores SM, Arlt W, et al. Critical illness-related corticosteroid insufficiency (CIRCI): A narrative review from a Multispecialty Task Force of the Society of Critical Care Medicine (SCCM) and the European Society of Intensive Care Medicine (ESICM). Crit Care Med. 2017;45(12):2089-98. https://pubmed.ncbi.nlm.nih.gov/28938251. https://10.1097/CCM.0000000000002724.
Ariani F, Liu K, Jing Z, Qu J. Glucocorticosteroid in treatment of severe pneumonia. Mediators Inflamm. 2013;2013:865635. https://pubmed.ncbi.nlm.nih.gov/24363503. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3865735. https://doi.org/10.1155/2013/865635.
Prina, E., Ceccato, A. & Torres, A. New aspects in the management of pneumonia. Crit Care. 2016;20(1):267. https://pubmed.ncbi.nlm.nih.gov/27716262. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5045574. https://doi.org/10.1186/s13054-016-1442-y.
Nedel WL, Nora DG, Salluh JI, Lisboa T, Póvoa P. Corticosteroids for severe influenza pneumonia: A critical appraisal. World J Crit Care Med. 2016;5(1):89–95. https://pubmed.ncbi.nlm.nih.gov/26855898. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4733461. https://doi.org/10.5492/wjccm.v5.i1.89.
Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180(7):934–43. https://pubmed.ncbi.nlm.nih.gov/32167524. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7070509. https://doi.org/10.1001/jamainternmed.2020.0994.
Ma S, Xu C, Liu S, et al. Efficacy and safety of systematic corticosteroids among severe COVID-19 patients: A systematic review and meta-analysis of randomized controlled trials. Sig Transduct Target Ther. 2021;6(1):83. https://pubmed.ncbi.nlm.nih.gov/33612824. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7897363. https://doi.org/10.1038/s41392-021-00521-7.
Ducrocq N, Biferi P, Girerd N, et al. Critical illness-related corticosteroid insufficiency in cardiogenic shock patients: Prevalence and prognostic role. Shock. 2018 Oct;50(4):408-13. https://pubmed.ncbi.nlm.nih.gov/29280926. https://doi.org/10.1097/SHK.0000000000001090.
Llewelyn H, Ang HA, Lewis K, Al-Abdullah A. Oxford Handbook of Clinical Diagnosis, 3rd ed. United Kingdom: Oxford University Press; 2014.
Public health surveillance for COVID-19: Interim guidance. World Health Organization. 2020. https://www.who.int/publications/i/item/WHO-2019-nCoV-SurveillanceGuidance-2022.1. Accessed May 25, 2021.
Venkatesh B, Finfer S, Cohen J, et al. Adjunctive glucocorticoid therapy in patients with septic shock. N Engl J Med. 2018;378(9):797–808. https://pubmed.ncbi.nlm.nih.gov/29347874. https://doi.org/10.1056/NEJMoa1705835.
Lee SM, An WS. New clinical criteria for septic shock: Serum lactate level as a new emerging vital sign. J Thorac Dis. 2016;8(7):1388-90. https://pubmed.ncbi.nlm.nih.gov/27501243. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4958885. https://doi.org/10.21037/jtd.2016.05.55.
Jones AE, Trzeciak S, Kline JA. The sequential organ failure assessment score for predicting outcomes in patients with severe sepsis and evidence of hypoperfusion at the time of emergency department presentation. Crit Care Med. 2009;37(5):1649-54. https://pubmed.ncbi.nlm.nih.gov/19325482. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2703722. https://doi.org/10.1097/CCM.0b013e31819def97.
Mao Y, Xu B, Guan W, et al. The adrenal cortex, an underestimated site of SARS-CoV-2 infection. Front Endocrinol (Lausanne). 2021;11:593179. https://pubmed.ncbi.nlm.nih.gov/33488517. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7820749. https://doi.org/10.3389/fendo.2020.593179.
Philippine Living Clinical Practice Guidelines for COVID-19. Philippine Society for Microbiology and Infectious Diseases. 2022. Accessed June 30, 2022. https://www.psmid.org/philippine-covid-19-living-recommendations-3/.
Li Y, Meng Q, Rao X, et al. Corticosteroid therapy in critically ill patients with COVID-19: A multicenter, retrospective study. Crit Care. 2020; 24(1):698. https://pubmed.ncbi.nlm.nih.gov/33339536. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7747001. https://doi.org/10.1186/s13054-020-03429-w.
Pal R, Banerjee M, Bhadada SK. Cortisol concentrations and mortality from COVID-19. Lancet Diabetes Endocrinol. 2020;8(10): 809. https://pubmed.ncbi.nlm.nih.gov/32946817. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7491987. https://doi.org/10.1016/S2213-8587(20)30304-1.
Arcellana AES, Lim KWO, Arcegono, MS, Jimeno, CA. Pilot testing of a protocol for critical illness-related corticosteroid insufficiency at a tertiary hospital. 2020. [Unpublished].
Heidarpour M, Vakhshoori M, Abbasi S, Shafie D, Rezaei N. Adrenal insufficiency in coronavirus disease 2019: A case report. J Med Case Rep. 2020;14(1):134. https://pubmed.ncbi.nlm.nih.gov/32838801. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7444179. https://doi.org/10.1186/s13256-020-02461-2.
Tan T, Khoo B, Mills EG, et al. Association between high serum total cortisol concentrations and mortality from COVID-19. Lancet Diabetes Endocrinol. 2020;8(8):659-60. https://pubmed.ncbi.nlm.nih.gov/32563278. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7302794. https://doi.org/10.1016/S2213-8587(20)30216-3.
Honore Pm, Redant S, Preseau T, et al. Understanding the underlying mechanisms of hyponatremia in coronavirus disease 2019 is critical since treatment varies based on etiology: Let us not forget critical illness-related corticosteroid insufficiency as the treatment is very different and often lifesaving! Crit Care Med. 2021;49(7):e724-5. https://pubmed.ncbi.nlm.nih.gov/33870921. https://doi.org/10.1097/CCM.0000000000005006.
Bateman A, Singh A, Kral T, Solomon S. The immune-hypothalamic-pituitary- adrenal axis. Endocr Rev. 1989;10(1):92–112. https://pubmed.ncbi.nlm.nih.gov/2666113. https://doi.org/10.1210/edrv-10-1-92.
Soni A, Pepper GM, Wyrwinski PM, et al. Adrenal insufficiency occurring during septic shock: Incidence, outcome, and relationship to peripheral cytokine levels. Am J Med. 1995; 98(3):266–71. https://pubmed.ncbi.nlm.nih.gov/7872343. https://doi.org/10.1016/S0002-9343(99)80373-8.
Natarajan R, Ploszaj S, Horton R, Nadler J. Tumor necrosis factor and interleukin-1 are potent inhibitors of angiotensin-II-induced aldosterone synthesis. Endocrinology. 1989;125(6):3084–9. https://pubmed.ncbi.nlm.nih.gov/2555138. https://doi.org/10.1210/endo-125-6-3084.
Siejka A, Barabutis N. Adrenal insufficiency in the COVID-19 era. Am J Physiol Endocrinol Metab. 2021 Apr 1;320(4):E784-5. https://pubmed.ncbi.nlm.nih.gov/33825496. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8057305. https://doi.org/10.1152/ajpendo.00061.2021.
Prescott HC, Rice TW. Corticosteroids in COVID-19 ARDS: Evidence and hope during the pandemic. JAMA. 2020;324(13):1292–5. https://pubmed.ncbi.nlm.nih.gov/32876693, https://doi.org/10.1001/jama.2020.16747.
Isidori AM, Pofi R, Hasenmajer V, Lenzi A, Pivonello R. Use of glucocorticoids in patients with adrenal insufficiency and COVID-19 infection. Lancet Diabetes Endocrinol. 2020;8(6):472-3. https://pubmed.ncbi.nlm.nih.gov/32334645. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7180011. https://doi.org/10.1016/S2213-8587(20)30149-2.
Angus DC, Derde L, Al-Beidh F, et al. Effect of hydrocortisone on mortality and organ support in patients with severe COVID-19: The REMAP-CAP COVID-19 corticosteroid domain randomized clinical trial. JAMA. 2020;324(13):1317-29. https://pubmed.ncbi.nlm.nih.gov/32876697. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7489418. https://doi.org/10.1001/jama.2020.17022.
Liu L, Li J, Huang YZ, et al. [The effect of stress dose glucocorticoid on patients with acute respiratory distress syndrome combined with critical illness-related corticosteroid insufficiency]. Zhonghua Nei Ke Za Zhi. 2012;51(8):599-603. https://pubmed.ncbi.nlm.nih.gov/23158856.
Alhazzani W, Møller MH, Arabi YM, et al. Surviving sepsis campaign: Guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Crit Care Med. 2020; 48(6):e440–69. https://pubmed.ncbi.nlm.nih.gov/32224769. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7176264. https://doi.org/10.1097/CCM.0000000000004363.
Ritter LA, Britton N, Heil EL, Teeter WA, Murthi SB, Chow JH, et al. The impact of corticosteroids on secondary infection and mortality in critically ill COVID-19 patients. Journal of Intensive Care Medicine. 2021;36(10):1201-8. https://pubmed.ncbi.nlm.nih.gov/34247526. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8442131. https://doi.org10.1177/08850666211032175
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Anna Elvira Arcellana, Kenneth Wilson Lim, Marlon Arcegono, Cecilia Jimeno

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The full license is at this link: http://creativecommons.org/licenses/by-nc/3.0/legalcode).
To obtain permission to translate/reproduce or download articles or use images FOR COMMERCIAL REUSE/BUSINESS PURPOSES from the Journal of the ASEAN Federation of Endocrine Societies, kindly fill in the Permission Request for Use of Copyrighted Material and return as PDF file to jafes@asia.com or jafes.editor@gmail.com.
A written agreement shall be emailed to the requester should permission be granted.










